Pancreatic steatosis is an incidental radiologic finding in asymptomatic patients, and its clinical importance is unclear. Primary aim: to study the prevalence of pancreatic steatosis (PS) in consecutive patients registered at our hospital, that underwent computed axial tomography (CAT) scanning of the abdomen and pelvis, excluding known pancreatic diseases. Secondary aim: to review the association of PS with the demographic and clinical data of the patients, as well as with hepatic steatosis (HS).
Materials and methodsAn observational study was conducted on adult patients that had CAT scans of the abdomen and pelvis. Definitions: a) tissue density was measured in Hounsfield units (HU) in five 1 cm2 areas of the pancreas, three areas of the spleen, and in segments VI and VII of the liver; b) fatty pancreas: a difference < –10 HU between the mean pancreas and mean spleen densities; and c) fatty liver: density < 40 HU. We registered the epidemiologic and laboratory data of the patients. The association of those factors with the presence of PS was analyzed using SPSS version 24.0 software, and statistical significance was set at a p < 0.05.
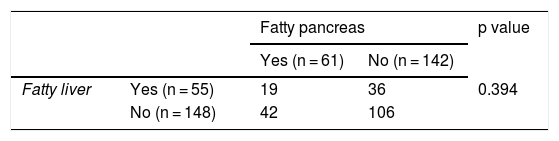
ResultsOf the 203 patients, PS was found in 61 (30%). The patients with PS were significantly older and had a higher body mass index. We found no significant association with the rest of the parameters studied, nor with HS (55 patients). None of the patients had symptoms attributable to a disease of the exocrine pancreas.
ConclusionsFatty infiltration of the pancreas is a frequent finding in CAT scans, and its clinical importance is unclear. Aging of the population and the increase in obesity underline the need for future studies on PS.
La esteatosis pancreática es un hallazgo incidental radiológico en pacientes asintomáticos, cuya importancia clínica es poco clara. Objetivo primario: estudiar la prevalencia de esteatosis pancreática (EP) en pacientes consecutivos, registrados en nuestro hospital, quienes realizaron tomografía axial computada (TAC) de abdomen y pelvis, excluyendo enfermedades pancreáticas conocidas. Objetivo secundario: revisar la asociación de EP con datos demográficos, clínicos y con esteatosis hepática (EH).
Material y MétodosEstudio observacional en pacientes adultos con TAC de abdomen y pelvis. Definiciones: A) la densidad del tejido fue medida en Unidades Hounsfield (UH) en 5 áreas de 1 cm2 del páncreas, 3 en el bazo y en los segmentos VI y VII del hígado; B) páncreas graso: promedio de páncreas-promedio de bazo < -10 UH; C) Hígado graso: densidad < 40 UH. Registramos los datos epidemiológicos y de laboratorio de pacientes. La asociación de estos factores con la presencia de EP fue analizado con software SPSS Versión 24.0., considerando p < 0,05 significativo.
ResultadosSe encontró EP en 61 de los 203 pacientes (30%). Los individuos con EP tuvieron significativamente mayor edad e índice de masa corporal. No encontramos asociación significativa con el resto de parámetros estudiados, tampoco con EH (55 pacientes). Ninguno de los pacientes tenía síntomas atribuibles a una enfermedad de páncreas exocrino.
ConclusionesInfiltración grasa de páncreas es un hallazgo frecuente en TAC, cuya importancia clínica es incierta. El envejecimiento de la población y el aumento de la obesidad subrayan la necesidad de futuros estudios sobre EP.
In 1933, Ogilvie observed an increase of fat content and hypertrophy of islets of Langerhans in 17% of obese persons, compared with 7% of normal weight persons1. In 1978, in material from autopsies, Olsen found that fatty infiltration of the pancreas was greater in the more advanced-age patients2. Fatty infiltration of the pancreas was also described as a radiologic finding3,4, but neither its nomenclature nor its clinical importance is clear. For many years, fatty infiltration of the pancreas was considered an innocuous condition, but in the past few decades, its association with obesity1 and metabolic syndrome5 has made it the focus of numerous observations and studies6–11. Over the years, many terms have been used to refer to the accumulation of fat in the pancreas. The uncertainty regarding the nomenclature also reflects the different concepts, ranging from obesity-related fatty infiltration, through acinar cell replacement with fat, which does not involve major damage to the pancreas, to nonalcoholic steatopancreatitis (NASP), which leads to the concept of potentially progressive disease.
