Acute appendicitis is one of the surgically resolved abdominal pathologies with the highest incidence, occurring in 7% of the general population.1 Fortunately it has a low mortality rate under 0.1%.2–4
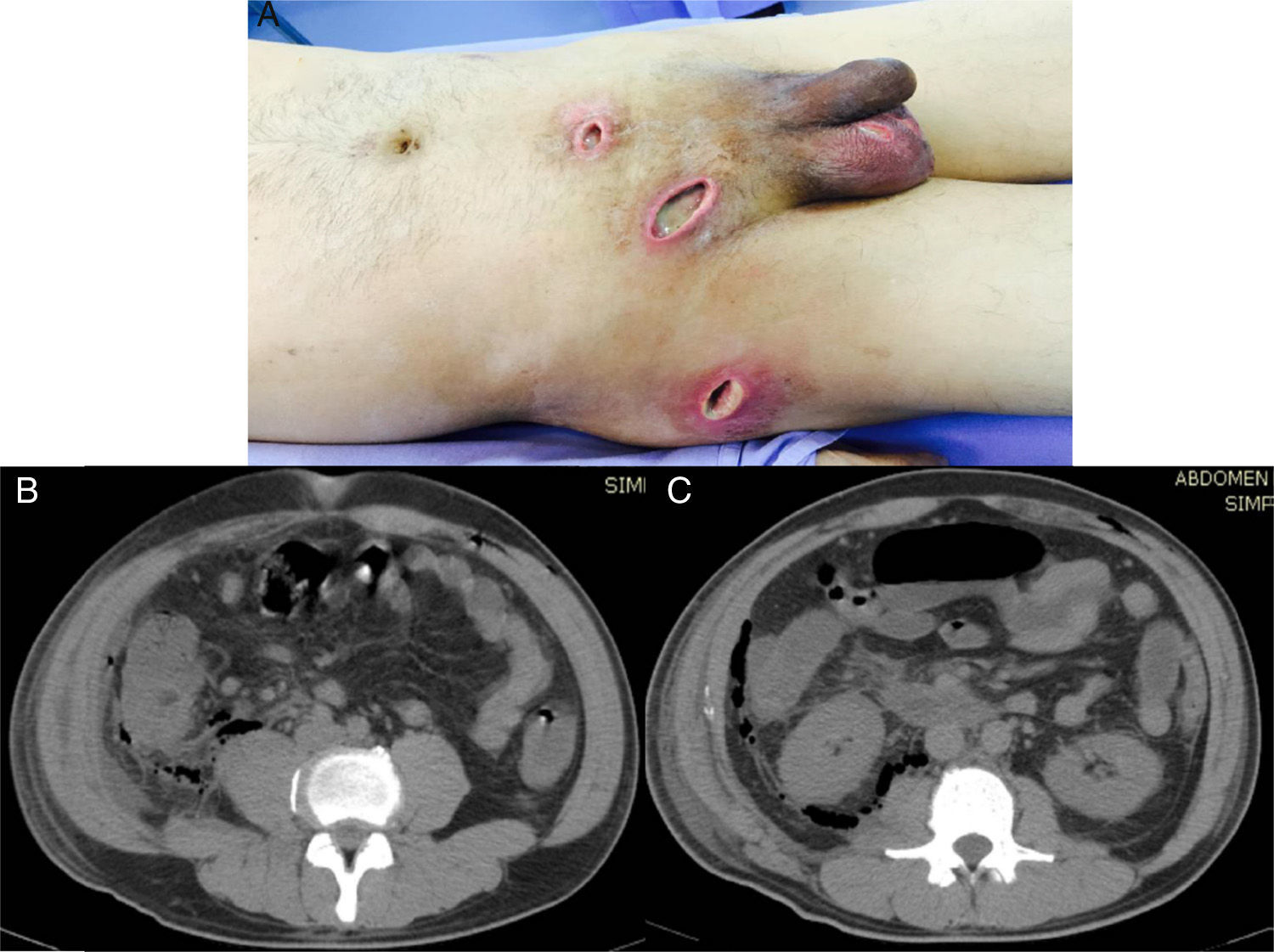
A 44-year-old man, who came to us from another hospital, had a relevant personal history of long progression type 2 diabetes mellitus that was apparently well controlled, and he had undergone a laparoscopic appendectomy on April 12, 2015 (38 days before we saw him). Phase III acute appendicitis was reported. It was defined as a venous infarction, total wall necrosis, and perforation, with the later formation of a localized abscess. Unfortunately, we had no detailed clinical report on the intraoperative findings or the surgical technique performed (use of antibiotic-impregnated sutures and/or preoperative asepsis and antisepsis measures). However, upon the patient's admission to our hospital, we observed a 3-port approach. One was a transumbilical port, another was at the level of the left flank, and the other was suprapubic. The first 2 had cicatrized, but abundant purulent matter was exuding from the suprapubic port wound. Likewise, we observed 3 other incisions, one at the level of the right inguinal region, another at the ipsilateral scrotal level, and another at the level of the right pelvic limb on the lateral surface of its proximal third, all of which contained abundant purulent matter and had an apparent internal connection (fig. 1A).
