Functional constipation and irritable bowel syndrome with constipation are highly prevalent and affect the quality of life of those who suffer from them.
AimsTo evaluate quality of life in patients with functional constipation and irritable bowel disease in accordance with the Rome III criteria, using the PAC-QOL and SF-36 questionnaires.
Materials and methodsA cross-sectional study was conducted using self-administered questionnaires. The PAC-QOL, SF-36, and Rome III constipation module questionnaires were applied to patients that complained of constipation at the outpatient clinic of a tertiary care hospital. The constipation subtypes were: functional constipation (no pain), irritable bowel syndrome with constipation (pain and/or discomfort≥3days/month), and unclassifiable constipation (pain≤2days/month). Data were summarized in proportions, and group comparisons were made between the scores of each of the areas of the PAC-QOL and SF-36 questionnaires using parametric tests (Student's t test and ANOVA).
ResultsA total of 43 PAC-QOL surveys were analyzed, resulting in cases of irritable bowel syndrome with constipation (14%), functional constipation (37%), and unclassifiable constipation (49%). There were statistically significant differences (P<.05) in Physical discomfort (irritable bowel syndrome with constipation vs functional constipation and unclassifiable constipation vs irritable bowel syndrome with constipation), Worries and concerns (irritable bowel syndrome with constipation vs functional constipation), and Treatment satisfaction (irritable bowel syndrome with constipation vs functional constipation and unclassifiable constipation vs irritable bowel syndrome with constipation). A total of 93 SF-36 questionnaires were analyzed, describing cases of irritable bowel syndrome with constipation (23%), functional constipation (27%), and unclassifiable constipation (51%). Lower physical energy was found in relation to irritable bowel syndrome with constipation vs functional constipation (P<.0221) and unclassifiable constipation (P<.0086), respectively, and there was greater physical pain in the cases of irritable bowel syndrome with constipation vs unclassifiable constipation (P<.0362).
ConclusionsDifferences in quality of life of patients presenting with constipation subtypes were identified using the PAC-QOL and SF-36 questionnaires. The patients that had the irritable bowel syndrome with constipation subtype experienced poorer quality of life in all the evaluated domains.
El estreñimiento funcional y el síndrome de intestino irritable con estreñimiento son altamente prevalentes y generan alteración en la calidad de vida de quienes los padecen.
ObjetivosEvaluar la calidad de vida en pacientes con estreñimiento funcional y síndrome de intestino irritable, de acuerdo a los criterios de ROMA III, utilizando cuestionarios: PAC-QOL y SF-36.
Materiales y métodosEstudio transversal tipo encuesta autoadministrado. Se aplicó PAC-QOL, SF-36 y cuestionario modular de estreñimiento ROMA III a pacientes con queja de estreñimiento en la consulta externa de un hospital de tercer nivel. Los subtipos de estreñimiento fueron: estreñimiento funcional (sin dolor), síndrome de intestino irritable con estreñimiento (dolor y/o malestar≥3días/mes) y estreñimiento no clasificable (dolor≤2días/mes). Los datos se resumen en proporciones, y se realizaron comparaciones entre la puntuación de cada uno de los rubros de ambos cuestionarios entre los grupos utilizando pruebas paramétricas (t-Student y ANOVA).
ResultadosSe analizaron 43 encuestas PAC-QOL, síndrome de intestino irritable con estreñimiento (14%), estreñimiento funcional (37%) y estreñimiento no clasificable (49%), encontrándose diferencia estadísticamente significativa (p<0.05) en Malestar físico (síndrome de intestino irritable con estreñimiento vs. estreñimiento funcional y estreñimiento no clasificable vs. síndrome de intestino irritable con estreñimiento), Preocupaciones (síndrome de intestino irritable con estreñimiento vs. estreñimiento funcional) y Satisfacción con el tratamiento (síndrome de intestino irritable con estreñimiento vs. estreñimiento funcional y estreñimiento no clasificable vs. síndrome de intestino irritable con estreñimiento). Se analizaron 93 encuestas SF-36, síndrome de intestino irritable con estreñimiento (23%), estreñimiento funcional (27%) y estreñimiento no clasificable (51%), encontrándose menor energía física entre síndrome de intestino irritable con estreñimiento vs. estreñimiento funcional (p<0.0221) y estreñimiento no clasificable (p<0.0086) respectivamente, y mayor dolor físico al compararse con síndrome de intestino irritable con estreñimiento vs. estreñimiento no clasificable (p<0.0362).
ConclusionesUtilizando los cuestionarios PAC-QOL y SF-36 se identifican diferencias en la calidad de vida en los subtipos de estreñimiento. Los pacientes con la variante síndrome de intestino irritable con estreñimiento experimentan menor calidad de vida en todos los dominios evaluados.
