Gastric adenocarcinoma is among the high-ranking tumors, with respect to frequency and mortality, worldwide. The inflammatory process and immune system activity are associated with oncologic control. Our aim was to identify whether the neutrophil-to-lymphocyte ratio (NLR), platelet-to-lymphocyte ratio (PLR), and other variables are prognostic factors for survival in patients with metastatic gastric cancer in a Mexican population.
Material and methodsPatients diagnosed with metastatic gastric adenocarcinoma, hospitalized within the time frame of December 2011 to 2021, were analyzed. The NLR, PLR, and albumin and hemoglobin levels obtained from blood samples were calculated. Functional status (ECOG and Karnofsky), sex, histology, and the presence of signet ring cells were also considered possible prognostic factors. Each factor’s prognostic value for overall survival was determined through univariate and multivariate analyses.
ResultsThe study included 956 patients diagnosed with metastatic gastric cancer, of whom 494 (51.7%) were men and 462 (48.3%) were women. The main histologic finding was diffuse adenocarcinoma (n = 619, 64.7%), followed by intestinal adenocarcinoma (n = 293, 30.6%), and the presence of signet ring cells was found in 659 (68.9%) patients. Diagnostic laparoscopy was performed on 238 patients (24.9%) to confirm peritoneal carcinomatosis. The multivariate analysis showed that an NLR above 3.2 (HR 1.51, 95% CI 1.27–1.8; p < 0.001), albumin below 3.5 g/dl (HR 1.25, CI 1.06–1.47; p = 0.006), and an ECOG performance status of 2 or higher (HR 1.39, CI 1.10–1.76; p = 0.005) were independent factors that predicted a lower survival rate, whereas a Karnofsky score above 70% (HR 0.69, CI 0.53–0.91; p = 0.008) was associated with a better survival rate. Lastly, the PLR was not statistically significant in the multivariate analysis.
ConclusionsThe NLR, nutritional status assessed through albumin measurement, and functional status can act as independent prognostic survival factors in hospitalized Mexican patients diagnosed with metastatic gastric adenocarcinoma and be taken into account during therapeutic decision-making.
El adenocarcinoma gástrico se ubica entre las neoplasias malignas con mayor frecuencia y mortalidad en el mundo. Se ha observado que el proceso inflamatorio y la actividad del sistema inmunológico están asociados al control oncológico. Nuestro objetivo es identificar si el índice neutrófilo/linfocito (INL), índice plaqueta/linfocito (IPL) y otros factores son pronósticos para supervivencia en pacientes con cáncer gástrico metastásico en nuestra población.
Material y métodosPacientes con diagnóstico de adenocarcinoma gástrico metastásico, admitidos de diciembre 2011 a 2021. A partir de una muestra de sangre al ingreso se calculó el INL, IPL, albumina y hemoglobina. Además, se consideró el estado funcional (ECOG y Karnofsky), sexo, histología y presencia de células en anillo de sello como otros factores que pudieran ser pronósticos. Por medio de un análisis univariado y multivariado se determinó el valor pronóstico de cada factor para supervivencia global.
ResultadosSe incluyeron 956 pacientes con diagnóstico de cáncer gástrico metastásico, 494 (51.7%) fueron hombres y 462 (48.3%) mujeres, la principal histología fue el adenocarcinoma difuso 619 (64.7%) seguido por adenocarcinoma intestinal 293 (30.6%) y del total de pacientes, 659 (68.9%) tuvieron presencia de células en anillo de sello. En 238 pacientes (24.9%) se realizó laparoscopia diagnóstica para confirmar la carcinomatosis peritoneal. El análisis multivariado demostró que un INL mayor a 3.2 (HR 1.51, IC 95% 1.27-1.8; p < 0.001), albumina menor a 3.5 g/dl (HR 1.25, IC 1.06 - 1.47; p = 0.006) y un ECOG de 2 o mayor (HR 1.39, IC 1.10-1.76; p = 0.005) fueron factores independientes que predijeron una menor supervivencia mientras que el Karnofsky mayor a 70% (HR 0.69, IC 0.53-0.91; p = 0.008) se asoció a mejor supervivencia y finalmente, el IPL no tuvo significancia estadística para este análisis.
