The precision of endoscopic ultrasound (EUS) in the differential diagnosis of solid pancreatic lesions made through fine-needle aspiration biopsy (FNAB) is 74-95%.1–3
EUS elastography evaluates tissue elasticity and rigidity and is based on the premise that the compression of a given tissue through an echoendoscope produces a certain tension, which differs from organ to organ, depending on the hardness or softness of each one. EUS elastography can improve the diagnostic precision of EUS and FNAB.4
We present herein 2 patients presenting with pancreatic lesions that we treated with EUS elastography; up to the present, ours is the first report on this technique in Mexico. A linear
echoendoscope (EG-3870UTK®, Pentax) and a fine needle aspiration 22G needle (Wilson Cook, Winston-Salem, NC, USA) were used in the 2 cases. The Hitachi Preirus® platform (Hitachi-Aloka Medical, Ltd) was used for the elastography; it produces an image that shows a color map representing the distribution of tissue elasticity within a preselected region of interest, superimposed on the conventional EUS mode-B image. Hard tissue is blue and soft tissue is red; tissues with an intermediate elasticity are in the green-yellow spectrum. Images are interpreted by comparing the elasticity of a given lesion with that of a reference area that is selected inside the same organ or from an adjacent soft tissue; this is called the strain ratio (SR).5 It is important to remember that the pressure or strength applied to the tissue with the EUS modifies or determines the color tones and therefore the SR value, making adequate technique a necessity in order to prevent acquisition and interpretation errors.
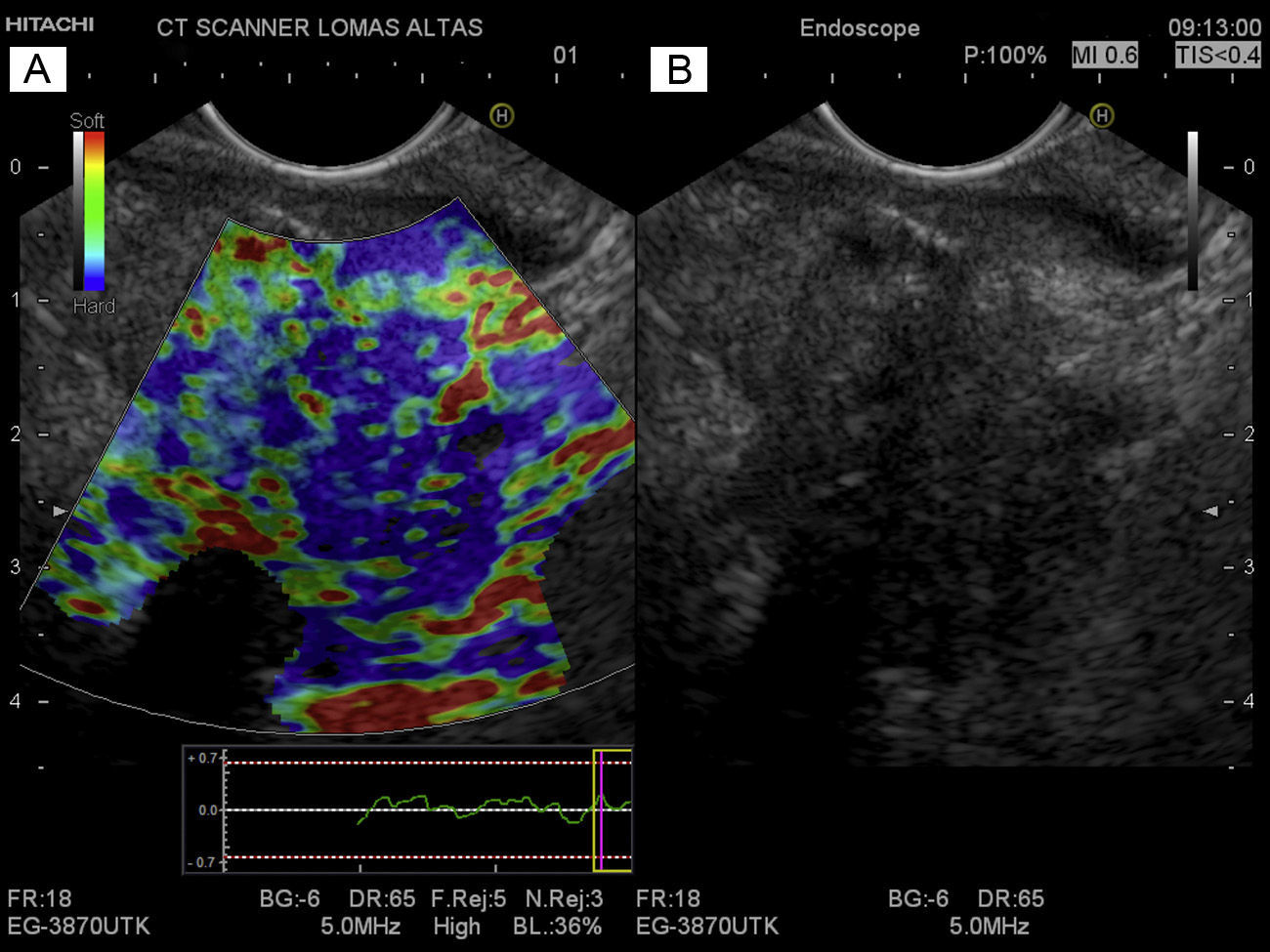
Case 1A 75-year-old man presented with a hypodense lesion in the neck of the pancreas. A EUS-guided FNAB was performed. The cytopathologic report was adenocarcinoma of the pancreas. During the elastography, the pancreatic lesion was seen as blue, which was indicative of hard and not very elastic tissue, compared with the peripheral tissue that was green, corresponding to soft tissue (fig. 1).
