The presence of papillary adenomatous polypoid lesions in the common bile duct is rare and the cases reported in the literature are associated with bile duct cysts.1,2 Because both entities are considered premalignant conditions, they should be resected. Surgical resolution is the usual option and there are few reports on endoscopic management.1 In addition, subcapsular hematoma of the liver and laceration of Glisson's capsule are uncommon complications of endoscopic retrograde cholangiopancreatography (ERCP).3–6 We present herein the case of distal bile duct adenoma not associated with biliary tract cysts, resolved through endoscopic polypectomy and complicated by subcapsular hematoma of the liver and Glisson's capsule laceration.
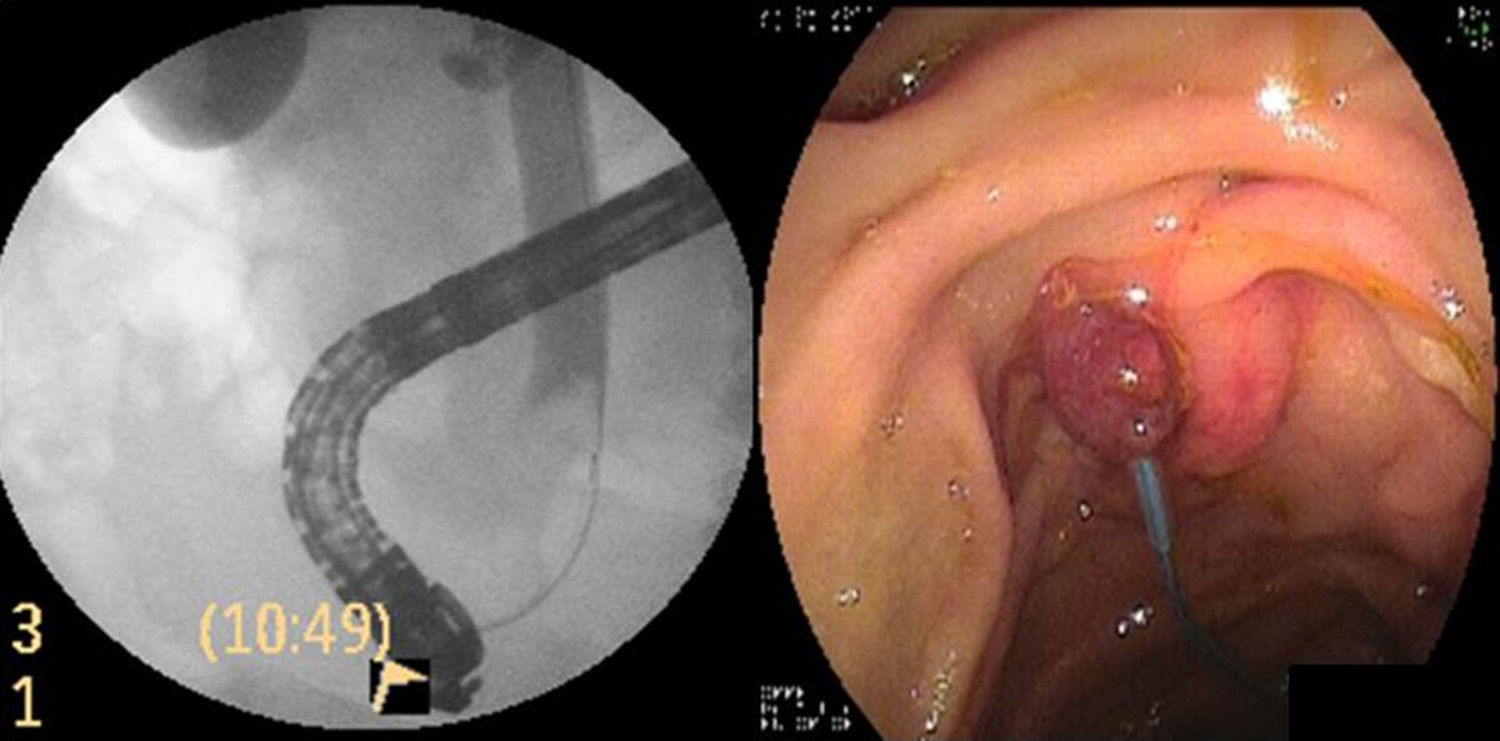
A 78-year-old man had a past history of chronic auricular fibrillation and mitral valve replacement and was under treatment with an anticoagulant (acenocoumarol). He was seen in medical consultation due to nonpainful jaundice of 3-week progression and laboratory tests with a pattern of cholestasis. Abdominal ultrasound showed dilation of the proximal bile duct with an endoluminal image in the distal bile duct. Cholangiography revealed a negative image at the level of the distal bile duct (Fig. 1). Sphincteropapillotomy was performed and a balloon extractor exteriorized a 12mm pedunculated lesion with a Kudo III mucosal pattern (consistent with adenoma) that was then biopsied. The decision was made to place a 10 Fr plastic biliary stent to ensure drainage and define the therapeutic conduct. The pathologic anatomy study reported papillary adenoma with low-grade dysplasia. The patient progressed with improved cholestasis.
Due to the abovementioned comorbidities, endoscopic treatment was performed. The anticoagulation medication was suspended.
During the procedure, the biliary tract was cannulated with a hydrophilic guidewire. Proximal migration of the plastic stent was observed and it was removed with a Dormia basket. The polypoid lesion was exteriorized with the balloon extractor, the pedicle was snared with an Endoloop® (Boston Scientific, Massachusetts, USA), and polypectomy was carried out with a diathermal loop (coagulation current) (Fig. 1).