ConclusionesEl INL, el estado nutricional midiendo la albúmina y el estado funcional pueden ser factores independientes pronósticos de supervivencia en pacientes mexicanos que ingresan con diagnóstico de adenocarcinoma gástrico metastásico y pudieran ser considerados durante la toma de decisiones terapéuticas.
Gastric adenocarcinoma ranks among the first 5 tumors in incidence and mortality worldwide.1 Early-stage tumors have the best prognosis, with a 5-year survival above 95% observed in countries with a well-established screening program, such as Japan and Korea.2 In the rest of the world, including Mexico, gastric cancer is diagnosed at advanced stages, with a negative impact on survival. Systemic treatment is a standard and surgery is relegated to palliative treatment. There is a group of patients with metastatic disease that are not candidates for systemic treatment due to their poor functional status, organ dysfunction, or malnutrition, or the fact that treatment would deteriorate their quality of life without providing any benefits, and so they can only be offered better medical support through palliative care.3 More prognostic factors should be looked for to aid us in better selecting patients for receiving treatment and in providing better medical support in a timely manner, when treatment is not an option.
Several studies have shown that the immune system influences the natural history of cancer, and that neutrophils, lymphocytes, monocytes, and platelets induce the inflammatory response through the production of cytokines and proinflammatory factors that induce damage in cellular DNA, inhibiting apoptosis, and in turn, favoring tumor progression and metastasis.4 One of the most widely studied biomarkers is the neutrophil-to-lymphocyte ratio (NLR), which reflects the balance between proinflammatory cell status and the humoral antitumor immune system. Murakami et al. conducted a retrospective analysis on 92 patients with unresectable gastric cancer, establishing an NLR of 2.83 as the cutoff point, and found that the group of patients with an NLR above that value had poorer survival.5 In a meta-analysis, an elevated NLR was shown to be related to more advanced clinical disease stages, with lower survival rates and shorter disease-free periods. NLR determination, together with other variables, such as sex, age, and clinical stage, increases prognostic power.6 In addition, the usefulness of the NLR as a predictive factor of systemic treatment response has been proposed, finding that an increase in NLR after the first cycle of chemotherapy predicts a poor response.7
The platelet-to-lymphocyte ratio (PLR) is another biomarker that has been studied in gastric cancer, but results have been less consistent, as well as controversial. The same as with the NLR, no cutoff point has been defined for the PLR in the wide range of studies conducted. In a meta-analysis by Zhan et al., they chose a cutoff point of 150 and carried out subgroup analyses, finding that a PLR above 150 was associated with poorer overall survival and a shorter disease-free period, especially in patients that underwent surgical treatment. They also found that patients with tumors invading the serosa of the stomach (T3/T4), metastasis to the lymph nodes, and more advanced stages (III and IV) had an elevated PLR. Lastly, the PLR was not associated with the grade of tumor differentiation, tumor size, or tumor location.8
Anemia is frequent in advanced stages of gastric cancer. The decrease in hemoglobin is accompanied by a decline in functional status, and in several studies, has been described as a prognostic factor that should be corrected before starting treatments, given that tumor hypoxia increases resistance to chemotherapy, reducing its effectiveness.9
Evaluating nutritional status is vitally important because it influences patient progression, altering wound healing mechanisms in patients that have been operated on. It also impacts the bioavailability of medications, and very importantly, alters the response of the immune system against cancer. Studies utilizing albumin as a biomarker have reported that low levels of the protein are associated with worse oncologic outcomes.10
Finally, the functional status of all oncologic patients should be determined, utilizing scales that can measure the physical capacity of patients that are going to receive treatment. A poor functional status is one of the main contraindications for receiving palliative systemic or surgical treatments in patients with metastatic gastric cancer, making it an important prognostic factor.
The primary aim of the present retrospective review was to identify whether the variables of NLR, PLR, hemoglobin, albumin, functional status, sex, histology, and the presence of signet ring cells were independent prognostic factors for survival in patients diagnosed with metastatic gastric adenocarcinoma admitted to our hospital.