There has been an alarming increase in overweight and obesity worldwide, with a prevalence of 33.8% (2007-2008) in the United States12. In Chile, in 1990, Berrios et al. reported obesity in 19.6% of men and 30.8% of women in the metropolitan area13. At the national level in Chile, obesity increased from 23.2% in 2003 to 34.4% in 2016, in the general population14. Obesity is associated with diseases with a great impact on public health, such as metabolic syndrome, cardiovascular diseases, and different types of cancer15–17. Obesity is also associated with fatty infiltration and inflammation in different organs, including the liver (hepatic steatosis [HS], nonalcoholic steatohepatitis [NASH]), skeletal muscle, heart, and pancreas18,19.
Three main imaging methods have been utilized to determine the presence of pancreatic steatosis (PS): abdominal ultrasound, computed axial tomography (CAT) scanning, and abdominal magnetic resonance imaging (MRI). Each method has its particular criteria and there are no definitive international consensuses that unify them. An adequate correlation was demonstrated between histologic findings and abdominal CAT imaging of fatty infiltration of the pancreas20.
The worldwide prevalence of fatty pancreas is not well known. Its estimated prevalence in China21 was reported at 16% in a 2014 publication and increased to 30% in 201622. No national data are available in Chile.
The primary aim of our study was to determine the prevalence of PS in adult patients that had CAT scans of the abdomen and pelvis, excluding patients with known pancreatic diseases. As the secondary aim, the association of PS with demographic and clinical data of the patients, as well as with HS, was reviewed.
Materials and methodsA retrospective, descriptive, observational study was conducted, in which CAT scans of the abdomen and pelvis, taken during the months of April and May 2015 at the Hospital Clínico Universidad de Chile, were analyzed. All consecutive adult patients that had a clinical record at our hospital were included. The exclusion criteria were: age below 15 years, known pancreatic diseases (acute pancreatitis, chronic pancreatitis, cancer of the pancreas), and known liver diseases (cirrhosis, NAFLD, etc.).
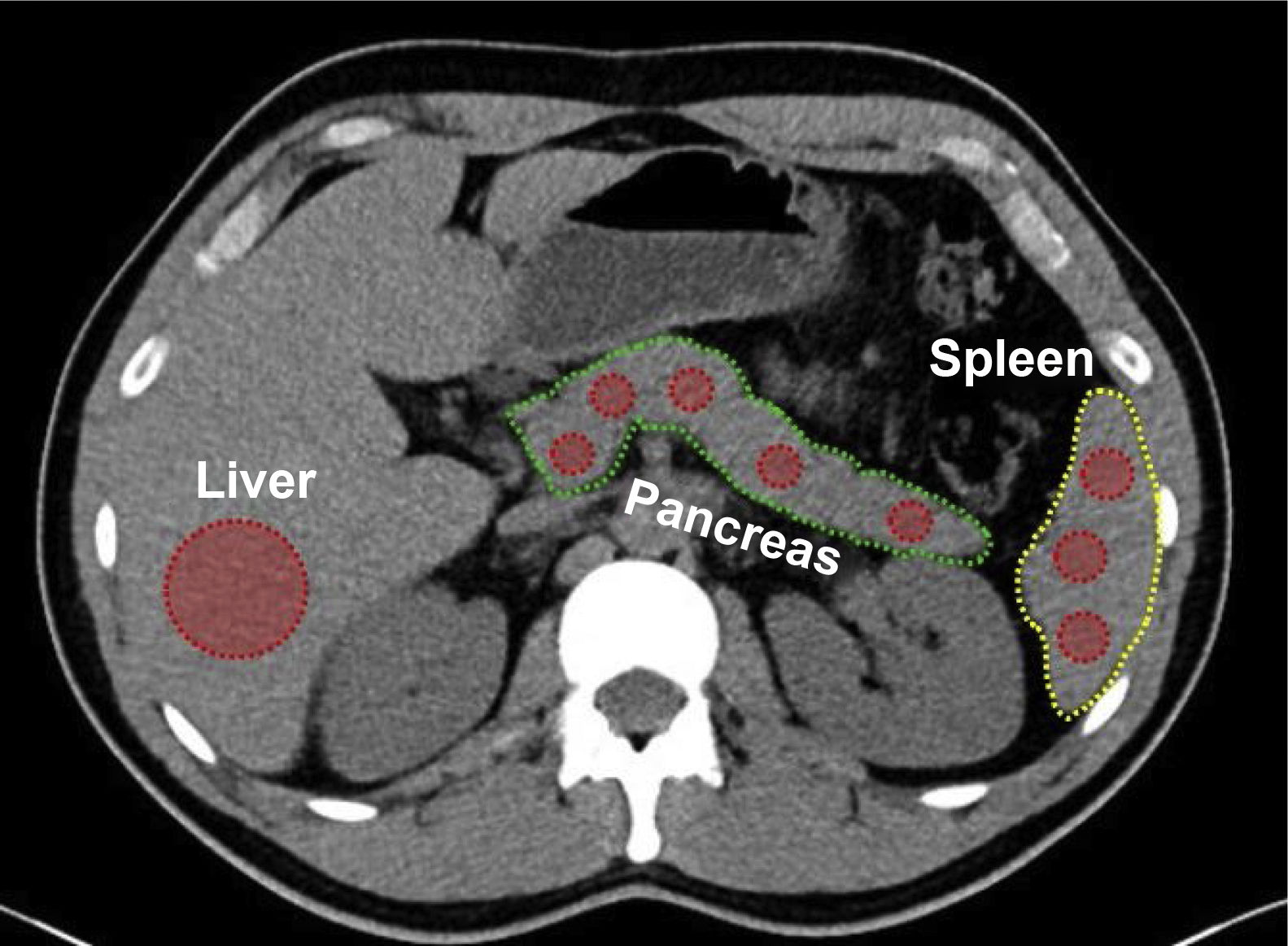
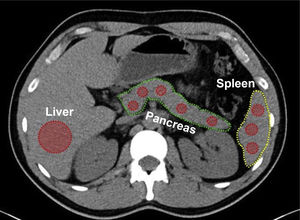
