A 78-year-old woman, resident of Mexico City, had a past history of open cholecystectomy, scoliosis in occasional treatment with anti-inflammatory agents for 10 years, and allergy to penicillin.
Study motive. One year and 6 months with hyporexia, occasional nausea with no vomiting, mild intermittent pain in the epigastrium and hypogastrium, weight loss of 4kg in one year, stools with reduced consistency, and hematochezia during the past 4 months.
The patient had a body mass index of 25, oval-shaped ephelides measuring 2-3mm on the face and neck, and 1-2mm on the back of the hands, a mildly distended abdomen, and hepatomegaly.
Laboratory tests reported negative fecal occult blood, hemoglobin 8.9mg/dl, and hematocrit 28%.
She had been studied by the Oncology Service 4 months earlier for suspicion of cancer. An abdominal tomography scan showed hepatic lesions consistent with metastasis and fine needle biopsy of the lesions was performed. The histopathologic study reported malignant melanoma metastasis. Cytology was also consistent with malignant melanoma.
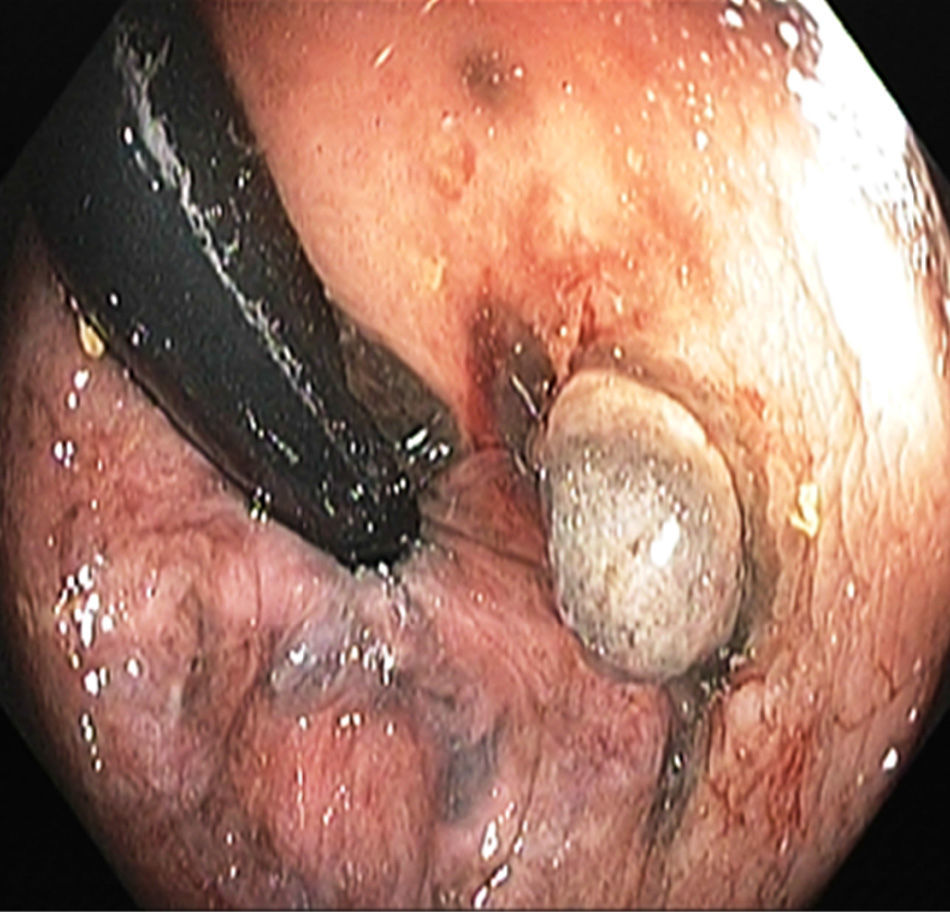
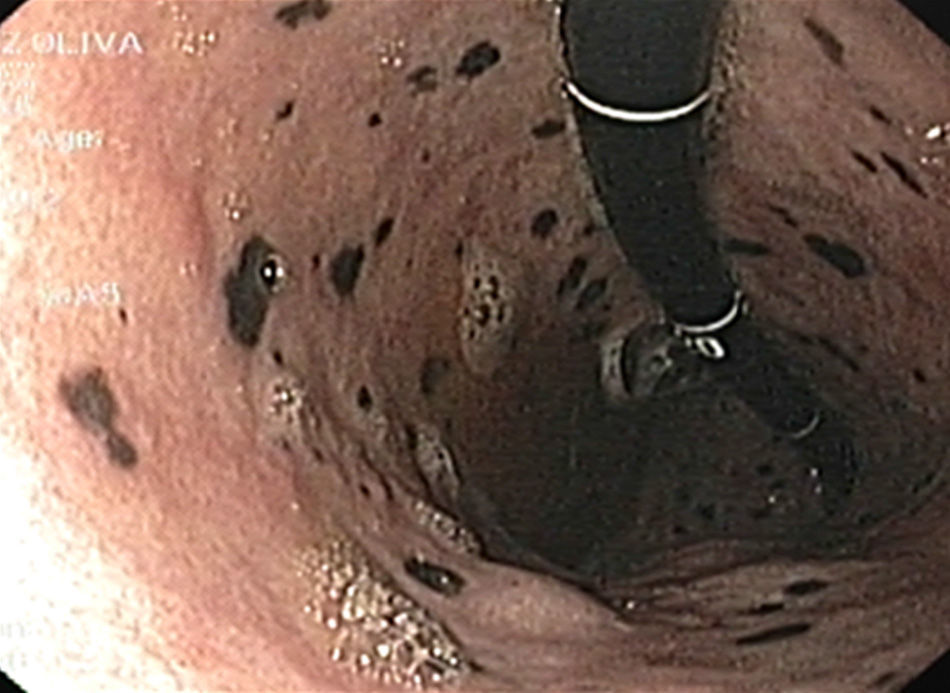
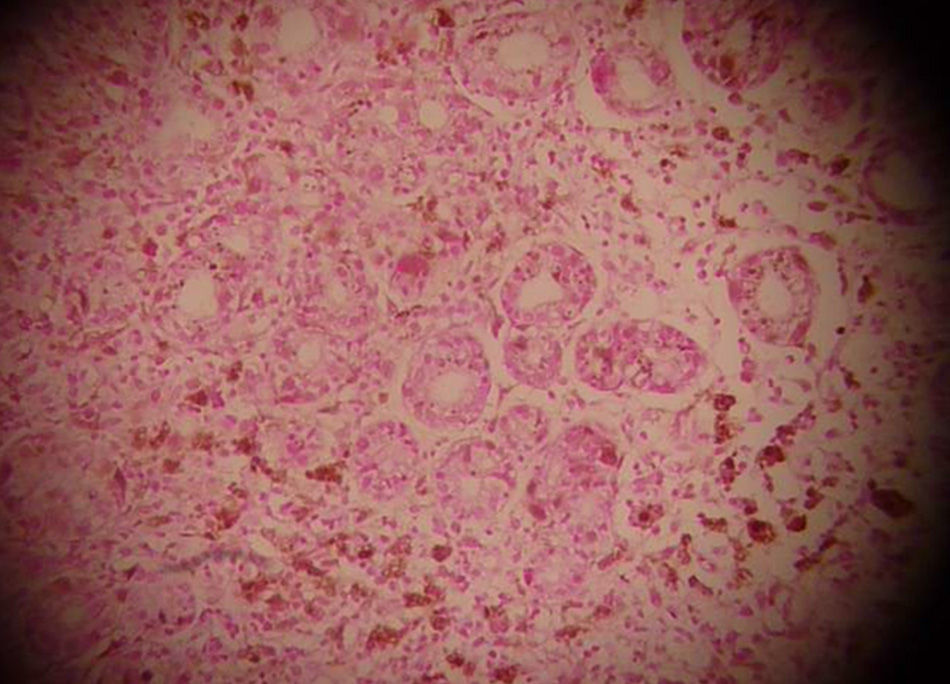
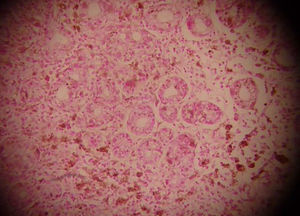
Lower gastrointestinal endoscopy revealed a vegetative, lobulated, hyperchromic lesion 2cm from the anal margin consistent with malignant melanoma and diffuse flat hyperchromic lesions measuring 2-3mm in the descending colon and the sigmoid colon (fig. 1). The histopathologic report confirmed malignant melanoma. Upper gastrointestinal endoscopy showed unaltered esophageal mucosa and multiple non-confluent 2-3mm flat, hyperchromic lesions in the stomach. The