Irritable bowel syndrome (IBS) is one of the most frequent functional gastrointestinal disorders. Prevalence worldwide is estimated at 11%. There is little information on the prevalence of the other functional bowel disorders (FBDs). Our aim was to establish the prevalence of IBS and other FBDs according to the Rome IV criteria, in Uruguay.
Materials and methodsAn observational, population-based prevalence study was conducted. Data were collected through an online questionnaire, utilizing the Rome IV criteria.
ResultsOf the 1,052 participants (79% women, mean patient age 44 years), 47.2% met the Rome IV diagnostic criteria for at least one of the FBDs analyzed. Functional constipation (FC) was the most frequent, at 18.7% (16.4-21.1), followed by IBS at 17.1% (14.9-19.4) and functional diarrhea (FD) at 15.4% (13.3-17.6). IBS with constipation (IBS-C) was the most frequent IBS subtype (35%) and the IBS with diarrhea (IBS-D) subtype predominated in men. All FBDs were more prevalent in women and youths. Of the survey participants with a FBD, 59% stated that they perceived no worsening of their symptoms related to the COVID-19 pandemic.
ConclusionsOurs is the first prevalence study on FBDs conducted on the Uruguayan general population. Half of the participants surveyed presented with a FBD analyzed in the study. FC was the most frequent, followed by IBS and FD. The prevalence rate of IBS was the highest, based on the Rome IV diagnostic criteria, and constipation was the most frequent subtype.
El síndrome de intestino irritable (SII) es uno de los trastornos gastrointestinales funcionales más frecuentes. La prevalencia global se estima en 11%. Es escasa la información sobre la prevalencia de los demás trastornos funcionales intestinales (TFI). El objetivo fue establecer la prevalencia de SII y otros TFI según criterios de Roma IV en Uruguay.
Materiales y métodosSe realizó un estudio observacional de prevalencia de base poblacional. Se recogieron los datos mediante un cuestionario online, utilizando criterios diagnósticos Roma IV.
ResultadosDe los 1052 participantes (79% mujeres, media de edad 44 años), 47.2% cumplían criterios diagnósticos Roma IV para al menos uno de los TFI estudiados. Estreñimiento funcional (EF) fue el más frecuente con 18.7% (16.4-21.1), seguido de SII 17.1% (14.9-19.4) y por último diarrea funcional (DF) con 15.4% (13.3-17.6). El subtipo de SII más prevalente fue SII subtipo estreñimiento (35%), en hombres predominó SII subtipo diarrea. Todos los TFI fueron más prevalentes entre mujeres y jóvenes. De los encuestados con TFI, 59% referían no percibir que la pandemia por COVID-19 haya generado una peoría de sus síntomas.
ConclusionesEste es el primer estudio de prevalencia de TFI en la población general de Uruguay. La mitad de la muestra presentó alguno de los TFI estudiados. EF fue el más frecuente, seguido de SII y DF. La tasa de prevalencia de SII detectada fue la más alta reportada usando criterios diagnósticos Roma IV y estreñimiento fue el subtipo más frecuente.
Irritable bowel syndrome (IBS) is one of the most frequent functional gastrointestinal disorders. Prevalence worldwide is estimated at 11%, although it is probably underdiagnosed, given the heterogeneity among different regions, cultures, and ethnicities.1,2
IBS is one of the functional bowel disorders (FBDs) that encompass a spectrum of chronic gastrointestinal disorders characterized by abdominal pain, bloating and/or intestinal abnormalities. FBDs are defined by the Rome criteria (currently Rome IV) and include IBS, functional constipation (FC), functional diarrhea (FD), functional abdominal bloating/distension, unspecified bowel disorders, and opioid-induced constipation. There is significant overlapping of those conditions and they should be considered a continuum, as opposed to isolated disorders.3,4
The pathophysiology of IBS and FBDs is not fully understood. Different complementary mechanisms have been proposed, such as visceral hypersensitivity, motility alterations, microbiota-gut-brain axis dysfunction, low-grade inflammation, and dysbiosis.1,5,6
Prevalence studies that have evaluated FBDs are scarce and report greatly varying results. Recently, the Rome Foundation carried out a global prevalence study on FBDs that included 33 countries, using unified diagnostic criteria. Those authors found that FBDs are frequent, with a prevalence of 40.7%; the most frequent FBD was FC (11.7%), the prevalence of IBS was 4.1%, and the prevalence of FD was 4.7%.7
There are very few prevalence studies on IBS in Latin America. In Uruguay, a single study conducted in a neighborhood of Montevideo found a prevalence of 10.9%, utilizing Rome II criteria.8 With those same diagnostic criteria, Chile was found to have the highest prevalence in Latin America (28.6%).9 Prevalence was 16.9% in Mexico.10 Applying the Rome III criteria, prevalence was 15% in Peru and 16.8% in Venezuela.11,12
A systematic review and meta-analysis conducted by Suares and Ford identified a pooled prevalence of FC of 14% (Rome I, II, and III criteria). The highest prevalence was in South America (18%).13 At present, there are no prevalence studies on chronic constipation or FC in Uruguay.
