Introducción: La dispepsia funcional (DF), según Roma III, se clasifica en síndrome de distrés posprandial (SDP) y síndrome de dolor epigástrico (SDE). El test de saciedad (TS) se utilizó previamente para evaluar la acomodación y el vaciamiento gástrico, y permitió diferenciar individuos sanos de dispépticos.
Objetivos: 1) Estimar si el TS permite diferenciar a individuos dispépticos de sanos, y 2) evaluar si es útil para diferenciar ambos subtipos de DF.
Métodos: Estudio transversal. Se incluyó consecutivamente a adultos con DF y controles sanos entre agosto del 2011 y octubre del 2012. El TS consistió en la ingesta de un suplemento nutricional (Fortisip®, Nutricia Bagó®) a velocidad constante; la saciedad se calificó cada 5 min (1a 5 puntos). La ingesta se suspendió cuando se reportó puntaje máximo. Se registraron el volumen y las calorías totales ingeridos. Análisis estadístico: test Mann-Whitney.
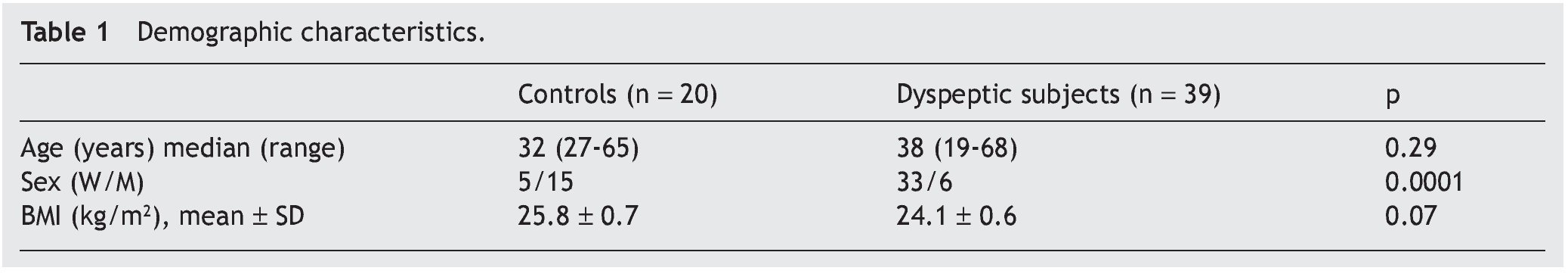
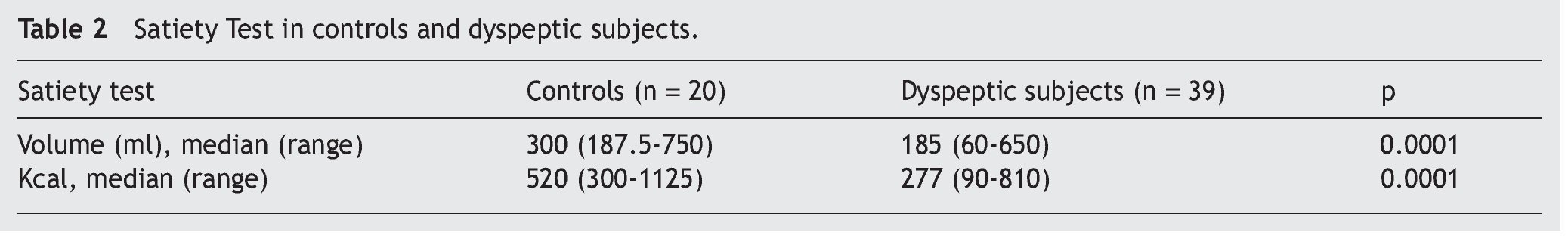
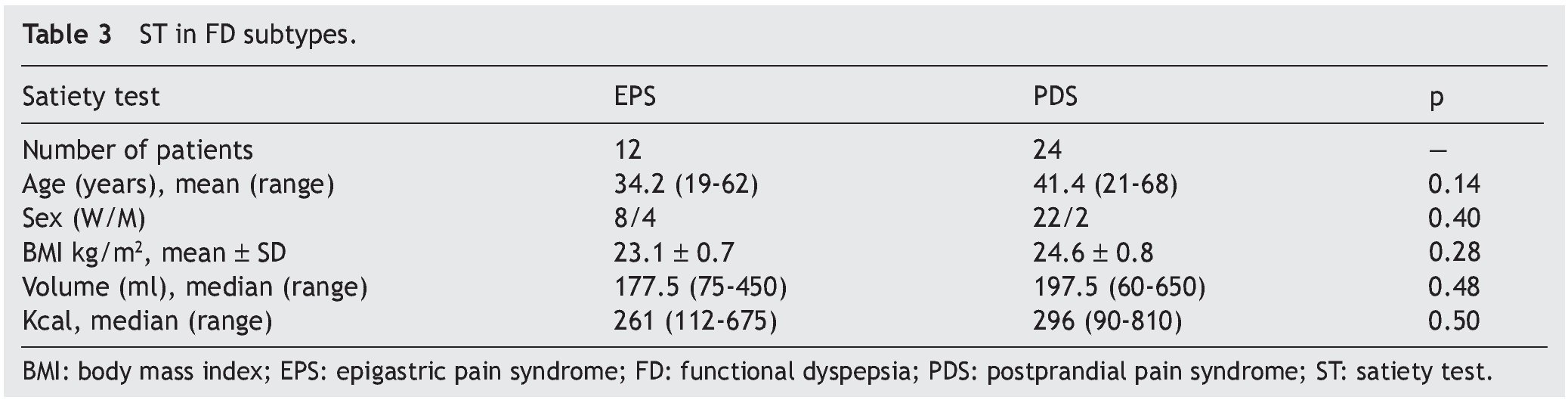
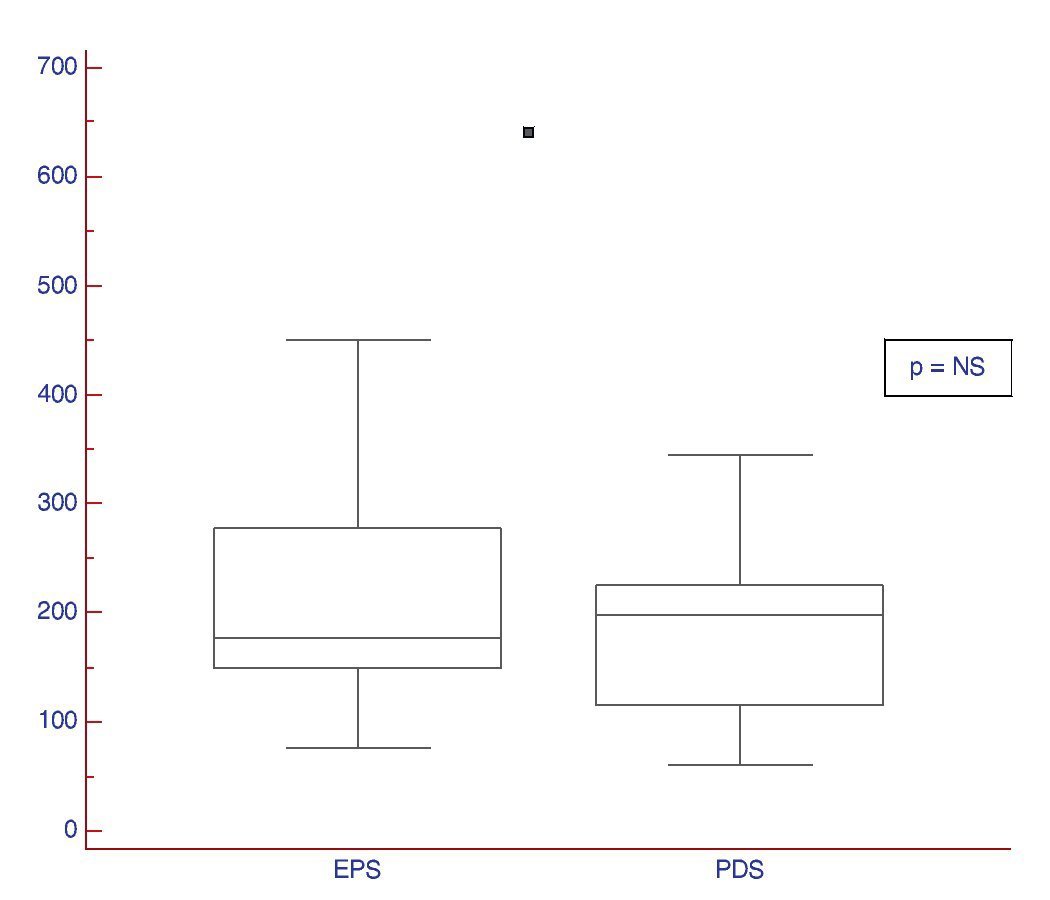
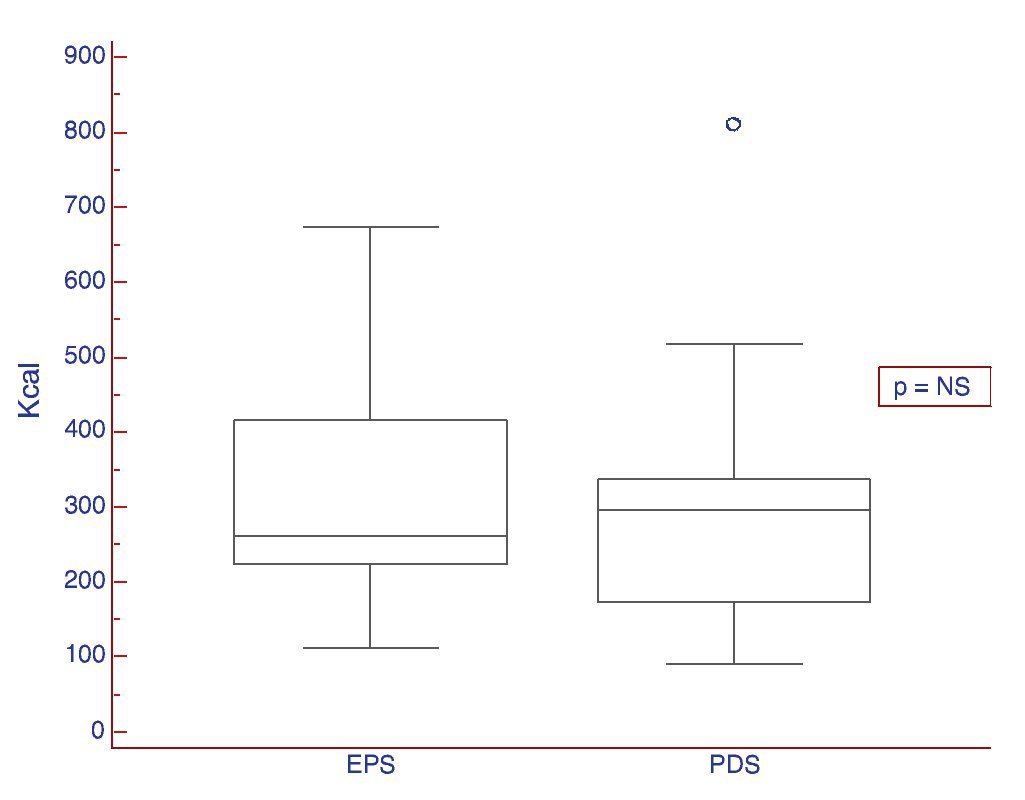
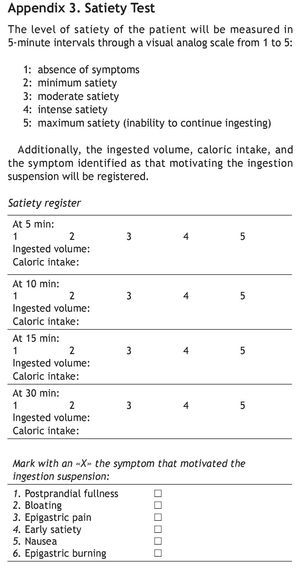
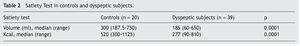