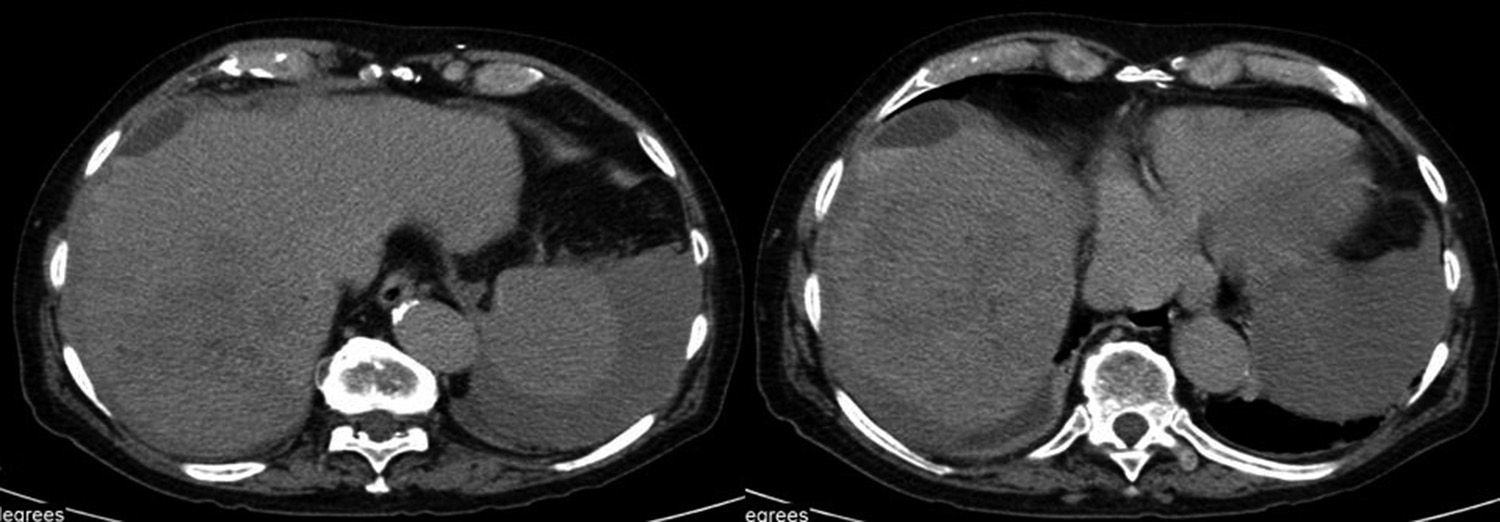
One hour after the endoscopy the patient complained of chills, abdominal pain in the right upper quadrant, and progressively intensifying ipsilateral shoulder pain. The patient then progressed to hypotension, hemodynamic instability, and a hematocrit value that decreased by 11 points. An abdominal computed axial tomography scan revealed hemoperitoneum and subcapsular hematoma of the liver (Fig. 2). Surgical intervention confirmed the tomographic findings, as well as laceration of Glisson's capsule with diffuse bleeding. Hemostasis was achieved through the liver packing technique. The patient was admitted to the Intensive Care Unit. He responded satisfactorily and was released 10 days later.
The pathologic anatomy study of the resected biliary tract tumor reported papillary adenoma with low-grade dysplasia and a lesion-free pedicle.
The patient had no disease recurrence or cholestasis during the 12-month control period after the resection.
Benign neoplasias of the biliary tract are rare and represent 6% of all tumors. They are classified as adenomas, papillomas, myoblastomas, adenomyomas, fibromas, leiomyomas, neurinomas, and hamartomas. In a review of 84 cases, 48% were papillomas and 46% were adenomas.7 In another report of 30 cases, 86% were adenomas or papillomas.8 The differential diagnosis must be made with choledocholithiasis, cholangiocarcinoma, ampulloma, and tumor of the pancreas. First-line treatment of this entity is surgical, given its association with biliary tract cysts and the premalignant condition of both. Pancreaticoduodenectomy is the surgical technique reported in the majority of cases. There are few reports on endoscopic resolution in the medical literature.9,10 Endoscopic treatment of our patient was chosen due to the lack of association with biliary tract cyst and the multiple comorbidities.
We believe that surgery should continue to be the first-line management if the patient's general medical condition allows it. Endoscopic management could be an option in those few patients in whom the absence of bile duct cyst has been confirmed through previous imaging studies.
Subcapsular hematoma of the liver is a rare complication of endoscopic cholangiography and hepatic laceration is even rarer. Certain authors state that the cause of subcapsular hematoma is the accidental puncture of the intrahepatic biliary tract with the guidewire.3–6 In our case, we used the guidewire during cannulation, but we also carried out the extraction procedure of the proximally migrated stent with a Dormia basket. We believe that these maneuvers could have caused the trauma to the liver parenchyma and Glisson's capsule. The patient had been receiving anticoagulation treatment, but it was correctly interrupted and the coagulation value was normal at the time of the endoscopy. The majority of patients progress favorably with general measures, antibiotic therapy, and strict hemodynamic control. Only some patients require surgery, percutaneous drainage, or arterial embolization. We decided upon the surgical approach for our patient, given the hemodynamic instability and the laceration of the hepatic capsule.
These types of complications should be suspected in patients that complain of abdominal pain, right shoulder pain, and hemodynamic instability after ERCP.
Financial disclosureNo financial support was received in relation to this article.
Conflict of interestThe authors declare that there is no conflict of interest.
Please cite this article as: Curvale C, Guidi M, Málaga I, Hwang HJ, Matanó R. Adenoma papilar de colédoco: patología infrecuente, resolución endoscópica novedosa, complicación rara. Reporte de un caso. Revista de Gastroenterología de México. 2016;82:109–111.