Klebsiella pneumoniae (K. pneumoniae) is a Gram-negative bacillus that causes nosocomial pneumonia and intra-abdominal and urinary tract infections1. Liver abscesses in patients with K. pneumoniae infection were first described in Taiwan in 1980. K. pneumoniae liver abscesses generally present with extrahepatic complications, such as bacteremia, sepsis, metastasis to the central nervous system (CNS), endophthalmitis, and necrotizing fasciitis, comprising the clinical syndrome now defined as invasive liver abscess syndrome2. The metastatic infection rate varies from 3.5 to 20%, and the mortality rate from 2.8 to 10.8%3. The hypervirulent serotypes, K1 and K2, have been identified and are characterized by increased capsule production and siderophore expression that worsen the clinical presentation. Hypervirulent K. pneumoniae has a mucoid phenotype and the associated genes include the regulator of mucoid phenotype A (rmpA), rmpA2, and the mucoviscosity-associated gene A (magA) that increases capsule production4.
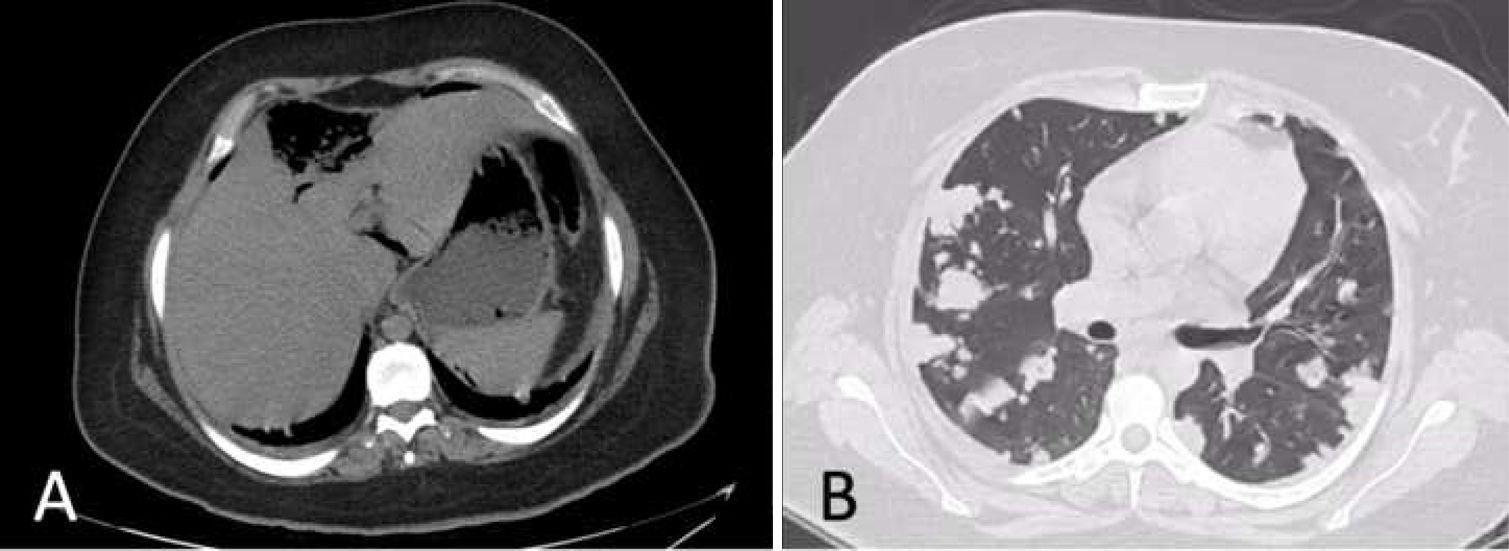
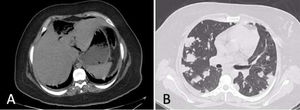
A 23-year-old woman, with a history of type 2 diabetes mellitus, arrived at the emergency room with diffuse abdominal pain, nausea, vomiting, and fever of 3-day progression. The pain intensified, radiating to the epigastrium and right hypochondrium. Her vital signs were heart rate of 131 beats per minute, respiratory rate of 24 breaths per minute, blood pressure of 110/60 mmHg, and temperature of 38.6 °C. Physical examination revealed bibasilar crackles, diffuse abdominal pain upon palpation, and signs of peritoneal irritation. Laboratory test results reported leukocytosis of 19,280 cell/mm3, neutrophils of 79.8%, and admission glucose level of 489 mg/dl. The rest of the laboratory tests were normal. A chest x-ray was ordered and identified multiple bilateral infiltrates (Fig. 1). A non-contrast chest and abdominal computed tomography (CT) scan showed a large 6 × 7.1 × 3 cm ruptured liver abscess, with gas bubble production, located in the right liver lobe. There was no diaphragmatic rupture or signs of continuity to the chest. Pneumoperitoneum, with free fluid in both parietocolic gutters, was present (Fig. 2A). Multiple cavitated pulmonary nodules, consistent with septic embolisms, were reported in the chest (Fig. 2B). The patient had not been previously treated, and so broad-spectrum antibiotics were started, but her clinical condition rapidly worsened and she progressed to septic shock, requiring vasopressors. The patient was taken to the operating room, where emergency laparotomy was performed, revealing approximately 1 liter of purulent matter in the abdominal cavity. Pus samples were taken for culture. Liver biopsy was performed to rule out malignancy. The abscess identified in segment IV was drained and the critically ill patient was admitted to the intensive care unit. She died 10 h after the surgical procedure. The culture report stated K. pneumoniae and the liver biopsy described fibrinous and purulent material.