Functional constipation (FC) and irritable bowel syndrome (IBS) are 2 diseases that present frequently in the population1 and they have an impact on the quality of life of the patients that suffer from them.2
The prevalence of FC has been estimated at 5-25% and a recent meta-analysis has calculated it at 14.4% in the Mexican population.3 The worldwide prevalence of IBS is from 10 to 20% and is approximately 16% in Mexico.4
Patients with chronic disorders not only suffer from physical pain, but they are also affected socially and psychologically.5 Patients that present with functional gastrointestinal disorders, especially FC and IBS, have been shown to experience poorer quality of life.2 Several studies have demonstrated these findings, particularly in patients with an FGID that present with moderate to severe symptoms. Lower quality of life scores have been observed in patients with IBS, when compared with other diseases such as asthma, and similar scores have been reported when compared with chronic diseases.6
In general, constipation has an important impact on the quality of life of those that present with it, regardless of culture or nationality. It also has a predominant effect in areas of mental health, compared with other chronic conditions such as osteoarthritis and diabetes mellitus.7
The evaluation of quality of life in patients with FC and IBS is a tool through which the effect of these diseases on physical and emotional aspects can be recognized. Previous studies have reported that these disorders cause greater school and work absenteeism, as well as loss of productivity.2,8,9
Significant differences in the physical and emotional domains of the SF-12 questionnaire have been reported in patients presenting with chronic constipation, when compared with subjects that do not have this problem.1 The SF-36 questionnaire has been used in different studies for determining overall quality of life in patients with FC and IBS. Statistical differences have also been shown in all the domains of the SF-36 between IBS patients and healthy subjects, in each of the 8 scales measured by this tool.10
Due to the prevalence and symptomatic nature of chronic constipation, systematized evaluations are particularly important in order to have better long-term understanding and management of these patients.11
The Patient Assessment of Constipation-Quality of Life (PAC-QOL) is a 28-item questionnaire that has recently been developed for the specific evaluation of quality of life in patients presenting with constipation.11 It has been used to assess patients with constipation in phase III studies that have been carried out to analyze new prokinetic drugs for the treatment of this disorder.12
The Rome III criteria facilitate the diagnosis of functional gastrointestinal disorders, including FC and IBS with constipation (IBS-C).13 In the Rome III questionnaire constipation module, the first question is: “In the last 3 months, how often have you had discomfort or pain in some part of the abdomen?” This question separates the two problems by referring to the presence of abdominal discomfort or pain and the answer ranges from “Never” to “Every day”. According to the answer, it is possible to determine whether the patient has FC or IBS-C. However, there is a group of patients that presents with pain, but does not fit the IBS or FC criteria, and thus they are described as patients with unclassifiable constipation.
At present, there is no study that analyzes quality of life with both general and specific questionnaires in patients with constipation and its different subclassifications based on the Rome III criteria. Therefore, the aim of our study was to evaluate quality of life in patients with chronic constipation and its variants according to the Rome III criteria using a general questionnaire (SF-36) and a specific one (PAQ-QOL).
MethodsPopulationA cross-sectional study, employing a survey, was carried out within the time frame of April 29 and June 19, 2014. Only patients complaining of constipation that were encountered in the waiting room of the outpatient clinic of the Internal Medicine and Gastroenterology Departments of the Instituto Nacional de Ciencias Médicas y Nutrición Salvador Zubirán were invited to participate. The study was approved by the Ethics Committee of the Institute and all patients gave statements of informed consent before taking part in the survey.
DefinitionsInitially, the Spanish version of the Rome III questionnaire constipation module was applied to all the patients that were waiting to have their outpatient consultation and that answered the question “Do you suffer from constipation?” affirmatively. Afterwards the Spanish versions of the self-administered PAC-QOL and SF-36 version 2 questionnaires were applied.
Constipation was considered to be present if the patient had 2 of the following 6 Rome III constipation symptoms: 1) straining during at least 25% of defecations, 2) lumpy stools in at least 25% of defecations, 3) sensation of incomplete evacuation in at least 25% of defecations, 4) sensation of anorectal obstruction/blockage in at least 25% of defecations, 5) manual maneuvers to facilitate at least 25% of defecations, and 6) bowel movements ≤ 3 times a week. Patients were regarded as having constipation if they presented with 2 of these 6 symptoms and if symptom onset was ≥ 6 months.