Resultados: Se incluyó a 39 dispépticos y 20 controles. Los pacientes fueron predominantemente mujeres (84.6 vs. 25%; p < 0.0001) y similares en edad (39.59 ± 13.53 vs. 34.70 ± 9.85 años) e índice de masa corporal (24.32 ± 3.52 vs. 25.82 ± 3.34 kg/m2) respecto de los controles. Subtipos de DF: SDP: 61%, SDE 31% y síndrome mixto: 8%. 1) Los dispépticos toleraron menor volumen y calorías (185 vs. 300 ml y 277 vs. 520 Kcal, respectivamente p < 0.001), y 2) no se observaron diferencias en el TS entre ambos subtipos puros de dispepsia.
Conclusiones: El TS fue diferente entre individuos sanos y dispépticos, aunque presentó similar volumen y calorías en ambos subtipos de DF.
Introduction: According to the Rome III Criteria, functional dyspepsia (FD) is classified as post-prandial distress syndrome (PDS) and epigastric pain syndrome (EPS). On the other hand, the satiety test (ST) has been used to evaluate gastric accommodation and emptying, distinguishing healthy individuals from those with dyspepsia.
Aims: To determine whether the ST can distinguish dyspeptic individuals from healthy ones and to evaluate its usefulness in differentiating the two FD subtypes.