The prevalence of FD has not been widely studied. One Taiwanese study conducted by Chang et al. on the prevalence of FBDs, using the Rome III criteria, identified a low prevalence of FD (2.2%), affecting more men than women.14
Palsson et al. compared the prevalence rates of FD, using the Rome III and IV criteria, and found a greater prevalence with the Rome IV criteria (4.7%).15
Chronic stress is a factor to consider in FBD symptom onset and exacerbation, especially in IBS.3,4,7 The rapid propagation of the coronavirus disease (COVID-19) has had an emotional and neuropsychologic impact. An intensification of existing psychologic disorders has been observed, along with the development of new disorders (anxiety, depression, alcohol abuse, and panic).16,17
The aim of the present study was to establish the prevalence of IBS and other FBDs in Uruguay, as well as the impact of the COVID-19 pandemic on individuals with FBDs.
Materials and methodsStudy characteristicsAn observational, descriptive, cross-sectional, population-based prevalence study was conducted.
MethodologyThe data were collected from an online questionnaire, created using Google Forms and disseminated on social networks (WhatsApp, Facebook, Instagram, Twitter). The survey was available for use from May 25 to June 22, 2021.
Sample sizeSample size was calculated in OpenEpi, taking into account the total population of Uruguay, according to the 2011 census (data retrieved from the National Statistics Institute [INE, the Spanish acronym]).18 For a 95% confidence interval and an estimated prevalence of IBS of 10% and 20%, a minimum sample size of 139 and 246 individuals, respectively, was established.
The percentage of inhabitants per department was considered for establishing an objective minimum number of participants for each department, to achieve a representative sample size of each Uruguayan territory.
Statistical analysisAll the eligible questionnaires were numbered according to the order in which they were filled out. The data were processed utilizing OpenEpi, version 3 software.
The summary measures of ratio and proportion were utilized to analyze the qualitative variables and statistical significance was set at a p < 0.05.
The demographic data of age, sex, department of origin, and educational level were obtained.
The Rome IV questionnaire, validated in Argentina in Spanish, was utilized to collect data and define the cases of IBS, FC, and FD.
The inclusion criteria were Uruguayan nationality, age above 18 years, and acceptance to participate in the study.
The exclusion criteria were a personal medical history of celiac disease, gastrointestinal cancer, inflammatory bowel disease (IBD), colonic diverticulosis, or intestinal resection.
Ethical considerationsThe study complied with the norms of the CIOMS and the Declaration of Helsinki and was approved by the Ethics Committee of the Hospital de Clínicas de Uruguay.19
A written statement of informed consent was explained to each patient, describing his/her participation, study aims, and confidentiality criteria for managing his/her personal data.
ResultsGeneral sample characteristicsDuring the period in which the survey was available (May 25 to June 22, 2021), 1,362 persons participated. Thirteen participants were excluded because they were foreigners, 11 because they were under 18 years of age, and 2 because they chose the option to not participate. An additional 284 (21%) participants were excluded due to having a history of organic disease.