A) Important soft tissue infection is shown that extends from the suprapubic incision to the right inguinal region, and to the right scrotal region and flank, all with significant purulent matter. B) Tomographic image showing the retroperitoneal abscess extending proximally until reaching the costal ridge, with the presence of gas in its entire extension. C) Image showing the retroperitoneal abscess at the level of the cecum that extended through Toldt's fascia, with the presence of gas at this level.
The patient stated that on his 4th postoperative day, while he was still hospitalized, he presented with fever, pain at the surgical site, and a purulent discharge from the suprapubic port. His attending physician decided to remove the sutures from that port to favor its adequate drainage. However, despite antibiotic management (we do not know which regimens were established), progression was not satisfactory. To the contrary, there were signs of increased systemic inflammatory response, as well as soft tissue infection that extended to the inguinal region, the right scrotum, and the level of the right paracolic gutter. The 3 incisions mentioned above were made, all of which contained abundant purulent matter. Due to this poor progression, the patient was released 28 days later, still with wounds draining purulent matter, for which he came to the emergency department of our hospital on the 20th of May for medical attention.
Upon admission, the patient was conscious, with a facial expression of pain, and not very cooperative. His oral mucosa was dehydrated and he stated he had a weight loss of 8kg in the past 3 weeks. The patient had right pleural effusion and tachycardia, as well as a distended abdomen with muscular resistance that was depressible and painful upon mid and deep palpation. There was important pain at the level of the abdominal wall along the right paracolic gutter extending to the costal ridge and abundant purulent matter exuded from the abovementioned incisions. The patient had marked signs of peritoneal irritation, positive rebound tenderness, and reduced peristalsis. Laboratory tests upon admission reported conspicuous leukocytosis (22,000 cell/mm3) and an elevated procalcitonin level of 125 ng/ml.
Abdominal tomography scan identified a retroperitoneal collection at the level of the right fossa and paracolic gutter that extended into the soft tissues (figs. 1B and C). Exploratory laparotomy revealed an abscess of approximately 80 cc at the level of the retroperitoneum. A sample was taken from it for culturing and it developed Escherichia coli. The abscess was drained, and a closed drain was later placed at that level. The cavity was closed and lavage and soft tissue debridement was carried out, communicating the suprapubic wound and the proximal third of the leg. Access to the entire right paracolic gutter was thus achieved, revealing fasciitis and necrotic tissue. The latter was debrided and a Vacuum Assisted Closure (VAC) system was placed. Two surgical lavages with VAC replacement were later required. Patient progression was very satisfactory and leukocyte in blood (6.06 thousand/μl), procalcitonin (0.08 ng/ml), and C-reactive protein (0.71 ng/dl) values returned to normal. Given the patient's good progression, the surgical wound where the VAC was previously placed was closed and the abdominal drain was removed at 3 weeks, with a minimum serous output (fig. 2).
DiscussionAppendectomy, whether performed as a laparoscopic or open procedure, continues to be the cornerstone of management for this pathology, due to the important complications that can arise from late treatment. There are studies reporting conservative management that have shown it to be a safe practice, but it has not become generalized,5–8 because that could allow symptoms with an inherent increase in morbidity and mortality to progress in those patients.
On the other hand, there is a risk for complications, even with opportune diagnosis and treatment, including a minimally invasive approach, as was the case with our patient. We would like to take a moment to analyze what the main causes of those complications could have been:
Undoubtedly a factor was the patient's history of type 2 diabetes mellitus, even though the patient was supposedly well controlled. Previous glycemic controls and glycosylated hemoglobin were not available and the patient had values above 400mg/dl upon hospital admission. This imbalance could have been secondary to the infectious process.
The laparoscopic approach as described by Aranda-Narváez et al.9 was employed. Open appendectomy entails a greater risk for infection of the parietal surgical site and the laparoscopic approach for organ/space infection. However, our patient developed both, a retroperitoneal abscess and soft tissue infection. With respect to the soft tissue infection, the process of specimen extraction would need to be evaluated and we had no record of it, but we did know that abundant purulent matter had been reported.
The previous management of the patient was surprising in regard to the soft tissue infection. It appears that even though 3 incisions at different sites were made, an attempt was made to be as noninvasive as possible. This simply resulted in poor infection control and its propagation, possibly due to the fact that the incisions were very small and superficial, making the debridement of all the necrotic tissue through them unfeasible. In addition the incisions were made in the patient's room with local anesthesia and undoubtedly the discomfort that this caused the patient also hindered adequate drainage and debridement.
A meta-analysis by Sauerland et al. concluded that the laparoscopic approach could be generalized to include all patients, with surgical site infection being one of the most important aspects to consider.10 Despite the fact that there is a lower risk for soft tissue infection with the laparoscopic approach, one must not lose sight of the factors that can reduce this type of complication. They include removing the specimen inside an extraction bag (Endo Catch), a careful lavage of the abdominal cavity, and the placement of a closed drain, given that a localized abscess was encountered during appendectomy.
FundingNo financial support was received in relation to this study/article.
Conflict of interestThe authors declare that there is no conflict of interest.
Please cite this article as: Bahena-Aponte JA, González-Contreras Q, Tepeyac A. Complicaciones graves de apendicitis aguda con abordaje laparoscópico. Revista de Gastroenterología de México. 2017;82:186–189.