Methods: Adults with FD were consecutively enrolled in a cross-sectional study within the timeframe of August 2011 and October 2012. Healthy subjects participated as controls. The ST consisted of the intake of a nutritional supplement (Fortisip®, Nutricia Bagó®) at a constant speed; satiety was graded at 5-minute intervals (1 to 5 points). Intake was suspended when the maximum score was reported. The total ingested volume and caloric intake was recorded and the Mann-Whitney U test was used in the statistical analysis.
Results: The study included 39 dyspeptic patients and 20 control individuals. The patients were predominantly women (84.6 vs. 25%; p < 0.0001) and they were similar in age (39.59 ± 13.53 vs. 34.70 ± 9.85 years) and BMI (24.32 ± 3.52 vs. 25.82 ± 3.34 kg/m2) with respect to the controls. The FD subtype percentages were PDS: 61%, EPS: 31%, and Mixed syndrome: 8%. There was a lower ingested volume and caloric intake on the part of the dyspeptic patients (185 vs. 300 ml and 277 vs. 520 Kcal, respectively. Both: P<.001). No differences in the ST were observed between the two pure dyspepsia subtypes.
Conclusions: There was a difference in the ST between healthy individuals and those with dyspepsia, but the ingested volume and caloric intake in the two FD subtypes were similar.