Material and methodsA retrospective, observational, cross-sectional study was conducted that included patients above 18 years of age diagnosed with metastatic gastric adenocarcinoma (clinical stage IVb, according to the AJCC-2018) admitted to our hospital within the time frame of December 2011 and 2021. Clinical staging was determined through panendoscopy and computed axial tomography, and when those studies could not confirm peritoneal carcinomatosis, diagnostic laparoscopy was performed. Patients with incomplete medical records in whom clinical stage could not be determined and patients with esophagogastric tumors and/or tumors extending into the esophagus were excluded from the study. The first complete blood count registered upon hospital admission was utilized to calculate the NLR and PLR and hemoglobin levels in the patients.
Statistical analysisDescriptive statistics were carried out (after the Kolmogorov-Smirnov normality test). The quantitative variables were expressed through median and interquartile range (IQR) between the 25th and 75th percentiles, and the qualitative variables through counts and percentages. The variables were compared using the Student’s t test for the numerical variables and the chi-square test for the qualitative variables. For the variables of interest, comparative groups were formed based on cutoff points in receiver operating characteristic (ROC) curves, when the characteristics of the curve showed predictive power; otherwise, the median was used. Thus, the median was utilized for the NLR, PLR, and the ROC curve for hemoglobin; a level <3.5 g/dl of albumin in the first blood sample of the patient was considered malnutrition. Functional status was calculated utilizing the Eastern Cooperative Oncological Group performance status (ECOG PS) scale and the Karnofsky score, with a score >2 and <70%, respectively, as poor functional status. Survival was compared between groups, using the Kaplan-Meier method with the log-rank test. Lastly, the multivariate analysis was performed with the COX regression to determine the prognostic value of the independent factors for survival and the variables that showed a trend or statistical significance in the univariate model were introduced into the multivariate model (p < 0.10). Statistical significance was set at a p < 0.05.
Ethical considerationsThis is a retrospective, nonexperimental study that does not require informed consent. All ethics protocols of our hospital for carrying out published works have been followed. The personal data of all patients has been maintained anonymously and each patient’s right to privacy has been respected.
ResultsA total of 956 patients were included in the study, of whom 494 (51.7%) were men and 462 (48.3%) were women. Mean patient age was 54 years (IQR 44–64). The main histologic finding was diffuse adenocarcinoma (619; 64.7%), followed by intestinal adenocarcinoma (293; 30.6%) and mixed adenocarcinoma (44; 4.6%). Signet ring cells were present in 659 (68.9%) patients. Table 1 shows the rest of the demographic characteristics of our study population. Diagnostic laparoscopy was performed on 238 (24.9%) patients, confirming peritoneal carcinomatosis, and imaging studies were carried out on the 718 (75%) remaining patients, identifying solid organ metastasis and/or peritoneal carcinomatosis. Utilizing the median, the cutoff points were 3.2 (IQR 2.1–5.07) for the NLR and 226 (IQR 156.7–330.8) for the PLR. Regarding hemoglobin, the area under the curve (AUC) was 0.56, with 10 g/dl as the best cutoff point.
Patient demographic characteristics.
| Variable | n = 956 |
|---|---|
| Sex, n (%) | |
| Men | 494 (51.7%) |
| Women | 462 (48.3%) |
| Age in years, median (IQR) | 54 (44–64) |
| Histology, n (%) | |
| Diffuse adenocarcinoma | 619 (64.7%) |
| Intestinal adenocarcinoma | 293 (30.6%) |
| Mixed adenocarcinoma | 44 (4.6%) |
| Signet ring cells, n (%) | |
| Absent | 297 (31.1%) |
| Present | 659 (68.9%) |
| Diagnostic laparoscopy, n (%) | |
| No | 718 (75.1%) |
| Yes | 238 (24.9%) |
| NLR, n (%) | |
| <3.2 | 478 (50%) |
| ≥3.2 | 478 (50%) |
| PLR, n (%) | |
| <226 | 477(49.9%) |
| ≥226 | 479 (50.1%) |
| Hemoglobin (g/dl), n (%) | |
| <10 | 254 (26.6%) |
| ≥10 | 702 (73.4%) |
| Albumin (g/dl), n (%) | |
| ≥3.5 | 538 (56.3%) |
| <3.5 | 418 (43.7%) |
| ECOG PS, n (%) | |
| 0–1 | 698 (73%) |
| >2 | 258 (27%) |
| Karnofsky score, n (%) | |
| <70% | 177 (18.5%) |
| ≥70% | 779 (81.5%) |
ECOG PS: Eastern Cooperative Oncology Group performance status; IQR: interquartile range; NLR: neutrophil-to-lymphocyte ratio; PLR: platelet-to-lymphocyte ratio.