Over the past few decades, the association of K. pneumoniae with a complex invasive syndrome has become recognized and is now identified as invasive liver abscess syndrome. It is a disease with worldwide prevalence and the frequency of K. pneumoniae in pyogenic liver abscesses has increased over the past 30 years in Taiwan2. The disease presents in immunocompromised patients, and diabetes mellitus is the most common predisposing factor5. A lower frequency of metastasis has been observed in diabetic patients with strict glycemic control6. Metastatic disease is associated with severe clinical presentation and a high mortality rate. Chang et al.3 reported that unilocular liver abscess was more virulent than the multilocular disease. Younger patients with a stronger immune system were hypothesized to present with more aggressive clinical symptoms due to findings of a higher APACHE II score, septic shock, metastatic infection, acute respiratory failure, and the formation of gas in the abscess observed in imaging studies7.
Chou et al.7 described pulmonary septic embolism, a complication that has not been widely studied, and reported a rate of 4.5% in a total of 14 cases. Eighty-three percent of those cases presented with diabetes mellitus and their prevalent symptoms were fever and dyspnea. Only one patient in their case series had abdominal pain upon hospital admission. In addition, those authors considered that abdominal ultrasound should be ordered to rule out liver abscess in diabetic patients presenting with fever, dyspnea, and a chest x-ray revealing multiple opacities and infiltrative patterns.
It is important to remember that pyogenic liver abscesses account for 75% of liver abscesses in industrialized countries, but only 66% of the bacterial pathogens are identified. In the United States, the increase in frequency of K. pneumoniae liver abscesses may reflect an increase in the Asian population seen at their institutions or be due to a previously unreported hypervirulent serotype8. To the best of our knowledge, the present case of invasive liver abscess syndrome is the first to be reported in Latin America. This syndrome should be suspected when a patient is immunocompromised and chest x-ray reveals infiltrates, along with an image suggestive of liver abscess, so that he/she can be treated opportunely, preventing the high mortality resulting from invasive liver abscess syndrome.
Ethical disclosuresThe authors declare that no experiments were conducted on humans or animals for the present study, that they have followed the protocols of their work center on the publication of patient data, and that they have preserved patient anonymity at all times. Informed consent was not required for the publication of the present case because the article contains no personal data that could identify the patient.
Financial disclosureNo specific grants were received from public sector agencies, the business sector, or non-profit organizations in relation to this report.
Conflict of interestThe authors declare that there is no conflict of interest.
Please cite this article as: Morales-Morales CA, González-Urquijo M, Quevedo-Fernández E, Gil-Galindo G. Síndrome de absceso hepático invasivo con embolismos pulmonares sépticos. Revista de Gastroenterología de México. 2021;86:439–441.