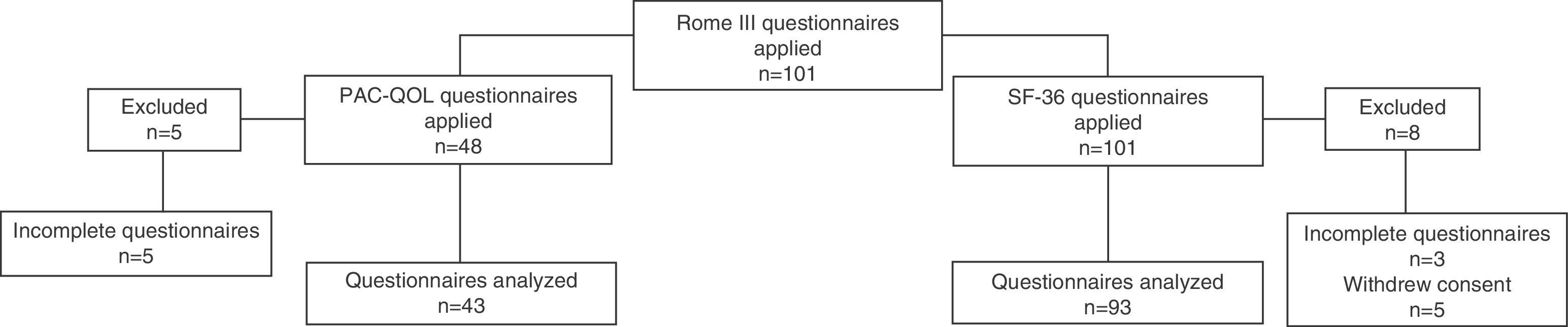
According to the answer to the first question of the Rome III constipation module, “In the last 3 months, how often have you had discomfort or pain in some part of the abdomen?”, the patients were classified as follows: 1) FC, if the answer was “0” (“Never”) in addition to having 2 or more of the 6 constipation symptoms, 2) IBS-C, if the answer was “≥ 3” (presence of abdominal discomfort or pain “2 or 3 days a month”, “Once a week”, “More than once a week”, or “Every day”) and the presence of 2 or more of the 6 constipation symptoms, and 3) unclassifiable constipation, if the answer was “1 and 2” (presence of abdominal discomfort or pain “Less than once a month”, or “Once a month”), without meeting the criteria for IBS or FC, but having at least 2 of the 6 constipation symptoms. Figure 1 shows a flow diagram that explains the questionnaire application process in the patients with constipation.
Quality of life (PAC-QOL and SF-36)The PAC-QOL questionnaire consists of 28 items grouped into 4 subscales: a) Physical Discomfort, b) Psychosocial Discomfort, c) Worries and Concerns, and d) Treatment Satisfaction. Scoring was done on a Likert 5-point scale from 0 (Nothing/Never) to 4 (Extremely/Always) in which a lower score reflected a better quality of life.11
The SF-36 questionnaire evaluates quality of life in adult populations (above 16 years of age) and is made up of 36 items that assess: a) Physical Function, b) Physical Limitation, c) Emotional Limitation, d) Emotional Well-being, e) Bodily Pain, f) Fatigue/Energy, g) Social Function, and h) General Health. Each subscale has a score from 0 to 100, in which the higher score is equivalent to a better health status.14,15
From the total number of PAC-QOL questionnaires applied, 5 were eliminated because they were incomplete and from the total of the SF-36 questionnaires applied, 8 were eliminated; 3 because they were incomplete and 5 because the participant withdrew his or her consent to participate in the study (fig. 1).
Statistical analysisThe continuous variables were summarized as means and the categorical variables as percentages. The different constipation subtype scores were compared through parametric statistics for each of the areas of the PAC-QOL and SF-36 questionnaires (Student's t test and ANOVA), using the GraphPad Prism Version 5.03 statistical package.
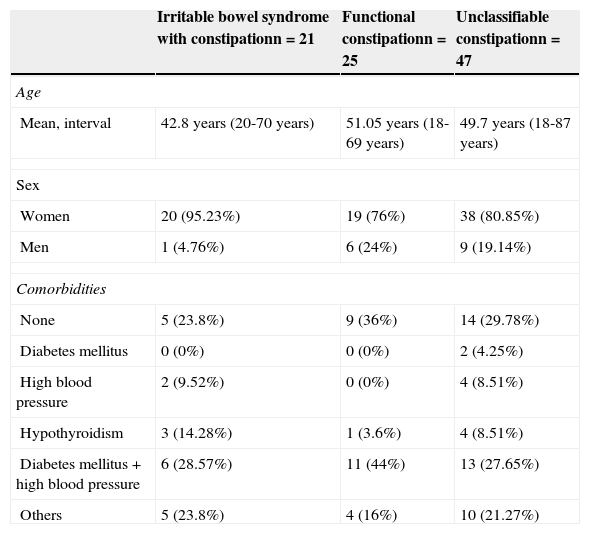
ResultsA total of 101 patients answered the Rome III questionnaire constipation module for constipation diagnosis. Figure 1 shows the number of PAC-QOL and SF-36 questionnaires applied. The mean length of time it took to answer the 3 questionnaires was 25min. A total of 101 questionnaires were applied and the patient age range was from 18 to 87 years (a mean of 48.72); 77 were women and 16 were men. Table 1 shows the demographic data.