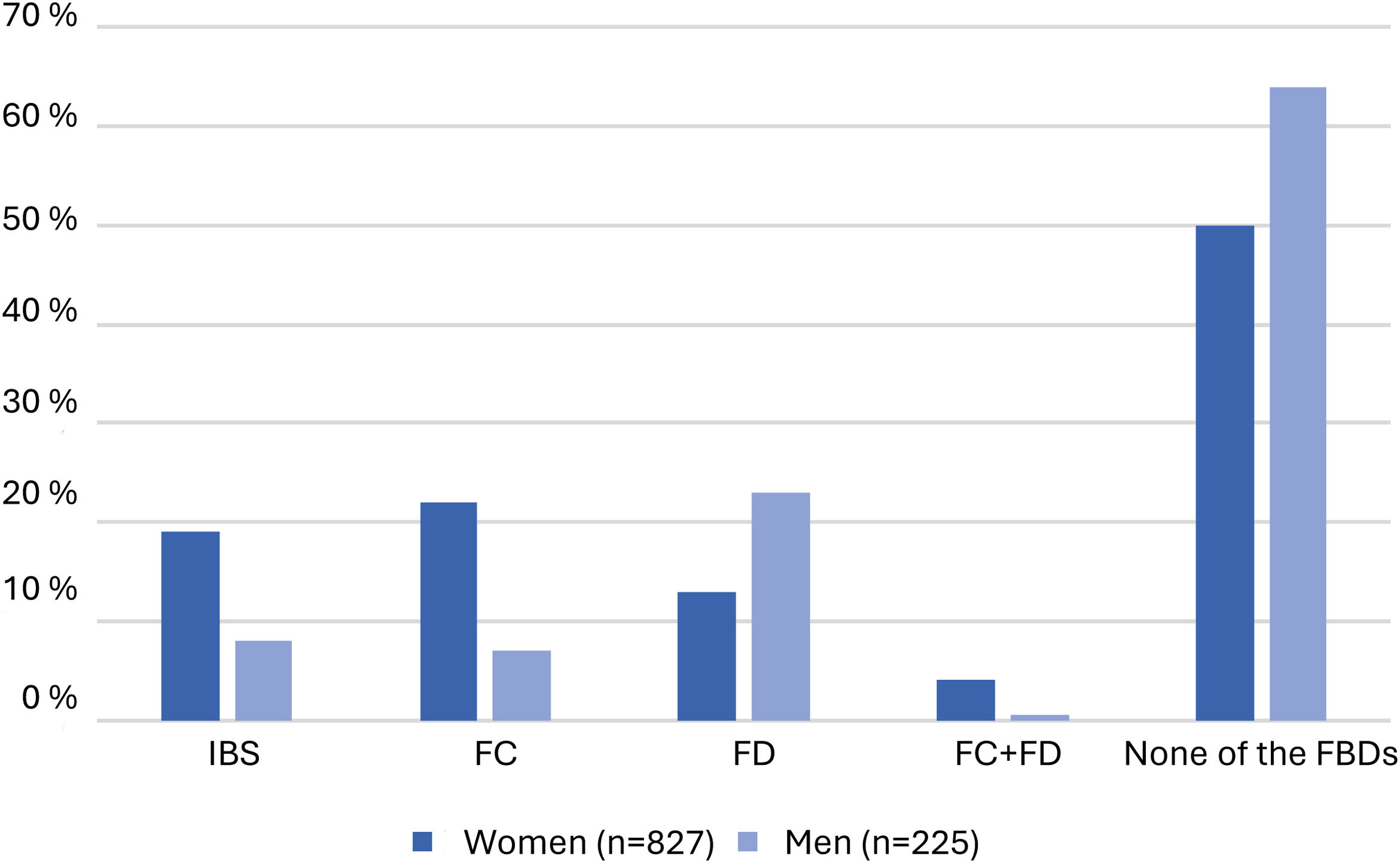
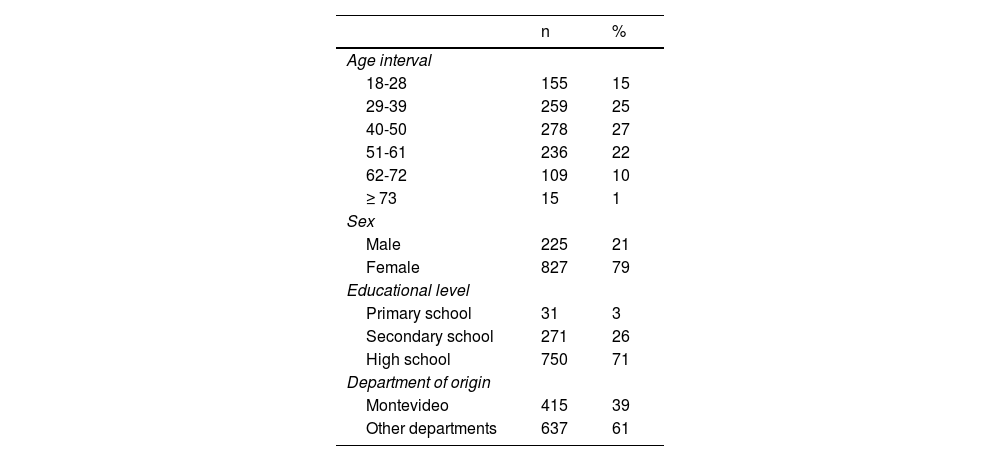
The sample size was 1,052 and 827 of the participants were women (79%). Mean patient age was 44 years (18-83); 66% (692 individuals) were 50 years old or younger and 34% (360 individuals) were over 50 years of age. The majority of the individuals surveyed (71%) had a high school education. With respect to department of origin, 39% of the participants were from Montevideo (Table 1).
Demographic characteristics (n = 1,052).
| n | % | |
|---|---|---|
| Age interval | ||
| 18-28 | 155 | 15 |
| 29-39 | 259 | 25 |
| 40-50 | 278 | 27 |
| 51-61 | 236 | 22 |
| 62-72 | 109 | 10 |
| ≥ 73 | 15 | 1 |
| Sex | ||
| Male | 225 | 21 |
| Female | 827 | 79 |
| Educational level | ||
| Primary school | 31 | 3 |
| Secondary school | 271 | 26 |
| High school | 750 | 71 |
| Department of origin | ||
| Montevideo | 415 | 39 |
| Other departments | 637 | 61 |