Density measurements of the pancreas and liverThe density of the pancreas was determined during the non-enhanced phase of the CAT scan20 in 5 areas measuring approximately 1 cm2 (uncinate process, head, neck, body, and tail), utilizing Hounsfield units (HU), and compared with the density of the spleen, measured in 3 random areas. The mean of the measurements in each of the two organs was calculated. At the same time, the density of the liver parenchyma was measured at an extensive region of interest (ROI) in segments VI and VII (Fig. 1).
PS criterion: difference between the mean densities of the pancreas and spleen < –10 HU.
HS criterion: density of the liver < 40 HU10.
Variables included in the studyThe data were collected from the clinical records of the patients. They included the demographic variables (age, sex) and clinical variables (body mass index [BMI], a history of diabetes mellitus [DM], and blood glucose values and lipid profile at the time of the test). The nutritional status of the patient was defined, based on the BMI (kg/m2); low weight (<18.5), normal weight (18.5-24.9), overweight (25-29.9), and obesity (>30).
The measurement and calculation data were registered on an Excel table.
Statistical analysisThe categorical variables were expressed as absolute value and percentage, whereas the quantitative variables were expressed as mean ± standard deviation or median and range, depending on whether their distribution was normal or non-normal.
Normal distribution of the data was evaluated using the Shapiro-Wilk test and the differences between groups was evaluated using the Kruskal-Wallis test or the Mann-Whitney U test, followed by the post hoc analysis of multiple differences. The proportions test, chi-square test, or Fisher’s test, as needed, were used for the categorical variables (p < 0.05). The correlation of PS with age and BMI was determined using the Spearman’s correlation coefficient. The analyses were carried out with SPSS software (IBM Corp. Released 2016. IBM SPSS Statistics for Windows, Version 24.0. Armonk, NY, USA).
Ethical considerationsThe study meets the current bioethics research regulations. The authors declare that the present article contains no personal information that could identify the patients. The project and retrospective review of the clinical records were approved by the Ethics Committee of the Hospital Clínico Universidad de Chile (HCUCh No. 023, August 2015).