Demographic characteristics of the patients, according to the groups studied: irritable bowel syndrome with constipation, functional constipation, and unclassifiable constipation.
| Irritable bowel syndrome with constipationn=21 | Functional constipationn=25 | Unclassifiable constipationn=47 | |
|---|---|---|---|
| Age | |||
| Mean, interval | 42.8 years (20-70 years) | 51.05 years (18-69 years) | 49.7 years (18-87 years) |
| Sex | |||
| Women | 20 (95.23%) | 19 (76%) | 38 (80.85%) |
| Men | 1 (4.76%) | 6 (24%) | 9 (19.14%) |
| Comorbidities | |||
| None | 5 (23.8%) | 9 (36%) | 14 (29.78%) |
| Diabetes mellitus | 0 (0%) | 0 (0%) | 2 (4.25%) |
| High blood pressure | 2 (9.52%) | 0 (0%) | 4 (8.51%) |
| Hypothyroidism | 3 (14.28%) | 1 (3.6%) | 4 (8.51%) |
| Diabetes mellitus+high blood pressure | 6 (28.57%) | 11 (44%) | 13 (27.65%) |
| Others | 5 (23.8%) | 4 (16%) | 10 (21.27%) |
Patient Assessment of Constipation-Quality of Life (PAC-QOL)
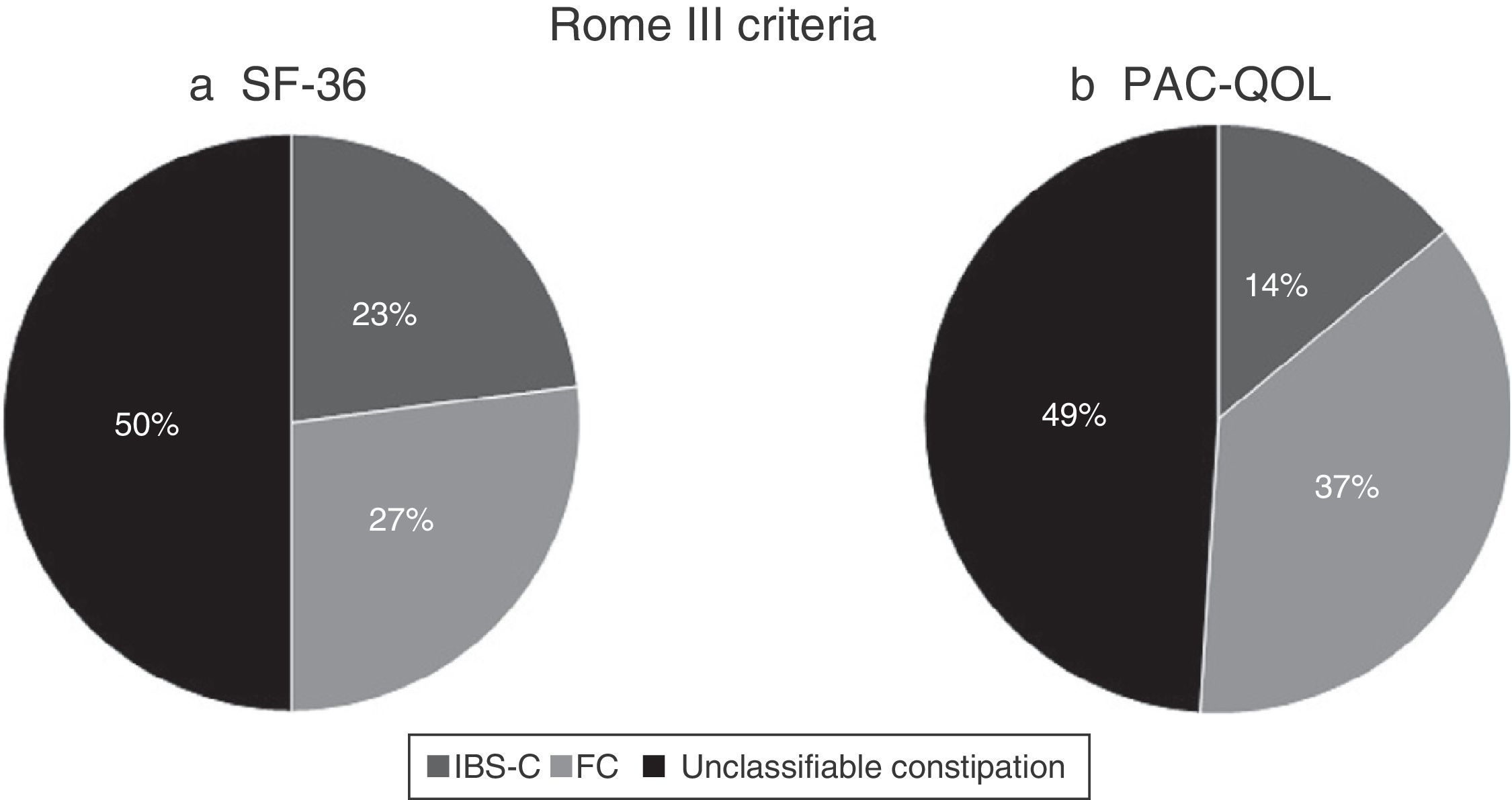
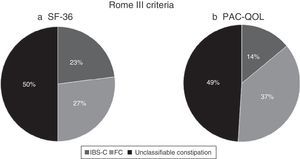
A total of 43 questionnaires were analyzed. The female sex was predominant (91%) in the study population and the mean age was 51 years (range: 20-87). The groups were distributed as follows, based on the Rome III criteria: IBS-C (14%), FC (37%), and unclassifiable constipation (49%) (fig. 2).