Of the 1,052 questionnaires analyzed, and according to the Rome IV diagnostic criteria, 17.1% (14.9-19.4) of the participants had IBS, 18.7% (16.4-21.1) had FC, and 15.4% (13.3-17.6) had FD. There was FD and FC overlap, with 43 (4.1%) of the participants meeting the criteria for both. A diagnosis of the FBDs analyzed could not be made in 556 individuals (52.8%).
The most frequent FBD by sex was FC (n = 181, 21%), followed by IBS (n = 161, 18%) in women. In men, the most frequent FBD was FD (n = 51, 22%), followed by IBS (n = 19, 8%) (Fig. 1).
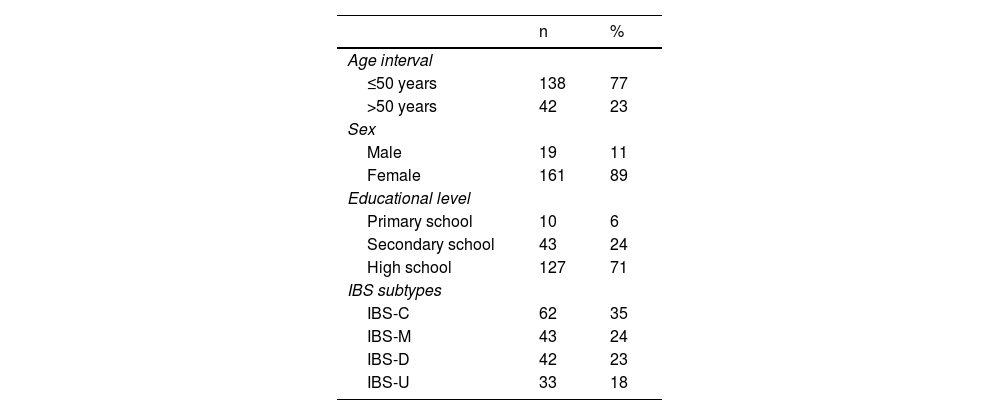
Irritable bowel syndromeThe total number of participants that met the IBS criteria was 180 and 161 of them were women (89%). Mean patient age was 41 years (18-70) and 77% were 50 years old or younger (Table 2). An increase in prevalence was observed up to 50 years of age, with a decrease in older ages. No cases were identified in the range of 73 to 83 years of age.