Introduction
Dyspepsia, whose etymologic meaning refers to poor digestion, is a condition with a symptomatology that is common in the general population. It represents 2-3% of the medical consultations in general practice and 40% of those to gastroenterologists.1 However, only one fourth of the patients with dyspepsia consult a physician. Epidemiologic studies based on clinical practice have a clear selection bias, and the most representative are the population studies.2 An epidemiologic study evaluating "non-studied" dyspepsia in a population sample in Argentina reported a prevalence of 29.6%.3
There are 2 main pathophysiologic alterations in functional dyspepsia (FD): a) motor abnormalities of the proximal digestive tract (motility alterations) and b) sensory visceral dysfunction (sensory perception alterations).4
Many patients with FD have an antral motor dysfunction or a delay in gastric emptying, but it has not been possible to show a correlation between symptoms and this abnormality.5
A subgroup of patients that present with symptoms of early satiety and weight loss, has gastric accommodation alterations. This appears to be a very important manifestation, due to the fact that it finally demonstrates some kind of correlation between certain types of symptoms and an identified pathophysiologic alteration.6
Visceral sensory alteration (the capacity to perceive or not perceive what is happening within the digestive tract)7 is another important pathophysiologic aspect because this pathophysiologic mechanism of hypersensitivity is linked to epigastric pain, burping, and weight loss. Stress and anxiety modify sensory perception and they cause subjects to present with high levels of anxiety, depression, hypervigilance, and multiorgan somatic complaints.
Since the early 1990s, digestive function pathology has been classified according to the Rome Criteria. The current guidelines are those of the Rome III Criteria8 that recommend differentiating between patients with epigastric pain and those with postprandial distress, identified as distinct pathophysiologic subgroups. 9 This subclassification is based on the main symptoms of pain or intermittent burning sensation localized in the epigastrium of at least average intensity presenting for a minimum of once a week, and postprandial fullness that occurs after a normal-sized meal various times a week. The criteria must be met during the last 3 months and the symptoms must have begun a minimum of 6 months before diagnosis. The 2 subtypes can coexist.
The exact etiopathogenic mechanism that causes the symptoms in an individual patient is still difficult to identify. Therefore, up to the present, clinical manifestations are the most effective diagnostic method and they determine the treatment strategy. The so-called satiety test (ST) is a recently described functional exploration of the digestive tract that enables the objective measurement of early satiety, a symptom observed in an important number of patients with FD.10 This simple, non-invasive test appears to hold an important place among the techniques used in the study of the pathophysiology of the motor and functional disorders of the stomach. It was originally designed for evaluating gastric symptoms during the intake of a liquid food, as a continuous and slow infusion, until reaching the level of maximum satiety. The test measured satiety by grading the volume of the ingested liquid on a Linkert scale of 0 to 5, with 5 being the highest score. A validation study conducted on a group of patients with FD suggested that the low caloric content test was correlated with the severity of early satiety symptoms and was potentially useful in assessing gastric accommodation.11
Likewise, there is evidence that the ST enabled the differentiation between healthy individuals and those presenting with dyspepsia in European5,9 and North and Central American populations.12 Such a study has not been conducted in Mexico and therefore we wish to evaluate this distinction in the Mexican population.
Our working hypothesis was that the ST is a diagnostic method that would enable the differentiation between the 2 dyspepsia subtypes, postprandial distress syndrome (PDS) or epigastric pain syndrome (EPS), thus managing the therapy with greater precision.13
Aims
1. To evaluate whether there was a difference in the ST (ingested volume and caloric intake) between healthy individuals and those presenting with dyspepsia.
2. To analyze the usefulness of the ST in differentiating between the 2 dyspepsia subtypes (PDS or EPS).
Methods
Study population
Adults of both sexes ≥ 18 years of age diagnosed with FD according to the Rome III Criteria that signed statements of informed consent were included in the study. The exclusion criteria were: evidence of organic disease through laboratory tests, upper digestive and/or abdominal endoscopy, the use of prokinetic agents, calcium blockers, anti-depressives, opioid analgesics, nonsteroidal anti-inflammatory drugs or iron supplements, known systemic disease altering motility, hydroelectric disorders, a past history of upper digestive tract surgeries, pregnancy or lactation, dementia or inability to follow the protocol, and a history of alcohol and/or illegal drug abuse.
Controls
Twenty healthy volunteers that did not fit any of the Rome III Criteria for FD, that reported no personal history of digestive diseases, and that were not taking any concomitant medication for digestive disorders were recruited as controls.
Consecutive recruitment was carried out within the time frame of August 2011 to September 2012 at the Hospital de Gastroenterología in Buenos Aires, Argentina.
Study design
An exploratory, comparative, prospective, and cross-sectional study was conducted.