first and second portion of the duodenum had multiple flat, hyperchromic lesions of similar characteristics (fig. 2). The histopathologic study reported gastric and duodenal melanosis due to melanin deposits at the macrophage level of the lamina propria. For the differential diagnosis a Fontana-Masson stain was done and its result was positive (fig. 3); a Pearls stain was negative in both biopsies.
A distinction should be made between melanosis, as the pigmentation of mucosae from the deposit of melanin in the macrophages-lysosomes at the level of the lamina propria, and pseudomelanosis, described as a pigmentation of the mucosae secondary to deposits of iron, ferrous sulfide, hemosiderin, lipomelanin, lipofuscin, calcium, potassium, aluminum, magnesium, and silver at the same level.1 After a review of the medical literature, we found reports of cases with pseudomelanosis secondary to the deposit of iron mainly at the level of the duodenum, with a predominance in Afro-American women in the seventh decade of life (range of 18 months -79 years).2–5 Important pigmentation pathology references at the level of the digestive tract include melanosis coli, which is the deposit of pigments at the level of the colon mucosa associated with the abuse of oral laxatives,6 and melanosis at the level of the esophagus, ileum, jejunum, peritoneum, cecal appendix, mesenteric lymph nodes, and the duodenum; the latter is secondary to iron deficiencies and ulcer cicatrization.3,5,7 Chronic renal failure (> 60% of the cases) and essential hypertension (> 80% of the cases) are associated with these findings, with no apparent cause-and-effect.8 More than 20 drugs have been associated