Characteristics of the population with IBS (n = 180).
| n | % | |
|---|---|---|
| Age interval | ||
| ≤50 years | 138 | 77 |
| >50 years | 42 | 23 |
| Sex | ||
| Male | 19 | 11 |
| Female | 161 | 89 |
| Educational level | ||
| Primary school | 10 | 6 |
| Secondary school | 43 | 24 |
| High school | 127 | 71 |
| IBS subtypes | ||
| IBS-C | 62 | 35 |
| IBS-M | 43 | 24 |
| IBS-D | 42 | 23 |
| IBS-U | 33 | 18 |
IBS: irritable bowel syndrome; IBS-C: irritable bowel syndrome with constipation; IBS-D: irritable bowel syndrome with diarrhea; IBS-M: irritable bowel syndrome mixed; IBS-U: irritable bowel syndrome unclassified.
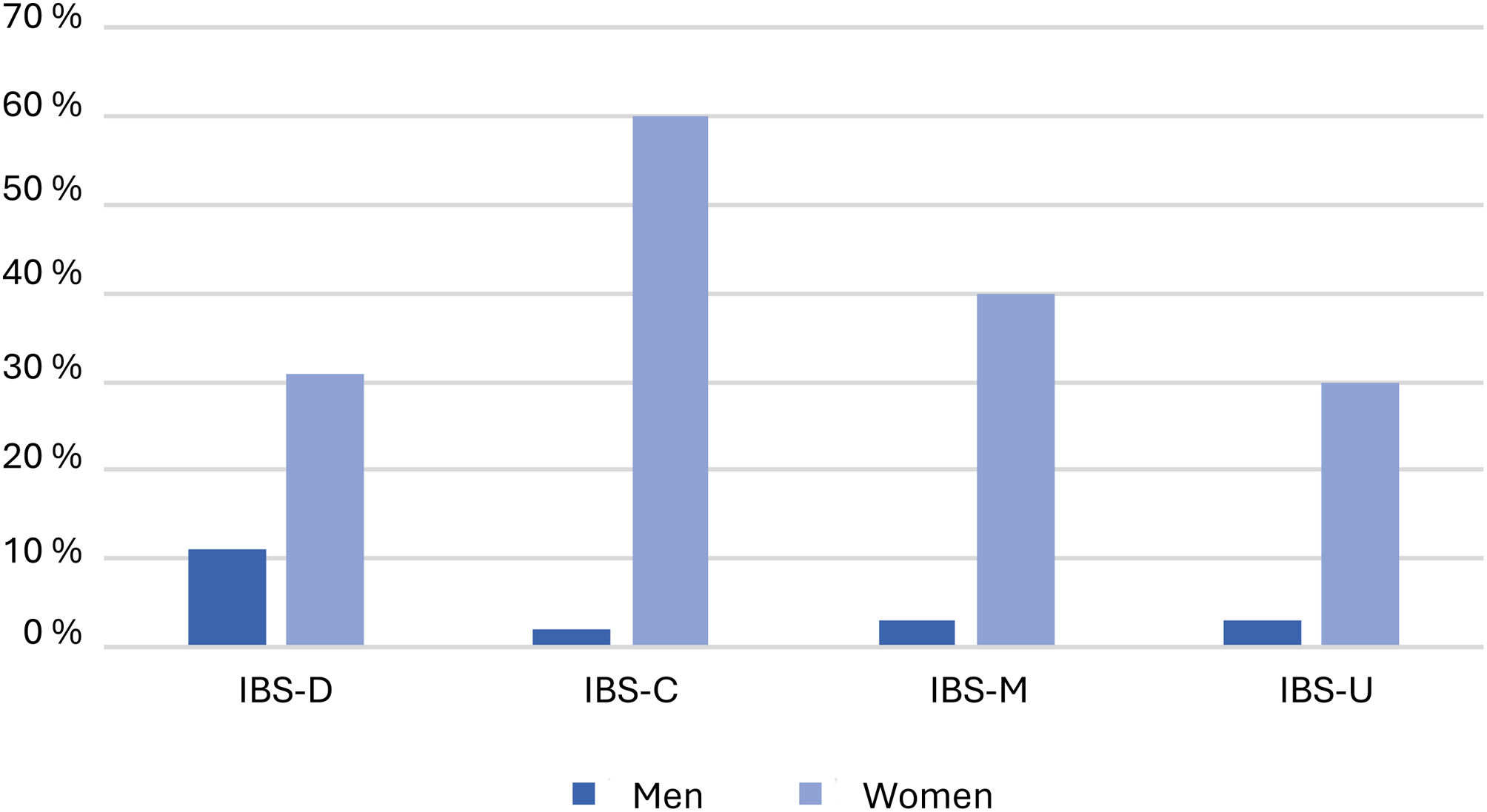
With respect to IBS subtypes, IBS with constipation (IBS-C) was the most prevalent (35%), followed by IBS mixed (IBS-M) (24%) and IBS with diarrhea (IBS-D) (23%). In analyzing the subtypes by sex, IBS-D was the most frequent subtype in men, whereas IBS-C predominated in women (Fig. 2).