Procedures
Symptom questionnaire
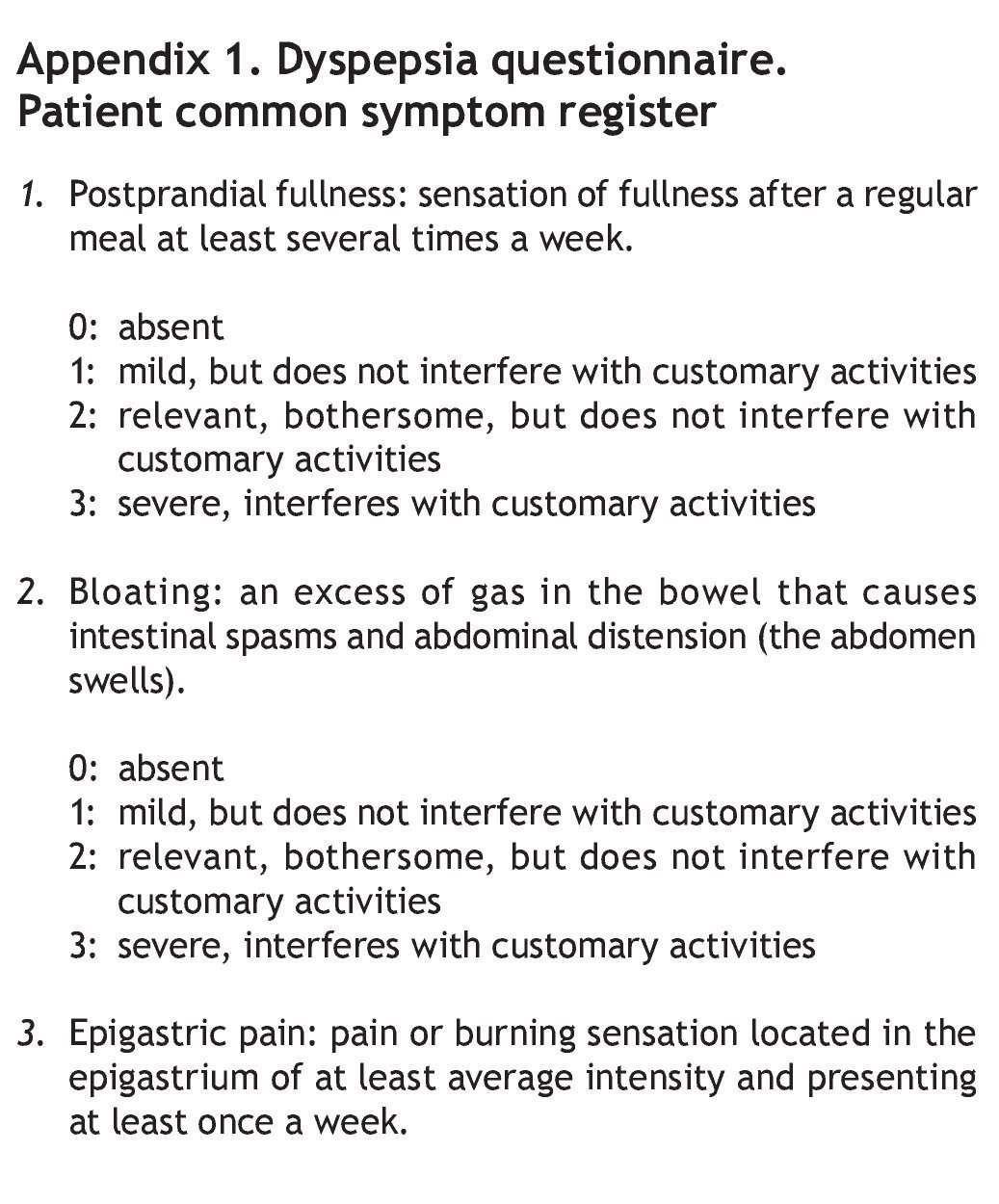
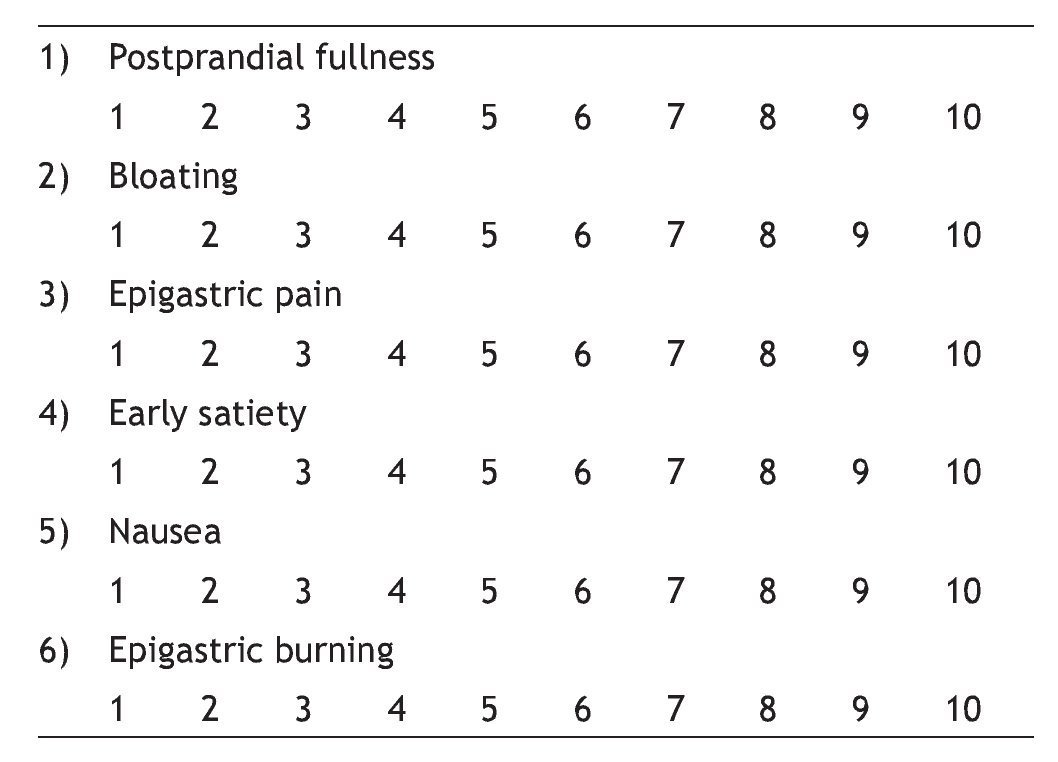
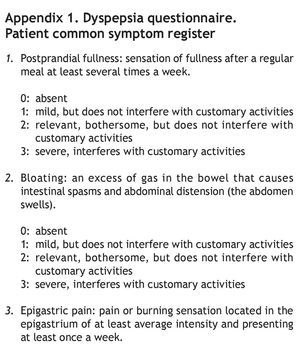
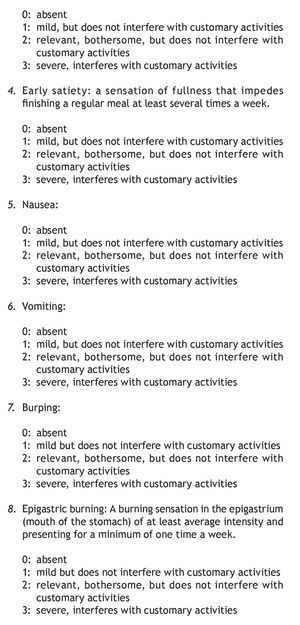
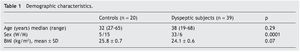
Before the ST was performed, each patient was classified according to the dyspepsia subtype and the severity of the common symptoms through the reproducible