A) The elastographic image of adenocarcinoma of the neck of the pancreas. The blue area seen in the center corresponds to the tumor (rigid tissue), the site where the FNAB was performed. Normal (soft) pancreatic tissue surrounds the tumor. B) The EUS mode-B image of a hypoechoic, heterogeneous lesion with irregular edges in the neck of the pancreas that corresponds to adenocarcinoma of the pancreas in the pancreatic neck. It is not possible to differentiate the tumor from the surrounding normal pancreatic tissue.
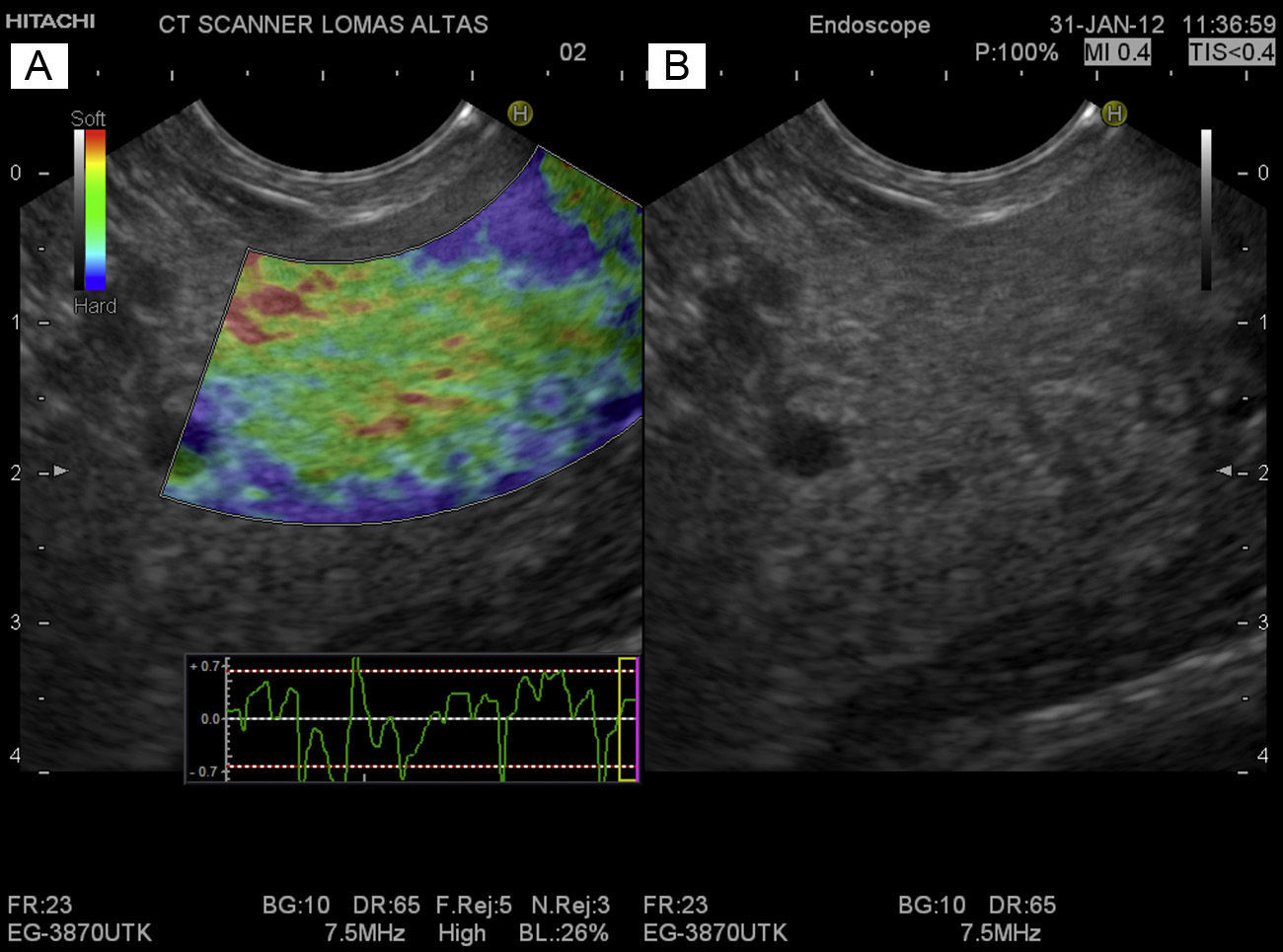
A 59-year-old woman presented with a cystic lesion in the body of the pancreas. EUS revealed a 7.3 x 3.6mm lesion, suggestive of an intraductal papillary mucinous neoplasm with no poor outcome data. The cyst was aspirated, obtaining a transparent and viscous fluid. The pancreas had a normal aspect. In the elastography, the cyst and the pancreas were green, suggesting soft and elastic tissue (fig. 2).
A) The elastographic image of a cyst in the body of the pancreas surrounded by normal pancreatic parenchyma. Green and red are the predominant colors and they correspond to normal pancreatic tissue (soft). The interior of the cyst is partially green. B) The EUS mode-B image of a cystic lesion in the body of the pancreas in which the pancreatic parenchyma has a normal endosonographic aspect.
EUS elastography measures the magnitude of the strain produced by a given tissue; this strain is inversely proportional to the risk for malignancy, and so could aid in distinguishing between benign and malignant lesions.6
This technique has been used and developed mainly in European countries,7,8 with different sensitivities, specificities, and diagnostic precision for differentiating malignant tumors from benign ones. The combined results of 2 meta-analyses conducted by Asian groups that included 109 to 1310 studies for a total of 893 to 1,042 cases presenting with pancreatic masses in which EUS elastography was used reported an accumulated sensitivity of 95-98% (95% CI 93-100) and an accumulated specificity of 69% (95% CI 52-82) for differentiating between benign and malignant pancreatic masses, respectively. Both studies concluded that this is a minimally invasive technique and a promising method for evaluating pancreatic masses, as well as an effective complement to EUS-guided FNAB.