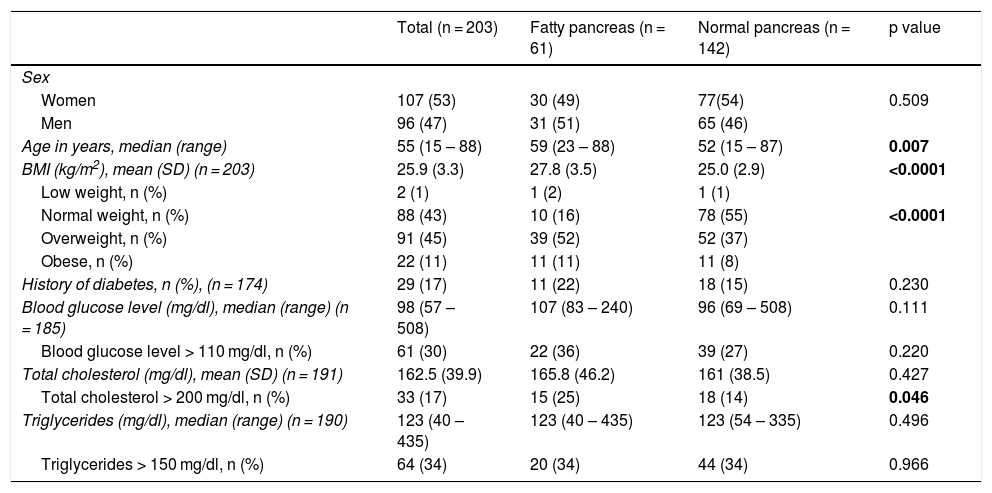
ResultsA total of 203 patients (1 CAT scan/patient) were included. Median patient age was 55 years (range 15-88) and 96 (47%) of the patients were women. Forty-four percent of the patients were normal weight and 29 patients had known diabetes. Table 1 shows the demographic and clinical characteristics of the patients. Abdominal CAT scan indications, within the study period, were abdominal pain in 31%, renal colic in 29%, suspected neoplasm 10%, postoperative control in 7%, suspected appendicitis in 6%, and other causes in 17%.
Demographic, clinical, and laboratory test characteristics of the patients evaluated through abdominal CAT scan, according to the density of the pancreas.
| Total (n = 203) | Fatty pancreas (n = 61) | Normal pancreas (n = 142) | p value | |
|---|---|---|---|---|
| Sex | ||||
| Women | 107 (53) | 30 (49) | 77(54) | 0.509 |
| Men | 96 (47) | 31 (51) | 65 (46) | |
| Age in years, median (range) | 55 (15 – 88) | 59 (23 – 88) | 52 (15 – 87) | 0.007 |
| BMI (kg/m2), mean (SD) (n = 203) | 25.9 (3.3) | 27.8 (3.5) | 25.0 (2.9) | <0.0001 |
| Low weight, n (%) | 2 (1) | 1 (2) | 1 (1) | |
| Normal weight, n (%) | 88 (43) | 10 (16) | 78 (55) | <0.0001 |
| Overweight, n (%) | 91 (45) | 39 (52) | 52 (37) | |
| Obese, n (%) | 22 (11) | 11 (11) | 11 (8) | |
| History of diabetes, n (%), (n = 174) | 29 (17) | 11 (22) | 18 (15) | 0.230 |
| Blood glucose level (mg/dl), median (range) (n = 185) | 98 (57 – 508) | 107 (83 – 240) | 96 (69 – 508) | 0.111 |
| Blood glucose level > 110 mg/dl, n (%) | 61 (30) | 22 (36) | 39 (27) | 0.220 |
| Total cholesterol (mg/dl), mean (SD) (n = 191) | 162.5 (39.9) | 165.8 (46.2) | 161 (38.5) | 0.427 |
| Total cholesterol > 200 mg/dl, n (%) | 33 (17) | 15 (25) | 18 (14) | 0.046 |
| Triglycerides (mg/dl), median (range) (n = 190) | 123 (40 – 435) | 123 (40 – 435) | 123 (54 – 335) | 0.496 |
| Triglycerides > 150 mg/dl, n (%) | 64 (34) | 20 (34) | 44 (34) | 0.966 |
BMI: body mass index; SD: standard deviation.