dyspepsia questionnaire employed by Tack and Cuomo in 1998 and 2001, respectively5,14 (appendix 1).
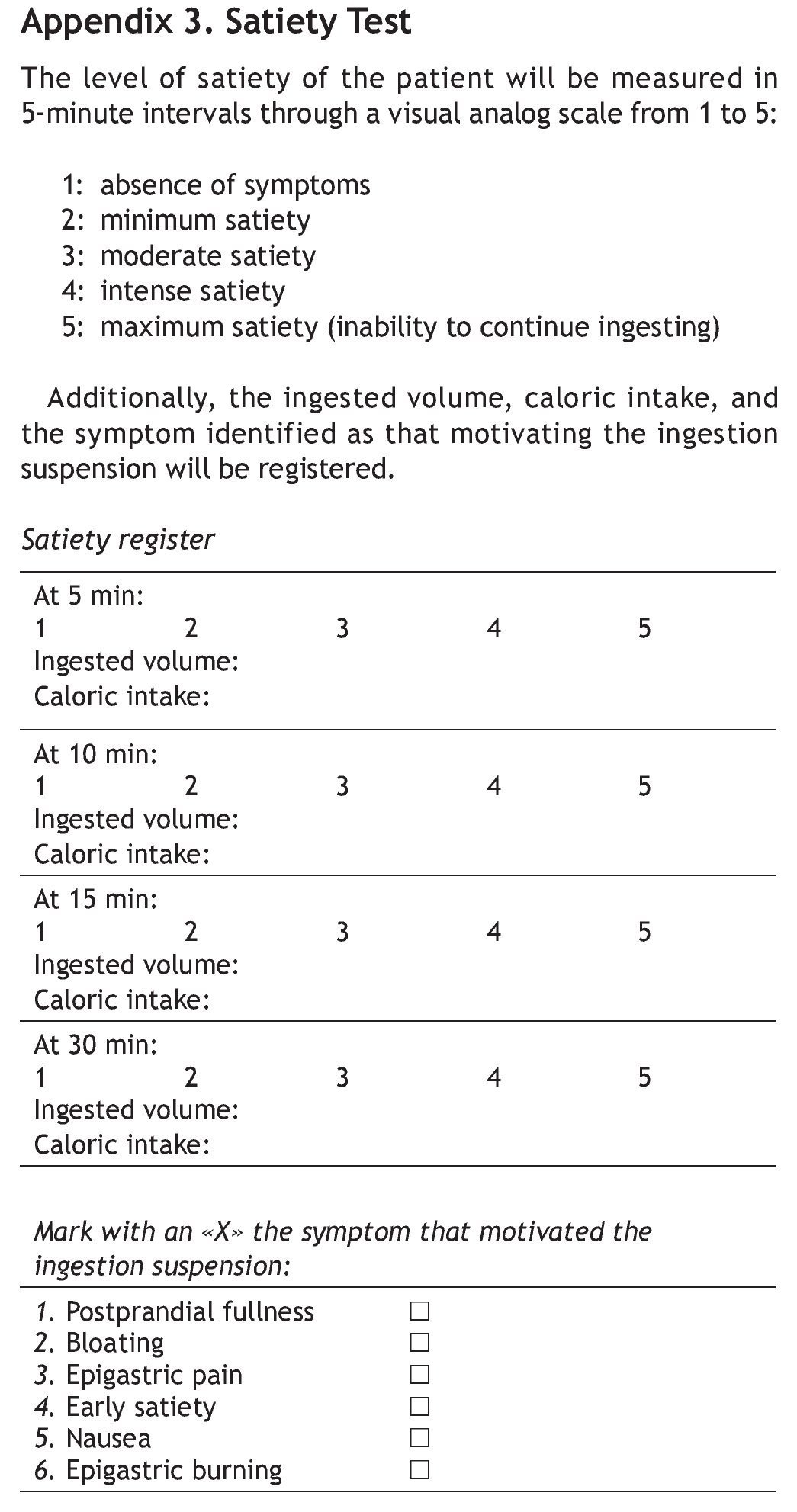
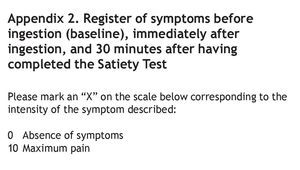
The ST was subsequently carried out, recording the appearance and severity of symptoms before (baseline determination) and immediately after ingestion, and then 30 min after having completed the test (appendix 2).