The majority of participants with IBS responded that they had experienced pain within the past 10 days (89%), and of those individuals, 13% presented with pain every day for the past 10 days. Fifty-two participants (29%) had continuous or almost continuous abdominal pain.
When asked about abdominal pain intensity, it was moderate-to-severe for 88 individuals (49%) and mild for 92 (51%).
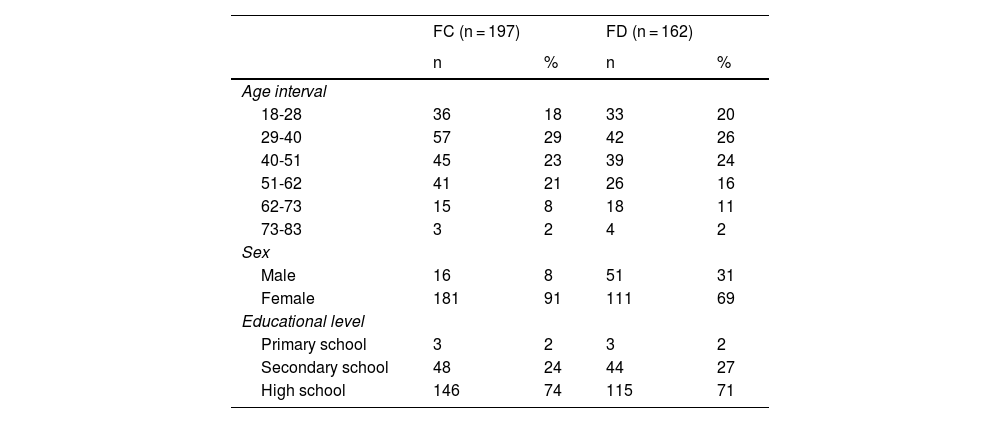
Functional constipation and functional diarrheaThe FC group (197 individuals) had a mean age of 42 years (18-77) and 181 (92%) were women. Mean age of the participants with FD was 43 years (18-77) and 111 (69%) were women. There was FD and FC overlap in 4.1% of the participants. A high school education was predominant in the two groups (Table 3).
Characteristics of the populations with functional constipation (FC) and functional diarrhea (FD).
| FC (n = 197) | FD (n = 162) | |||
|---|---|---|---|---|
| n | % | n | % | |
| Age interval | ||||
| 18-28 | 36 | 18 | 33 | 20 |
| 29-40 | 57 | 29 | 42 | 26 |
| 40-51 | 45 | 23 | 39 | 24 |
| 51-62 | 41 | 21 | 26 | 16 |
| 62-73 | 15 | 8 | 18 | 11 |
| 73-83 | 3 | 2 | 4 | 2 |
| Sex | ||||
| Male | 16 | 8 | 51 | 31 |
| Female | 181 | 91 | 111 | 69 |
| Educational level | ||||
| Primary school | 3 | 2 | 3 | 2 |
| Secondary school | 48 | 24 | 44 | 27 |
| High school | 146 | 74 | 115 | 71 |
Postprandial diarrhea (50% of bowel movements or more) presented in 80 individuals (49%). Sixty-nine percent of the participants experienced fecal urgency in some of their bowel movements.