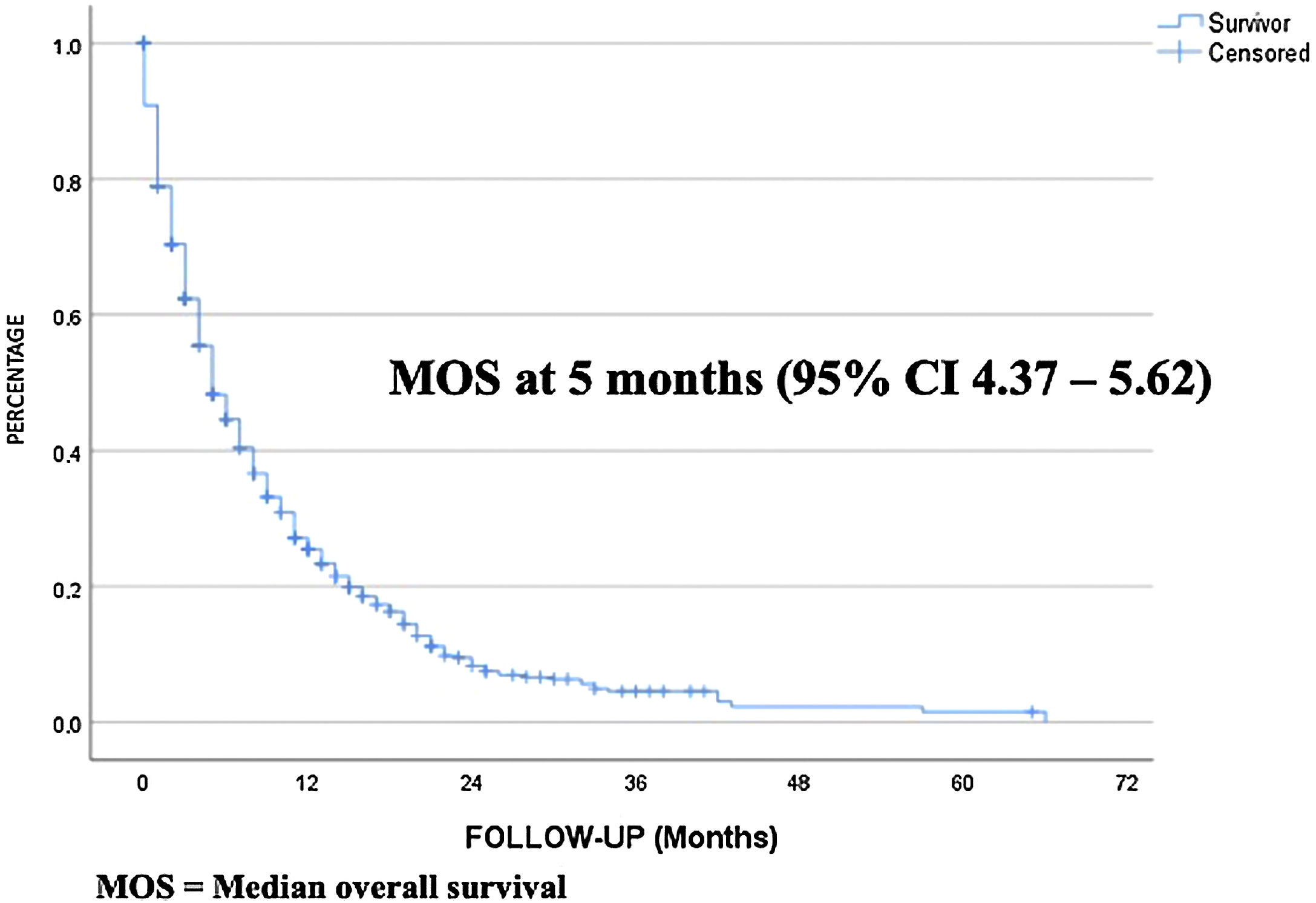
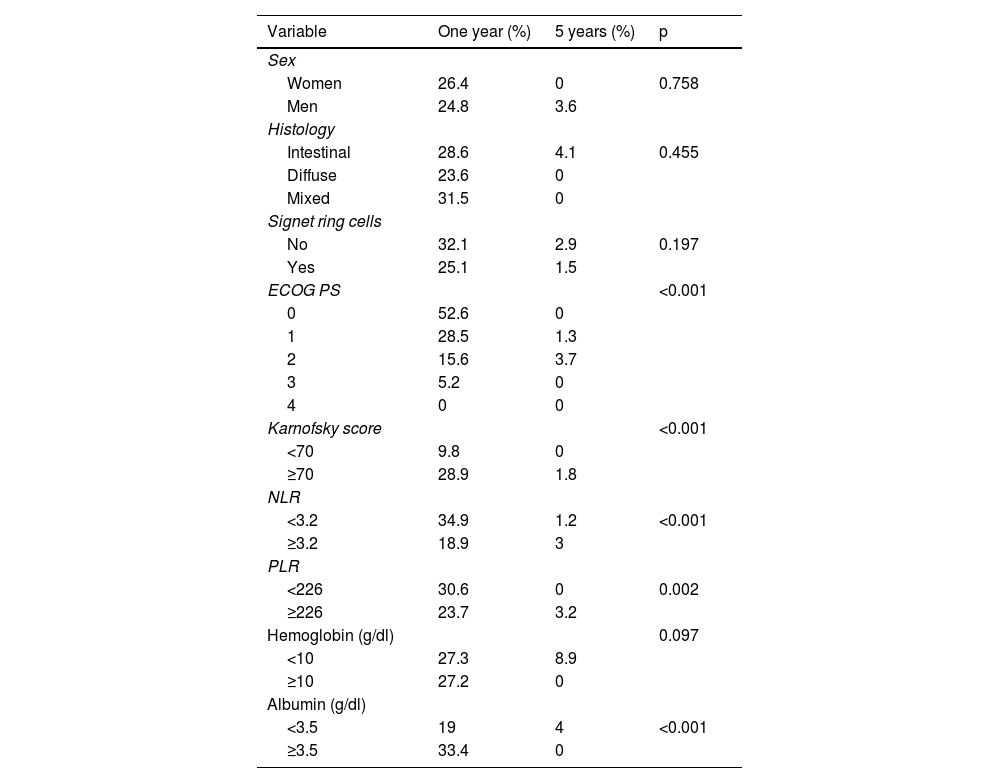
The median follow-up period was 4 months (IQR 1–9) and the median survival period was 5 months (95% CI 4.37–5.62) The overall one-year and 5-year survival rates were 25.6% and 1.5%, respectively (Fig. 1). For the univariate analysis, the variables with a statistically significant impact on survival were the NLR, the PLR, functional status (ECOG PS and Karnofsky score), and albumin. No statistical significance was found, with respect to sex, histologic type, signet ring cells, and hemoglobin, and so they were eliminated from the multivariate analysis. We observed a trend toward worse outcome in patients with diffuse adenocarcinoma, compared with intestinal adenocarcinoma (0 vs. 4.1%, p = 0.45) and a trend toward better survival in patients with a hemoglobin level below 10 g/dl, compared with higher hemoglobin values (8.9 vs. 0%, p = 0.14) (Table 2).