Satiety Test
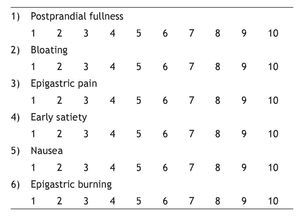
After a fasting period of 12 h, the subjects ingested a nutritional supplement (a semi-liquid foodstuff of a known and standardized composition: Fortisip, Nutricia Bagó®). It was free of both fiber and lactose and had a balanced content of carbohydrates (49%), proteins (16%), and lipids (36%). It was ingested at a constant speed (15 ml/min) until reaching maximum satiety (the sensation of gastric fullness that inhibits the desire to continue drinking or eating). Kcal intake was determined when the patient reached maximum satiety, in other words, when the patient stated «I can't drink another drop». This was registered in the questionnaire that was applied at 5-min intervals (appendix 3).
Antacid intake on demand as rescue medication was permitted one week prior to the study.
Measurement results:
1. Satiety in healthy individuals and in those presenting with dyspepsia: the ingested volume/caloric intake at the appearance of the symptom of maximum satiety was recorded to evaluate whether there was a difference between the two groups. When the test was performed, the ingested volume and caloric intake were registered at the instant the symptom of "maximum satiety" appeared, along with any eventual concomitant symptoms.
2. Usefulness of the test for differentiating between the two types of dyspepsia: the existence or not, of differences in the ingested volume and caloric intake between the two dyspepsia subtypes was evaluated. Dyspepsia subtype diagnosis was made according to the type and severity of the predominant symptom after the test:
º PDS:
— Postprandial fullness: the sensation of fullness after a regular meal at least several times a week.
— Early satiety: the sensation of fullness that impedes finishing a regular meal at least several times a week.
º EPS:
— Pain or burning sensation in the epigastrium of at least average intensity minimum of once a week.
º Mixed Syndrome.
Statistical analysis
The information was processed using MedCalc version 11.2.1.0 and the data were reported as means ± standard deviation. The results of the different groups were compared using the corresponding chi-square test or the Fisher exact test for the qualitative values and the corresponding Student's t test or Mann-Whitney test for the quantitative variables, according to normal or non-parametric distribution, respectively. Statistical significance was considered when there was a p < 0.05.
Because the study was an exploratory one, sample size was established at a minimum of 30 patients presenting with dyspepsia.
Ethical safeguards
The patients signed statements of informed consent and the study protocol was approved by the Bioethics Committee of the Hospital de Gastroenterología "Dr. Carlos Bonorino Udaondo".
Results
Description of the sample
Thirty-nine patients and controls were enrolled in the study; the characteristics of both the dyspeptic patients and the controls are described in Table 1. The FD subtypes were categorized according to the Rome III Criteria and the most frequent subtypes, in descending order, were: PDS: 61% (24/39), EPS: 31% (12/39), and Mixed: 8% (3/39).
Results
1. The comparison of the ingested volume and caloric intake between the dyspeptic patients and the controls showed that there was a statistically significant lower volume and caloric intake in the ST of the patients with dyspepsia (p < 0.001) (Table 2).
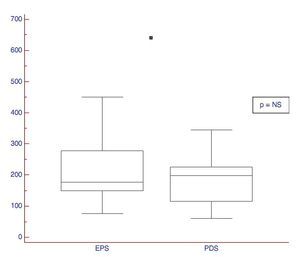
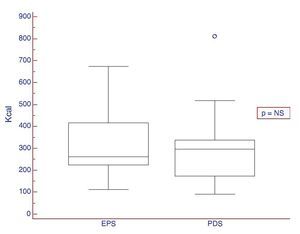
2. Usefulness of the test in differentiating between the two types of dyspepsia: the existence or not, of differences in the ST in patients with pure PDS and EPS was evaluated. The patients with mixed syndromes (n=3) were excluded from this analysis. No statistically significant differences were observed between the two dyspepsia subtypes (Figs. 1 and 2 and Table 3).