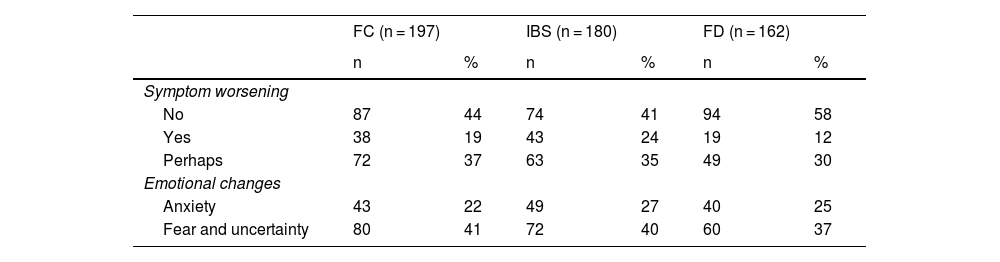
Impact of the COVID-19 pandemicWith respect to emotional changes resulting from the pandemic, anxiety was the most frequent, followed by fear and uncertainty. Fifty-nine percent of participants perceived no worsening of their symptoms related to the pandemic. In the IBS subgroup, 43 persons (24%) identified a worsening of their symptoms, and feelings of anxiety and fear and uncertainty were the most reported (Table 4).
Symptoms and emotional changes related to the COVID-19 pandemic.
| FC (n = 197) | IBS (n = 180) | FD (n = 162) | ||||
|---|---|---|---|---|---|---|
| n | % | n | % | n | % | |
| Symptom worsening | ||||||
| No | 87 | 44 | 74 | 41 | 94 | 58 |
| Yes | 38 | 19 | 43 | 24 | 19 | 12 |
| Perhaps | 72 | 37 | 63 | 35 | 49 | 30 |
| Emotional changes | ||||||
| Anxiety | 43 | 22 | 49 | 27 | 40 | 25 |
| Fear and uncertainty | 80 | 41 | 72 | 40 | 60 | 37 |
FC: functional constipation; FD: functional diarrhea; IBS: irritable bowel syndrome.
Ours is the first prevalence study on FBDs conducted in Uruguay that applied the Rome IV diagnostic criteria. Even though the survey was carried out on volunteers, through an online questionnaire, the age distribution of the sample population was representative, given its similarity to the distribution in the latest national census (11% above 60 years of age, 40% between 18 and 40 years of age, and 49% between 41 and 60 years of age).
Nevertheless, distribution by sex was not representative because the proportion of women was 79%, which could constitute bias due to the fact that women have a higher prevalence of FBDs. Likewise, the majority of the population had a high school education (71%) or secondary school education (26%), which could guarantee better comprehension of the questionnaire, but also be regarded as a risk factor for developing the disorders analyzed and overestimate prevalence.
The prevalence of IBS, according to the Rome IV criteria, was 17.1%, considerably higher than that reported in other studies, at both the regional and global levels. The latest survey by the Rome Foundation, using those same criteria, found a prevalence of 4.1%.7 In a recent meta-analysis, the pooled prevalence of 6 studies that applied the Rome IV criteria was 3.8%.20 In Uruguay, a single epidemiologic study conducted in 2003 on a selected population from Montevideo found a prevalence of 10.9%, utilizing the Rome II criteria, which was lower than that reported by countries of the region, using the same criteria.8–10
The higher prevalence of IBS in our study could be explained by the predominance of women and the high educational level. Chronic stress (more frequent in students and workers) has been proposed as a triggering factor.3,4,10,12 Obtaining information from self-administered surveys could also justify the difference, given that such surveys have been associated with higher prevalence, compared with interviewer-administered surveys.7,20
According to the Rome Foundation survey, the differences in regions could be explained by different dietary habits, cultures, or geographic conditions. However, it is difficult to attribute the gap found in our study to those variables. For example, there are populational similarities between Argentina and Uruguay, but prevalence in Argentina is 3.5%.