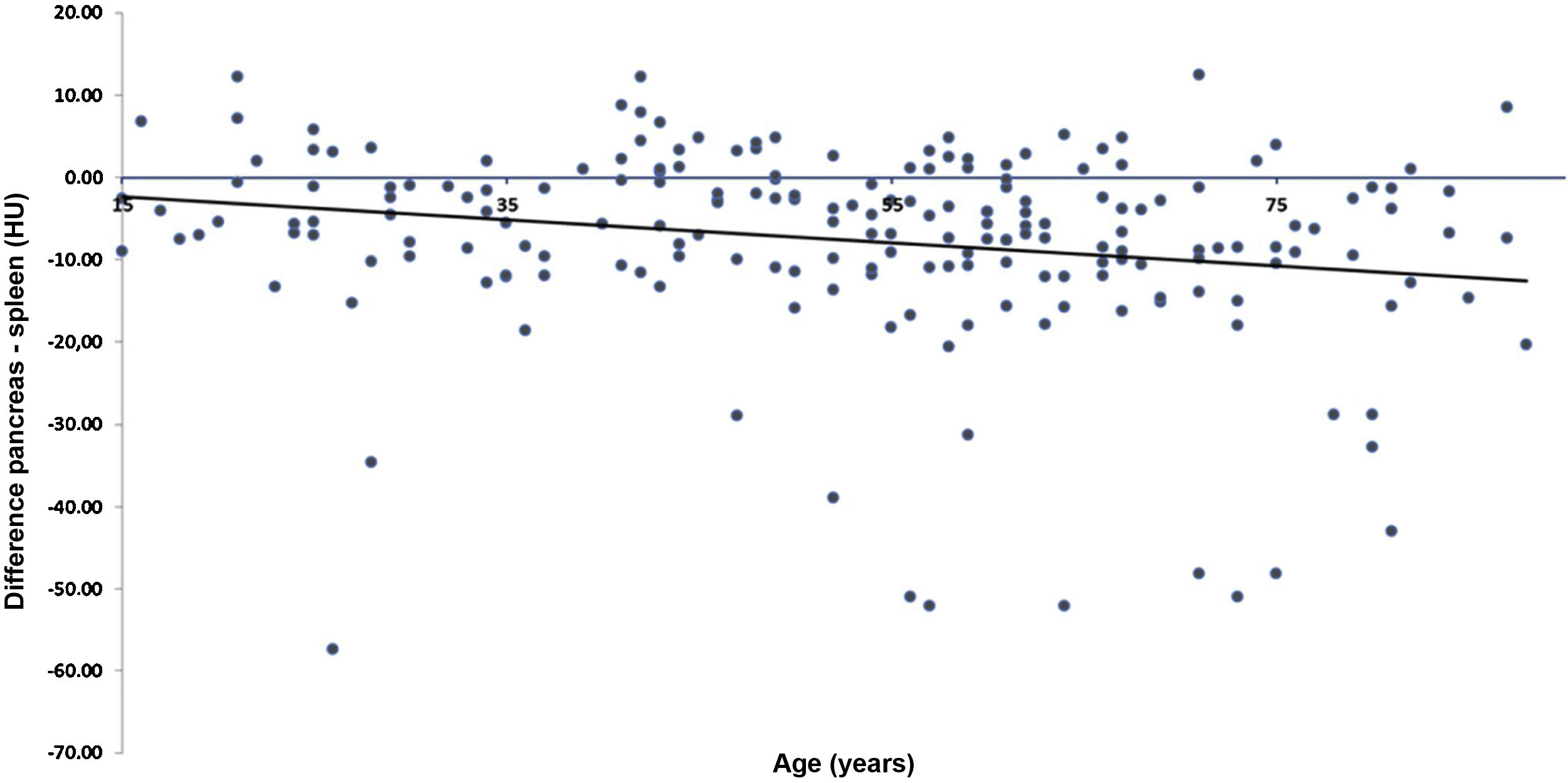
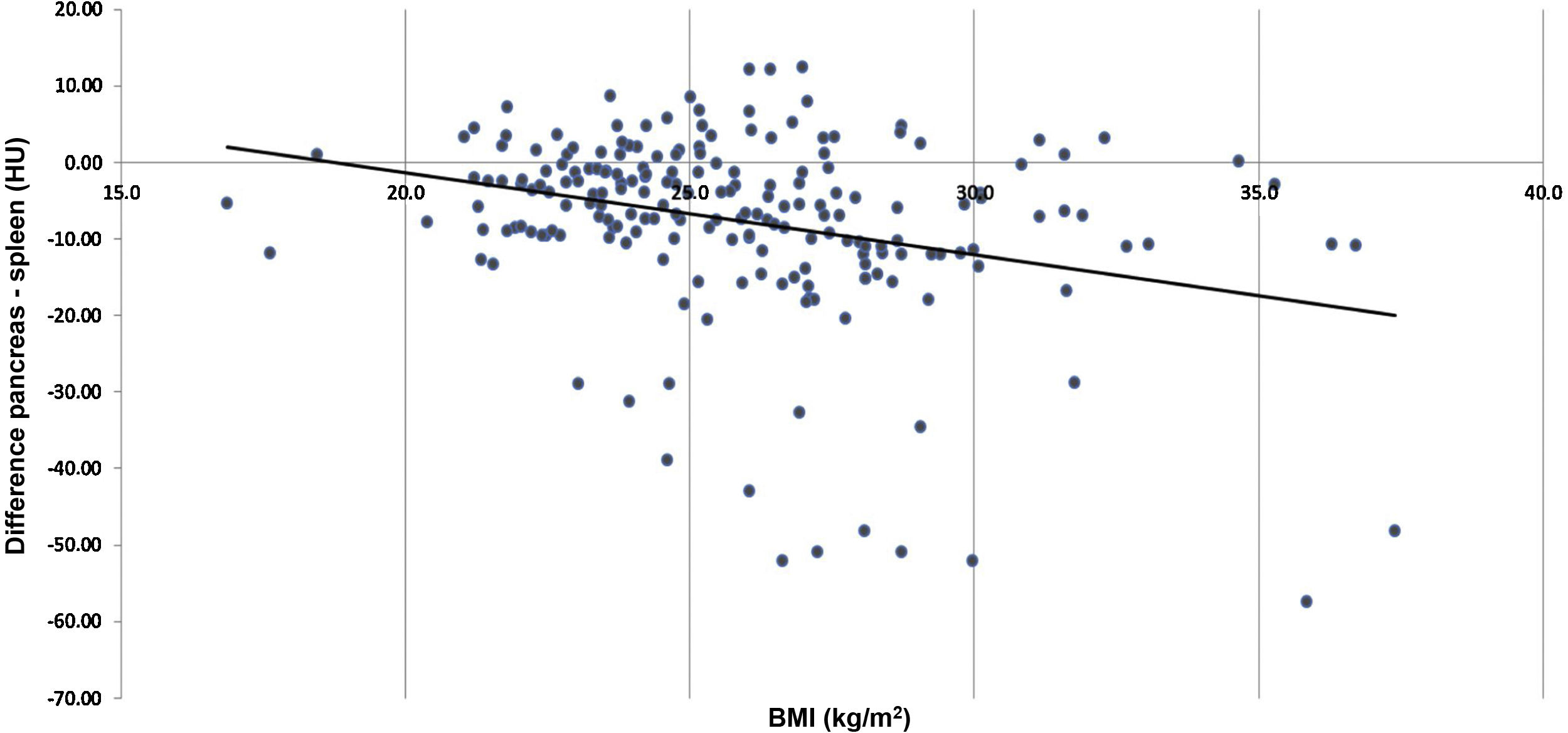
The difference between the mean pancreas and mean spleen densities (that difference referred to as P-S, hereafter) was below –10 HU in 61 patients (30%) (Table 1). No difference between men and women was found. The correlation between the numeric value of the P-S and age was significant and the lowest values were more frequent in the older patients (Fig. 2) (Spearman’s correlation coefficient in r = –0.23396, p = 0.00078). Analyzing the presence of PS, there was a significant correlation: patients with PS were significantly older than those with normal pancreatic density (Table 1). PS was also significantly correlated with the increase in BMI (Spearman’s correlation coefficient in R = –0.29581, p < 0.0001) (Fig. 3). The patients with fatty pancreas had a significantly higher BMI (Table 1). Diabetes was somewhat more frequent in the patients with PS than in those with a normal pancreas, but with no statistical significance. Likewise, we observed no significant association between PS and elevated cholesterol and triglyceride levels or with blood glucose levels (Table 1).