with pseudomelanosis, but the most frequently mentioned are furosemide, beta-blockers, thiazides, and iron supplements.5 The pigmentation lesions in the antrum and duodenum, as some reports have described, could be related to iron-deficient anemia; when the anemia was corrected the gastric lesions regressed. There are reported cases of late recurrent melanomas associated with melanin pigmentation at the duodenal level, as well as an isolated case of panenteric melanosis secondary to a malignant melanoma confirmed by histopathology.9,10 In relation to malignant melanoma presentation sites, the rectum holds third place, after the skin and the eye.
In regard to our particular case, we found only one reported case in the medical literature of panenteric melanosis secondary to a malignant melanoma that was histologically confirmed by corroborating the benign, submucosal, hyperchromic lesions at the gastric, duodenal and colonic levels.
The outcome and progression of these types of diffuse, hyperchromic lesions initially observed is highly suspicious of malignancy, therefore a complete study protocol that searches for an accurate clinical and endoscopic diagnosis must be started, emphasizing the fact that the lesions initially described in our case were a benign manifestation of an underlying malignant melanoma.
Financial disclosureNo financial support was received in relation to this article.
Conflict of interestThe authors declare that there is no conflict of interest.
Please cite this article as: Armienta SR, Camacho NM, Hernández GME, Plata PEJ. Melanosis panentérica secundaria a melanoma rectal. Reporte de caso. Revista de Gastroenterología de México. 2014;79:60–62.