By analyzing men and women as separate groups, the prevalence of IBS was 8% and 18%, respectively. Even though the prevalence of IBS was lower in men, it was not negligible, and was higher than that reported in previous studies.7,20
The majority of the participants with IBS were 50 years old or younger, and a decrease in prevalence in older individuals was observed, as has been reported by other researchers.1,7,10,11,15 Likewise, IBS-C (35%) was the most frequent subtype, followed by IBS-M (24%), as has been reported internationally.7 Studies utilizing the Rome II and Rome III criteria showed greater heterogeneity, with respect to the different subtypes, and a recent meta-analysis conducted by Oka et al. established the mixed subtype as the most frequent, followed by IBS-D.1,20
As has been shown in previous studies, we found that IBS subtypes were different in women and men: IBS-C predominated in women and IBS-D was more frequent in men.1,7,20
FC was the most frequent FBD, with a prevalence of 18.7%, which is higher than that reported in the Rome Foundation survey (11.7%).7 Palsson et al. compared the prevalence rates using the Rome II and Rome IV criteria and described a higher prevalence with the Rome IV criteria (7.6%).15 The change of diagnostic criteria was suggested to have possibly determined a migration of previously categorized IBS patients to FC or FD, due to the higher threshold in the frequency of abdominal pain needed for diagnosing IBS.5,15 Nevertheless, a systematic review and meta-analysis conducted by Suares and Ford identified a prevalence of FC of 14% with the Rome I, II, or III criteria, indicating the high prevalence with the earlier Rome criteria.13
The prevalence rates of FC are variable and there are no previous prevalence studies in Uruguay. The high prevalence of FC in our study is in line with the high prevalence of the other FBDs analyzed, and as in other studies, FC was the most frequent FBD.7,15
The prevalence of FC increased with age up to 62 years, with a lower frequency observed in individuals above 60 years of age, a finding similar to the results reported by the Rome Foundation and Palsson et al.7,15 Earlier studies that utilized criteria other than the Rome IV criteria found a higher prevalence in the older age groups, considering advanced age a risk factor.13,15 The fact that the Rome IV FC rates are higher in younger groups is surprising and could signify a change in the age pattern of presentation, with implications for future studies.
We found a higher prevalence of FD than that reported in other studies (15.4% vs. 4.7%).7,15 A significantly lower prevalence was described using the Rome III criteria, reflecting the impact of lowering the frequency threshold of diarrhea stools in the Rome IV criteria (25% of all stools), compared with the Rome III criteria (75% of all stools).15
With respect to the differences in the prevalence rate by sex, Palsson et al. identified no differences and the Rome Foundation study showed a slight predominance in men.7,15 FD was the most prevalent FBD in men in our study.
Age distribution was similar to that reported in international studies.1,7,15 Of the survey participants, 4.1% had FD and FC overlap, reaffirming the concept that those conditions should be considered a continuum, rather than isolated disorders.3,4
Regarding the effect of the COVID-19 pandemic on the FBDs, the majority of the participants identified no worsening of their symptoms. Researchers studying said effect have found conflicting results.21,22 That heterogeneity can be explained by different social distancing measures and the varying economic impact, according to each country.
The methodological strengths of our study were: a) it is the first study to evaluate the prevalence of FBDs in Uruguay, utilizing the Rome IV criteria; b) the use of a Rome IV questionnaire validated in Spanish in Argentina, a country with the same language and similar culture as Uruguay, and so the questions were clear for the participants; and c) a broad sample size with age group and geographic distribution representativeness.
The weaknesses were: a) female predominance in the sample, which could have affected the prevalence rates; b) the participants knew the gastroenterologic focus of the survey prior to taking it, possibly signifying that more persons with gastrointestinal symptoms were interested in participating; c) response quality control measures were not included; d) surveys conducted through online questionnaires exclude a small sector of the population that does not have access to or know how to use them; and e) there were no items regarding alarm symptoms or opioid consumption.
ConclusionsThe present analysis is the first prevalence study on FBDs conducted in Uruguay, as well as the first study on IBS with a national scope. Half of the sample presented with an FBD included in the study, and FC was the most frequent. The prevalence rate of IBS was higher than that reported worldwide, using the Rome IV criteria. No impact from the COVID-19 pandemic was found, with respect to a worsening of symptoms.
Financial disclosureNo financial support was received in relation to this study.
Conflict of interestThe authors declare that there is no conflict of interest.