Liver density was below 40 HU, consistent with HS in 55 cases (27%), and the frequency of PS was similar to that of HS in the total patient group. In the 61 cases with PS (P-S < –10 HU), there was associated HS in 19 patients (31%) (Table 2). Even though HS in patients with PS was more frequent than in the group with normal pancreas, and PS was also somewhat more frequent in patients with HS (34% vs. 28% in patients with no HS), the association of the involvement of the two organs was not statistically significant.
Discussion and conclusionThe primary aim of our work was to study the frequency of PS in a cohort of Chilean patients with no pancreatic disease, focusing attention on this little-known entity, whose clinical and pathophysiologic importance is the subject of a growing number of studies. Unlike the diagnostic imaging of HS, the presence of PS is only described incidentally in radiologic reports. The first difficulty is related to the diagnostic criteria for PS utilized for the detection of fatty infiltration in imaging studies. Diagnosis is not difficult when there is complete pancreatic lipomatosis, as in some rare cases of cystic fibrosis23 or Johanson-Blizzard syndrome24. The diagnosis of lipomas of the pancreas through imaging studies is not difficult either. Complete focal replacement, with fat circumscribing the pancreatic parenchyma, is identified, preventing unnecessary surgeries in the majority of cases25. The morphologic criteria of the different grades of fatty infiltration in CAT scans are clear: the pancreas is hypodense, compared with the spleen. However, the numeric value of the cutoff point that determines the minimum grade of significant steatosis is not clearly defined: although there is no general consensus on a numerical cutoff value26, some authors accept a P-S < –5 HU10, whereas others consider a pancreas-to-spleen attenuation ratio (P/S) < 0.727. Singh et al. described a fat content in healthy individuals of up to 6.2%28, and others accepted a fat content > 10.4%, as a significant histologic threshold for PS29. Kim et al.20 reported an excellent correlation between histologic fat content measurements and the parameters obtained through CAT scans. A graph supplied by those authors showed that 10% of fat content coincided with a P-S –10 HU and a P/S of 0.8. Therefore, we chose the P-S < –10 HU criterion: a lower difference (–5 HU) would include doubtful cases, whereas a ratio of 0.7 would leave out individuals with PS.
Few studies have analyzed the prevalence of PS, and we know of none conducted in Chile. A recent study carried out in China, on 1,190 subjects undergoing a medical examination, using abdominal ultrasound as the diagnostic instrument, reported a prevalence of 30.7%, with a significant correlation with obesity, diabetes, and metabolic syndrome22. That association is described in numerous studies, both clinical5 and anatomopathologic30. In a systematic review and meta-analysis by Singh et al.28, they calculated an overall prevalence of PS at approximately 33%. They found that PS was significantly associated with high blood pressure, type 2 diabetes mellitus, and metabolic syndrome28. One of the most accepted theories indicates that PS contributes to a progressive loss of beta cell mass, affecting their function, and in turn, promoting the appearance of diabetes11,31,32.
The frequency of PS in our series was similar to that reported in the abovementioned studies. Our observations confirm the increased probability of PS, in relation to age and BMI. In addition to the fact that populations will continue to age in the following decades, a sedentary lifestyle and a lack of balance in caloric intake and output, favor the increase in obesity. In Chile, recent data confirm a 24% increase in obesity in children at 6 years of age, a 15% increase at 14 years of age, and a considerably higher increase in adolescents above 15 years of age, with an overall prevalence of obesity of 34%14. Obesity is associated with a proinflammatory state, and low-grade inflammation favors fat accumulation33.
We could not confirm a significant association between PS and diabetes, albeit there were more diabetics among the individuals with PS. A high cholesterol level was more frequent in the patients with PS, but a high triglyceride level was not. Even though the association was weak, we have no information on the possible treatment with statins, which is frequent in the older population.