Univariate analysis for one and 5-year survival rates.
| Variable | One year (%) | 5 years (%) | p |
|---|---|---|---|
| Sex | |||
| Women | 26.4 | 0 | 0.758 |
| Men | 24.8 | 3.6 | |
| Histology | |||
| Intestinal | 28.6 | 4.1 | 0.455 |
| Diffuse | 23.6 | 0 | |
| Mixed | 31.5 | 0 | |
| Signet ring cells | |||
| No | 32.1 | 2.9 | 0.197 |
| Yes | 25.1 | 1.5 | |
| ECOG PS | <0.001 | ||
| 0 | 52.6 | 0 | |
| 1 | 28.5 | 1.3 | |
| 2 | 15.6 | 3.7 | |
| 3 | 5.2 | 0 | |
| 4 | 0 | 0 | |
| Karnofsky score | <0.001 | ||
| <70 | 9.8 | 0 | |
| ≥70 | 28.9 | 1.8 | |
| NLR | |||
| <3.2 | 34.9 | 1.2 | <0.001 |
| ≥3.2 | 18.9 | 3 | |
| PLR | |||
| <226 | 30.6 | 0 | 0.002 |
| ≥226 | 23.7 | 3.2 | |
| Hemoglobin (g/dl) | 0.097 | ||
| <10 | 27.3 | 8.9 | |
| ≥10 | 27.2 | 0 | |
| Albumin (g/dl) | |||
| <3.5 | 19 | 4 | <0.001 |
| ≥3.5 | 33.4 | 0 |
ECOG PS: Eastern Cooperative Oncology Group Performance Status; NLR: neutrophil-to-lymphocyte ratio; PLR: platelet-to-lymphocyte ratio.
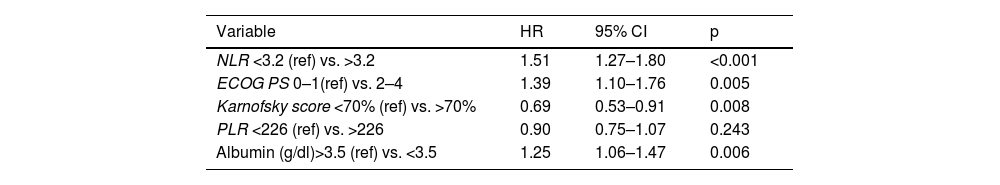
The multivariate analysis revealed that an NLR above 3.2 (HR 1.51, 95% CI 1.27–1.8; p < 0.001), albumin <3.5 g/dl (HR 1.25, CI 1.06–1.47; p = 0.006), and an ECOG PS above 2 (HR 1.39, CI 1.10–1.76; p = 0.005) can be predictors of a lower survival rate, whereas a Karnofsky score above 70% (HR 0.69, CI 0.53–0.91; p = 0.008) can be a predictor of better survival. The PLR was not statistically significant in the multivariate analysis (HR 0.90, CI 0.75–1.07; p = 0.24) (Table 3).
Multivariate analysis for survival.
| Variable | HR | 95% CI | p |
|---|---|---|---|
| NLR <3.2 (ref) vs. >3.2 | 1.51 | 1.27–1.80 | <0.001 |
| ECOG PS 0–1(ref) vs. 2–4 | 1.39 | 1.10–1.76 | 0.005 |
| Karnofsky score <70% (ref) vs. >70% | 0.69 | 0.53–0.91 | 0.008 |
| PLR <226 (ref) vs. >226 | 0.90 | 0.75–1.07 | 0.243 |
| Albumin (g/dl)>3.5 (ref) vs. <3.5 | 1.25 | 1.06–1.47 | 0.006 |
ECOG PS: Eastern Cooperative Oncology Group performance status; IQR: interquartile range; NLR: neutrophil-to-lymphocyte ratio; PLR: platelet-to-lymphocyte ratio.
The influence of the immune system on the mechanisms of invasion and metastasis in oncologic disease has been observed. A complete blood count and blood chemistry are accessible conventional studies that provide valuable information on the immunologic and nutritional statuses of the patient.4 We used those blood samples to determine the association of the NLR, PLR, hemoglobin, and albumin with the oncologic prognosis for survival in metastatic gastric cancer.