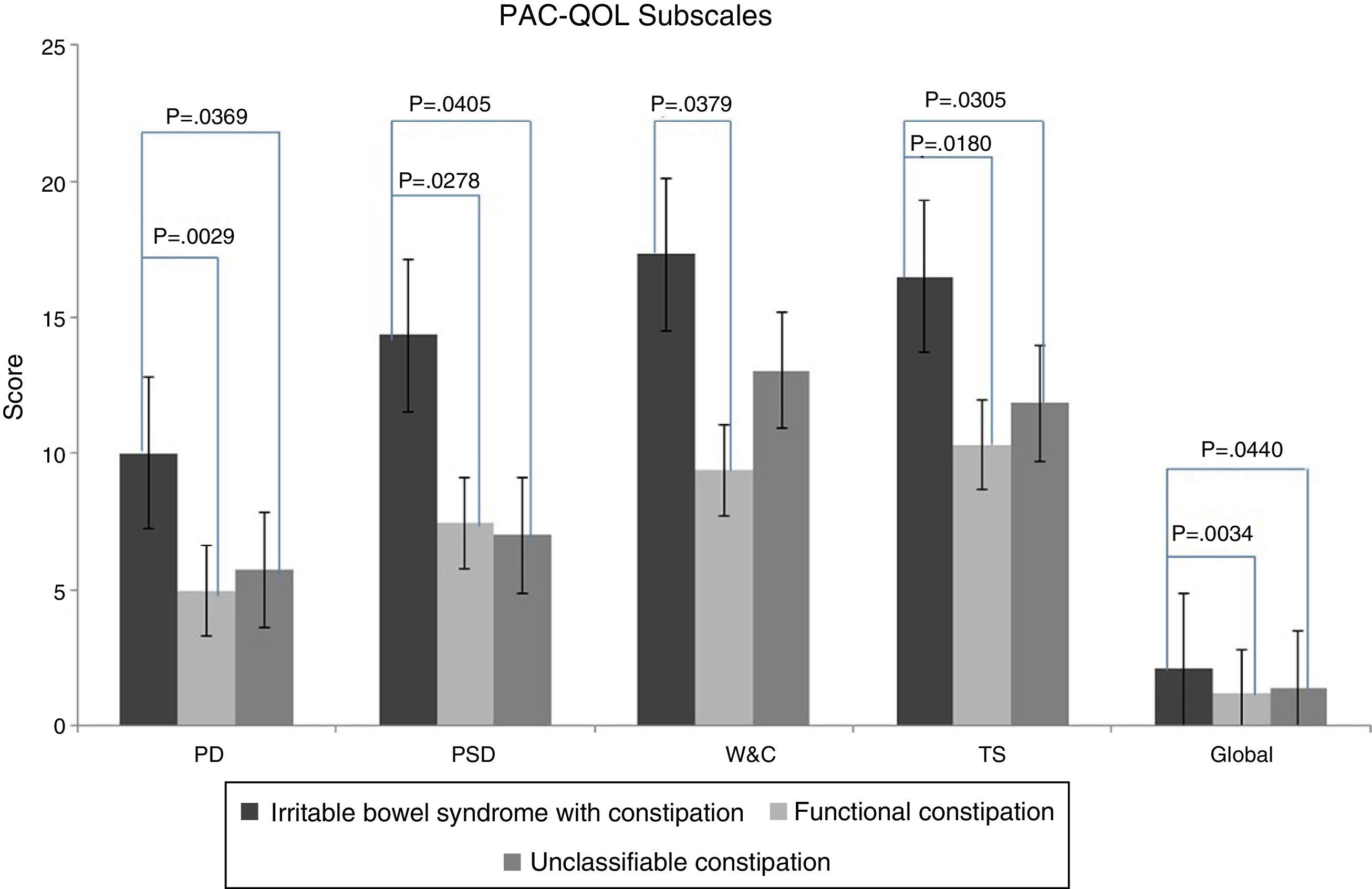
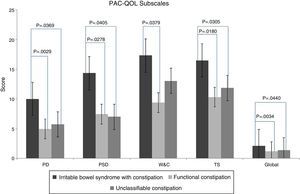
The analysis between groups showed significant differences (p=0.0299). Upon comparing individual groups, the IBS-C group had a higher score, compared with the FC group (p=0.0029; 10.00±1.125 vs 4.938±0.8086) and the unclassifiable constipation group (p=0.0369, 10.00±1.125 vs 5.727±0.9584) (fig. 3).