Figure 1. ST results expressed in volume in patients presenting with the dyspepsia subtypes: PDS and EPS.
Figure 2. ST results expressed in Kcal in patients presenting with dyspepsia subtypes: PDS and EPS.
The most frequent symptoms accompanying ingestion suspension, according to the dyspepsia subtype, are described as follows:
— PDS: postprandial fullness 50% (12/24), early satiety and nausea —individually— 16% (4/24), bloating and epigastric pain 8.33% (2/24).
— EPS: postprandial fullness 50% (6/12), nausea 25% (3/12), epigastric pain and nausea —together— 25% (3/12).
Discussion
Different organic diseases can cause symptoms that are consistent with dyspepsia. This disorder is common and usually has a benign cause. Current recommendations suggest that young patients < 45 years of age, with no alarm symptoms or risk factors for gastric disease can be treated empirically with anti-secretors or prokinetics for 4 weeks, after which the response is evaluated. The patients that continue to present with symptoms despite this strategy, or those > 45 years of age, should undergo endoscopic evaluation.15
FD is defined by the Rome III Criteria and subclassified into EPS and PDS; symptoms should be present during the last 3 months and have begun at least 6 months prior to diagnosis. Symptoms are nonspecific and the pathophysiology is diverse, which is why an effective universal treatment is still the subject of research.16,17
Dyspepsia evaluation includes upper digestive tract video-endoscopy, scintigraphy study of gastric emptying, breath test, ultrasound or nuclear magnetic resonance (NMR) imaging, and evaluation of a gastric accommodation through NMR, PET, or barostat.
Other more specific studies that evaluate motor function alterations include antro-duodenal-jejunal manometry that is used to record the myoelectric activity of the stomach; the barostat and satiety test are used for evaluating visceral sensitivity.18
The pathophysiologic mechanisms described in FD include motor abnormalities such as emptying and/or gastric accommodation disorders and visceral sensitivity dysfunction of unexplained clinical significance.19 Likewise, the lack of sensitivity and specificity of defined symptomatic patterns for identifying the respective pathophysiologic alteration, together with the fact that the tests for evaluating these disorders are invasive, laborious, and occasionally associated with radiation exposure, make the management of some of these patients difficult.20
The ST has been developed as a non-invasive method for evaluating gastric accommodation in healthy individuals and in those presenting with dyspepsia.11,21 These tests are easily performed without specific instruments and are well-tolerated; however, their sensitivity and specificity vary depending on the ingested substance used (water or nutritional supplement), the method of comparison employed for greater diagnostic performance (ultrasonography or scintigraphy), and the technique used for carrying out the test.14,22,23
Studies conducted on volunteers without dyspepsia that correlated the ST with the barostat showed the former to be useful in evaluating accommodation and the threshold for inducing severe discomfort. Nevertheless, the correlation between the ingested volume and the accommodation volume measured by the barostat is controversial.24-26
Tack et al. observed that patients with FD tolerated fewer volumes than healthy individuals and that the ingested volume, at different caloric densities, was the major determinant of gastric accommodation to a meal.10
Cuomo et al. analyzed symptom severity through a reproducible questionnaire that correlated the ST parameters with gastric emptying and dyspeptic symptoms and concluded that the ST was able to objectively measure satiety and relate it to symptom severity. The study also showed an indirect correlation between early satiety severity measured by the ST and gastric emptying, as well as an association between flatulence and delayed gastric emptying.9
Boeckxstaens et al. evaluated dyspeptic symptoms with the ST employing water and a nutritional supplement (Nutridrink) and observed that the FD patients reported more severe and persistent symptoms during the ST than the controls. In addition, the patients underwent the barostat study and were pathophysiologically classified as individuals with normal physiology, visceral hypersensitivity, and accommodation alterations. The symptoms triggered by the ST were not influenced by the results of the barostat study.27
Our results coincided with those previously reported, confirming the fact that healthy individuals can be distinguished from those with dyspepsia through the ST. To the best of our knowledge, there are currently no studies having evaluated the ST and the FD subtypes. In 2010, Kato et al. conducted a study utilizing the ST with water in order to differentiate distinct pathophysiologic mechanisms, but they did not include the clinical subtypes. Therefore, our study is the first to distinguish the clinical subtypes of FD through the ST.
Conclusions
According to our results, we can conclude that the ST was different between healthy individuals and patients presenting with dyspepsia, even though the ingested volume and caloric intake was similar in patients with PDS and EPS.
There is presently no scientific evidence at hand for recommending different alimentary instruction for these patients, and so clinical parameters continue to be the available tools for selecting the best-tolerated foods.
The reproducibility of this study with a greater number of patients would be useful for confirming our results.
Financial disclosure
No financial support was received in relation to this article.
Conflict of interests
The authors declare that there is no conflict of interest.
Received 6 February 2013;
accepted 21 June 2013
* Corresponding author at:
Av. Caseros 2061 (1264); Buenos Aires, Argentina.
Tel.: 54 11 43064641- INT 129.
E-mail address: carolinabolino@gedyt.com.ar (M.C. Bolino).