Our 2 cases presented with pathologies with completely different tissues in regard to elasticity, rigidity, and biologic nature. Similar to what has been reported,8,9 the malignant tissues were more rigid and were seen as blue areas, whereas healthy and/or benign tissues were green (figs. 1 and 2).
EUS elastography is a new endosonographic tool that objectively evaluates tissue elasticity and suggests the benign or malignant nature of lesions. Even though the current results are encouraging, diagnostic precision is modest,7,8 especially in differentiating tissues that have a similar rigidity but a different biology (chronic pancreatitis vs pancreatic cancer).4,7 At present it can be useful in cases with negative FNAB or as a guide for directing FNAB into zones that have a greater probability of malignancy (hard) and avoid necrotic tissue (soft). It cannot yet replace EUS-guided FNAB. Further studies are required that evaluate and determine the specific role of EUS elastography in the evaluation of solid pancreatic lesions.
Financial disclosureNo financial support was received in relation to this article. However, Medical Scope SA de CV and CT Scanner Lomas Altas temporarily loaned the Pentax EG-3870UTK echoendoscope and the Hitachi Preirus ultrasound console, respectively. No conditions were placed on the lending of the instruments and neither company participated in the elaboration of the present article.
Conflict of interestThe authors declare that there is no conflict of interest.
The authors wish to thank Medical Scope SA de CV, especially engineers Jorge Huerta and Karla Zavala, and CT Scanner Lomas Altas, especially Doctors Miguel Stoopen Rometi and Veronique Barois, for their collaboration and technical assistance in conducting the studies described in this article.
Please cite this article as: Peláez-Luna M, Romero F. Utilidad del ultrasonido endoscópico con elastografía en la evaluación y diferenciación de las lesiones pancreáticas. Revista de Gastroenterología de México. 2014;79:62–64.