Psychosocial DiscomfortIn relation to psychosocial discomfort, the IBS-C group had a higher score compared with the FC group (p=0.0278; 14.33±2.704 vs 7.438±1.469) and the unclassifiable constipation group (p=0.0405, 14.33±2.704 vs 6.818±1.658) (fig. 3).
Worries and ConcernsLikewise, there were significant differences upon comparing the IBS-C group with the FC group (p=0.0379; 17.33±4.410 vs 9.375±1.494), but there was no significant difference between the unclassifiable constipation group and the IBS-C and FC groups (p > 0.05) (fig. 3).
Treatment SatisfactionThere was a difference in the degree of treatment satisfaction among the 3 groups (p=0.0443). The patients with IBS-C had a higher score compared with those with FC (p=0.0180; 16.50±0.4282 vs 10.31±1.440), as well as with the patients with unclassifiable constipation (p=0.0305; 16.50±0.4282 vs 11.77±1.059) (fig. 3).
Overall PAC-QOLThere was a difference between groups in relation to the total score. There was also a difference when comparing the IBS-C and FC patients (p=0.0034; 2.077±0.2704 vs 1.146±0.1391) and the IBS-C and unclassifiable constipation patients (p=0.0440; 2.077±0.2704 vs 1.323±0.1699) (fig. 3).
SF-36 questionnaireA total of 93 questionnaires were analyzed. The female sex predominated (82%) in the study population and the mean age was 48.70 years (range:18-87). In accordance with the Rome III criteria, the groups were distributed as follows: IBS-C (23%), FC (27%), and unclassifiable constipation (51%) (fig. 2).
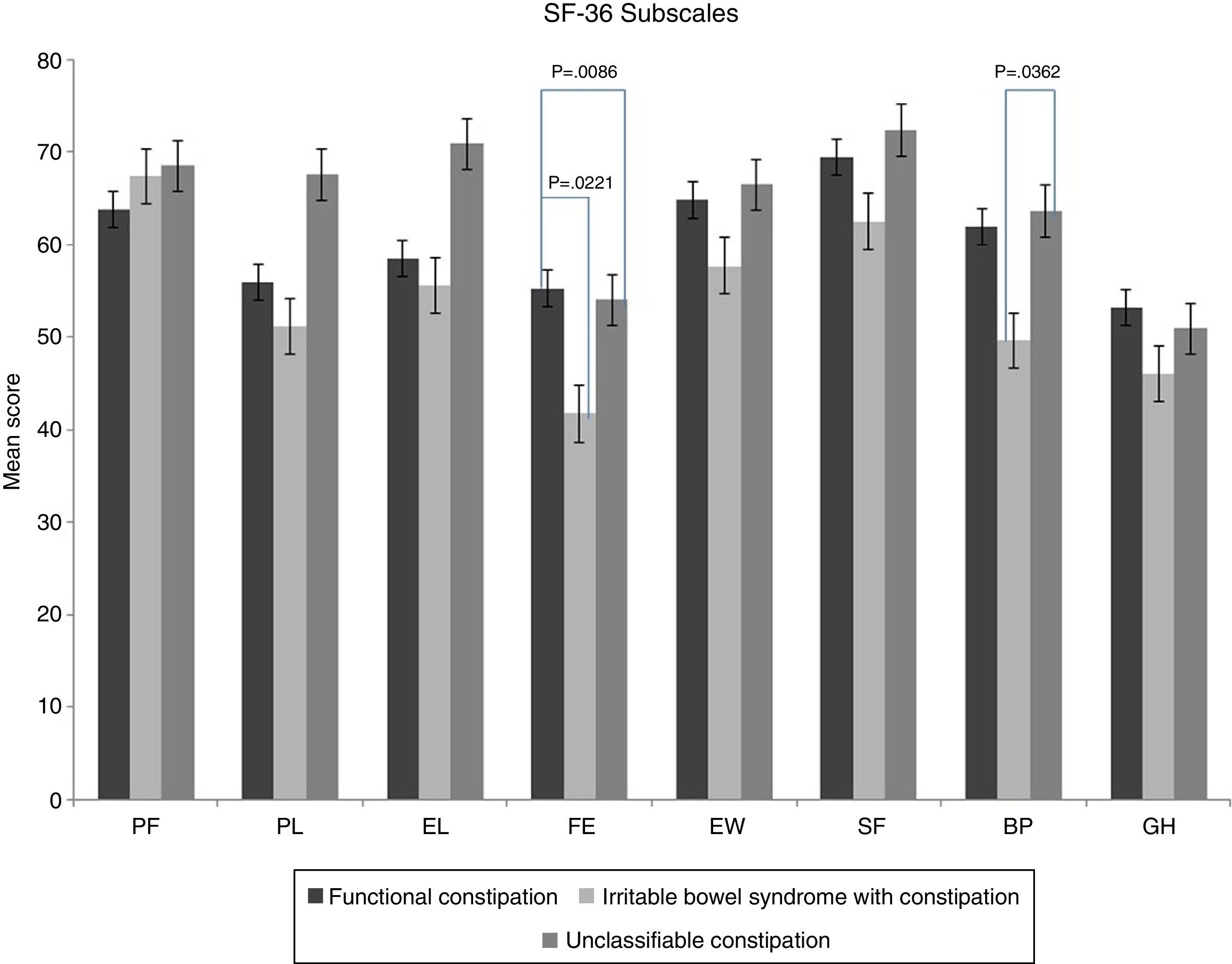
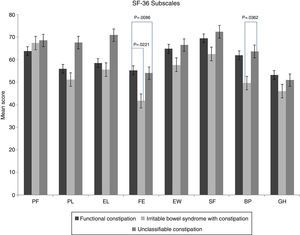
Physical Function, Physical Limitation, Emotional Well-Being, Social Function, and General HealthThere were no statistically significant differences (p>0.05) between the IBS-C, FC, and unclassifiable constipation groups during the analysis (fig. 4).
Body PainThere was no significant difference among the 3 groups, but there was a difference between the IBS-C group and unclassifiable constipation group (p=0.0362, 49.64±5.290 vs 63.62±3.673), indicating that patients with IBS-C experience more physical pain than those with unclassifiable constipation (fig. 4).
Fatigue/EnergyThere was a statistically significant difference between the 3 groups (p=0.0255). A significant difference was found upon comparing the IBS-C group and the FC group (41.67±3.386 vs 55.20±4.383, p=0.0221), signifying that the patients with IBS-C experience a lower energy level than those with FC. A difference was also found when IBS-C patients were compared with the unclassifiable constipation patients (41.67±3.386 vs 54.01±2.641, p=0.0086) (fig. 4).