In a meta-analysis that included 9 studies and 3,709 patients with advanced stage gastric cancer, an elevated NLR prior to starting any treatment was reported to result in poorer survival and influence therapeutic decision-making and follow-up in patients.6 We obtained similar results, using a cutoff point of 3.2 for the NLR, and found that patients with a higher NLR had worse overall survival. In a meta-analysis conducted by Du et al. in that same setting, those authors suggested that NLR determination in patients with unresectable or metastatic gastric cancer can strengthen the indication for systemic treatment.11 Sun et al. carried out a classification that combined the NLR and PLR, finding that patients with high levels should have strict follow-up to identify early recurrence, and even evaluate giving adjuvant treatment, for improving outcomes.12
The results from studies on the PLR as a prognostic factor in gastric cancer have been controversial. In the meta-analysis by Cao et al., an increase in PLR predicted poorer overall survival, but those authors found no such association in the prospective studies of the meta-analysis or in studies conducted in Japan and Korea.13 In our study, we found no statistically significant association between the PLR and prognosis, which could be due to several factors, such as the selected cutoff point, the study population, or the clinical stage analyzed.
Shen et al., in a study with 1,688 patients with gastric cancer, reported that preoperative anemia was associated with voluminous tumors with a higher degree of invasion, greater lymph node involvement, and a more advanced tumor stage.14 Contradictorily, in our univariate analysis, we found that patients with hemoglobin levels <10 g/dl at hospital admission appeared to have a better survival prognosis; however, that was not reflected in the multivariate analysis. This contradiction could be explained by the fact that because our hospital is a cancer referral center, several of the patients had previously undergone multiple transfusions, resulting in a hemoglobin level >10 g/dl at hospital admission, but their tumors were most likely more advanced. Gou et al. suggested correcting the hemoglobin deficit with transfusions, prior to starting treatment, after observing that a low hemoglobin level during immunotherapy in metastatic disease can be an independent factor predicting poorer overall survival and a shorter disease-free period.15
In our study, we also observed worse oncologic outcomes when the albumin level was below 3.5 g/dl. It is important to remember that albumin values fluctuate under the influence of different factors, in addition to nutritional status. Oh et al. found that albumin and other nutritional parameters function as independent prognostic indicators in gastric cancer at different stages, especially in advanced tumors.10 We believe a Mexican consensus is needed to define the optimum time for calculating those scores and biomarkers, as well as establishing the cutoff points for defining elevated and low levels. In our study, we utilized the functional status observed at the first consultation, and for the cutoff points, we considered levels at which there was already functional limitation, such as an ECOG PS above 2 or a Karnofsky score lower than 70%. We found them to be independent predictors of survival that should be taken into account during therapeutic decision-making.
The usefulness of the abovementioned prognostic scores would most likely be greater when nomograms could be formulated from prospective studies that included multiple prognostic factors, analyzing their different cutoff points in a larger population from numerous institutions that receive gastric cancer patients, and thus incorporating them into a management algorithm in clinical practice guidelines. The most important limitation of our study is the possible bias inherent in the retrospective design of our methodology. We reported the experience of a single center and our results should be validated through a prospective study to determine the real benefits.
One of the strengths of our study is the fact that the number of patients included provided a representative sample of Mexican patients with metastatic gastric cancer admitted to the hospital over a 10-year period. Another strength is that the prognostic factors of the NLR, albumin, and functional status we identified are easily obtained and accessible at practically any hospital center in Mexico, enabling their applicability to be generalized in several centers.
In conclusion, our study on a Mexican population identified NLR, nutritional status determined through albumin measurement, and functional status as independent prognostic factors for survival in patients admitted to the hospital with a diagnosis of metastatic gastric cancer. We believe those variables can be considered biomarkers during therapeutic decision-making, but their usefulness must be validated and confirmed through prospective or multicenter studies.
Financial disclosureNo financial support was received in relation to this study/article.
Conflict of interestThe authors declare that there is no conflict of interest.