The clinical importance of PS is still uncertain. Forty years ago, in studies by the Bordalo group, they presented histologic images, showing a fatty infiltration-fibrosis-chronic pancreatitis sequence in alcoholics34,35, but their theory was not widely accepted. Only recently, evidence was published on PS as a risk factor for the development of chronic pancreatitis, although unrelated to alcohol consumption36, and the authors of a report on 3 cases of advanced chronic pancreatitis suggest the etiologic importance of dyslipidemia and NAPS37. We emphasize that none of our patients had clinically manifested disease of the exocrine pancreas.
Data on the association of NAPS and NAFLD vary: some authors describe simultaneous involvement of the liver and pancreas19 in their patients, whereas others do not38. In NAFLD, fat accumulates in the hepatocytes, but in the pancreas, fat predominantly accumulates in the interlobular or intralobular spaces, leaving the exocrine and endocrine cells unharmed. However, morphologic and functional alterations of the islets are described in several studies conducted on obese patients, even in prediabetic subjects, and especially in men39. The reduced secretion of insulin increases the ectopic accumulation of fat, which also occurs in the pancreas, and consequently further deteriorates beta cell function, completing a vicious cycle. In our work, the association between the involvement of the liver and pancreas was weak and inconsistent. Taking the previously described data into account, if there is simultaneous involvement of the liver and pancreas, there is a greater risk for the progression to NAFLD due to the deterioration in endocrine function of the pancreas, with the consequent appearance of diabetes.
We observed a high prevalence of NAPS in our study, in the non-selected radiologic studies carried out, in relation to extrapancreatic diseases. The high number of cases shows that fatty infiltration of the pancreas does not cause clinical symptomatology, or abdominal discomfort, in the large majority of individuals, nor does it produce clinically manifested exocrine or endocrine pancreatic insufficiency. In addition, if only a minority of cases of NAPS present with progressive damage to chronic disease and involvement of the endocrine pancreas and exocrine pancreas, its elevated prevalence has epidemiologic importance for the early detection and follow-up of PS. Only the long-term follow-up of patients with PS can answer the question: Does PS progress to chronic pancreatic damage, albeit only in a minority of cases, similar to the liver?
Our study has certain limitations. It was carried out at a single center, and the included patients were not selected. The study was conducted on a very specific population of patients with abdominal symptoms, which could cause bias, given that the data cannot be extrapolated to the general population. Due to its retrospective design, our study lacks information on other concomitant diseases, medications, alcohol use, and smoking, present in the patients, which could have been relevant to the analysis.
In conclusion, we found a high frequency of asymptomatic PS in the patients that underwent abdominal CAT scans in 2 consecutive months at our hospital. PS was significantly associated with older age and increased BMI. Its prevalence was concurrent with the aging of the population and the increase in obesity. Dedicated attention on the part of radiologists, as well as specialists in diabetes and gastroenterologists, is required. Only prospective studies can clarify the evolution of fatty pancreas and its consequences on the function of the exocrine pancreas and the endocrine pancreas.
Financial disclosureNo specific grants were received from public sector agencies, the business sector, or non-profit organizations in relation to this study.
Conflict of interestThe authors declare that there is no conflict of interest.
Please cite this article as: Berger Z, Orellana F, Cocio R, Torres F, Simian D, Araneda G, et al. Esteatosis pancreática: hallazgo frecuente en población chilena. Revista de Gastroenterología de México. 2023;88:118–124.


![Correlation between pancreatic steatosis (P-S [HU]) and age (years). Correlation between pancreatic steatosis (P-S [HU]) and age (years).](https://static.elsevier.es/multimedia/2255534X/0000008800000002/v1_202305280003/S2255534X21001432/v1_202305280003/en/main.assets/thumbnail/gr2.jpeg?xkr=ue/ImdikoIMrsJoerZ+w97o/wdEXW47bqlyT1CqG6R0=)
![Correlation between pancreatic steatosis (P-S [HU]) and BMI (kg/m2). Correlation between pancreatic steatosis (P-S [HU]) and BMI (kg/m2).](https://static.elsevier.es/multimedia/2255534X/0000008800000002/v1_202305280003/S2255534X21001432/v1_202305280003/en/main.assets/thumbnail/gr3.jpeg?xkr=ue/ImdikoIMrsJoerZ+w97o/wdEXW47bqlyT1CqG6R0=)