DiscussionOur study showed that there are differences in the Rome III-based constipation subtypes in terms of quality of life, evaluated using both specific and general questionnaires. According to the SF-36 questionnaire, the patients with IBS-C were shown to be the most affected group, when compared with those of the FC and unclassifiable constipation groups, even though the differences were in only a few aspects. With respect to the PAC-QOL questionnaire, the IBS-C patients showed a poorer quality of life, followed by the patients in the unclassifiable constipation group and the FC group.
Ours is the first study conducted on a Mexican population that evaluates quality of life both generally and specifically in subgroups based on the Rome III criteria.
Previous studies have shown that patients with gastrointestinal disorders, mainly IBS and FC, present with a poorer quality of life,2 regardless of culture or nationality. This is especially true in regard to older adults7 and is related to symptom severity, being more evident in patients with moderate or severe symptoms.6
Much attention has been paid to quality of life by researchers and therapists because it allows the impact a disease has on different spheres of patient life to be known, with a consequent understanding of the patient's perceptions in relation to his or her environment. Therefore it is of interest to evaluate quality of life in order to determine treatment improvement and progress and to establish their level of impact on the physical, mental, and social realms of the individuals presenting with these diseases.5
Patients with chronic constipation have a poorer quality of life compared with healthy subjects. Moreover, there are reports indicating that patients with IBS experience diminished vitality.16 Using the SF-12, statistically significant differences were found between the physical and mental components of patients with chronic constipation, compared with healthy subjects. However, no differences were found with the application of the Quality of Life in Constipation-20 (CVE-20)1 questionnaire that specifically assesses quality of life in patients with constipation.
Patients with IBS experience physical, emotional, and social symptoms that have a negative impact on quality of life. IBS treatment is directed at relieving the symptoms and improving the functioning of the subjects that present with this disorder, making the use of scales for measuring quality of life relevant.17
It has been demonstrated that patients with FC experience a diminished quality of life, comparable to that of patients presenting with diseases such as asthma and rheumatoid arthritis.18 Using the SF-36 questionnaire, IBS patients have been shown to have lower scores than a sample of healthy subjects in a United States population.17 Similar results have been reported in European studies comparing IBS patients with healthy volunteers.19
Quality of life in patients with IBS and FC appears to improve in those patients that respond to any given treatment that is correlated with symptom improvement. There are factors that are apparently related to the quality of life experienced by the patients, and they include psychosocial elements, pain, and chronic stress.6 Decreased quality of life can result in school and work absenteeism and can also reduce productivity.2,8,9
Our study has several limitations. Given that the questionnaires are self-administered, it is possible that the patient may not adequately understand a question, depending on his or her educational level, sociocultural situation, or interest or motivation in filling out the questionnaire.12,20 In addition, our sample was small and perhaps was biased due to the fact that the questionnaires were applied at a tertiary care center. Likewise, the type of study (cross-sectional) does not permit the corroboration of constipation pathophysiology through auxiliary studies and the group of patients analyzed were seen at the outpatient clinic of a tertiary care hospital and thus might present with more intense symptomatology; both of these situations could influence the results. There could also have been bias in the selection of our patients, because the questionnaires were only administered to those patients thought to be “constipated” and that upon analyzing the answers in the Rome III questionnaire constipation module they were found to meet the criteria for being classified as having IBS and/or constipation. Nevertheless, the aim of the study was to analyze quality of life in a population presenting with constipation and therefore we exclusively directed the questionnaires to such a population.
Quality of life in the patients that complained of constipation was initially evaluated through the general SF-36 questionnaire, after which the specific PAC-QOL questionnaire was added to the analysis. The number of patients that answered the latter was lower and so we felt it was necessary to increase the number of measurements for that questionnaire. Likewise, since it was as specific questionnaire for the population with constipation we did not apply this type of questionnaire to a healthy population.
However, as study strengths, we believe that the patient could answer the PAC-QOL and SF-36 items with greater sincerity. The use of self-administered questionnaires enables information on sensitive subjects (situations that cause embarrassment) to be approached with greater accuracy and confidentiality20–important advantages in this study. The sample was an open one, not selected by speciality or by disease. The patients that were waiting for their medical consultation were not necessarily there because of their constipation, but rather for other factors, which is why we feel there was a lower level of ultra-selection of the sample.
In general the questionnaires were well received; the patients responded without pressure and the quality of their outpatient medical attention was in no way affected by whether or not they participated in the study.
The difference observed in how quality of life was affected utilizing the different questionnaires was interesting and is probably related to the fact that the PAC-QOL is a tool that is used specifically in patients with constipation, whereas the SF-36 evaluates general aspects of an individual's health.
When quality of life is affected, its impact on the development of patients in terms of productivity, absenteeism, and presenteeism is not known. Constipation treatment improves the quality of life of the subjects,6,21 but it is not known whether their work productivity or general welfare is also improved. And finally, it appears that there are other factors beyond abdominal pain that influence the worsening of quality of life in subjects with IBS that need to be identified in order to implement strategies targeted at improving them for the well-being of these patients.
ConclusionsThe SF-36 questionnaire demonstrated that the patients with IBS-C had a poorer quality of life, compared with the FC group and the unclassifiable constipation group. There were statistically significant differences in specific areas related to fatigue/energy and the presence of pain.
The PAC-QOL questionnaire, which is specifically for patients with constipation, showed differences in the patients with constipation subtypes; the patients with IBS-C were the most affected, compared with the other subtypes. Further studies are needed to determine the impact on performance in different productive areas (productivity, absenteeism, etc.) when quality of life is affected in patients that present with the different constipation subtypes.
Ethical responsibilitiesProtection of persons and animalsThe authors declare that no experiments were performed on humans or animals for this study.
Data confidentialityThe authors declare that they have followed the protocols of their work center in relation to the publication of patient data.
Right to privacy and informed consentThe authors have obtained the informed consent of the patients and/or subjects referred to in the article. This document is in the possession of the corresponding author.
Financial disclosureNo financial support was received in relation to this study/article.
Conflict of interestThe authors declare that there is no conflict of interest.
Please cite this article as: Ruiz-López MC, Coss-Adame E. Calidad de vida en pacientes con diferentes subtipos de estreñimiento de acuerdo a los criterios de ROMA III. Revista de Gastroenterología de México. 2015;80:13–20.