It is possible to resect the perforated segment and reestablish intestinal continuity with adequate morbidity and mortality results in patients with complicated diverticulitis.
AimsTo evaluate the type of surgery performed at our center and the results of the procedures in patients with complicated diverticulitis.
Material and methodsAll patients that underwent sigmoidectomy due to complicated diverticulitis within the time frame of 2005-2012 were included in the study. The primary objective was to evaluate the type of surgery performed. The secondary objective was to evaluate patient morbidity and mortality after 30 postoperative days.
ResultsThe study included 77 patients with a mean age of 51.17±12.80 years. The majority of the patients were men (64.9%) (n=50) and the mean BMI was 28.24±4.06kg/m2. A total of 63.6% (n=49) patients presented with a Hinchey iii-iv classification. Sigmoidectomy with primary anastomosis was performed in 58.4% (n=45) of the patients, 48.8% (22/45) of whom presented with Hinchey iii-iv. Primary anastomosis was more frequently performed in patients that had Hinchey i-ii(P=.001). Open surgery was carried out in 85.7% (n=66) of the cases. The mean surgery duration was longer in the patients with primary anastomosis (181.73±68.2min vs. 152.13±65.8min) (P>.05). Colorectal surgeons performed the procedures in 44.2% (n=34) of the cases. Complications presented in 23.4% (n=18) of the patients and there was a tendency toward more complications in patients that underwent the Hartmann's procedure. The mortality rate was 2.6% (n=2).
ConclusionsSigmoidectomy with primary anastomosis is a frequent surgery in patients with complicated diverticulitis at our hospital. There was no difference in morbidity and mortality, compared with the Hartmann's procedure.
Es posible resecar el segmento perforado y reestablecer la continuidad intestinal en pacientes con diverticulitis complicada con adecuada morbimortalidad.
ObjetivoEvaluar el tipo de cirugía realizada y los resultados operatorios en pacientes con diverticulitis complicada en nuestro centro.
Material y métodosSe incluyó a todos los pacientes sometidos a sigmoidectomía por diverticulitis complicada durante el período 2005 al 2012. El objetivo primario fue evaluar el tipo de cirugía realizada. El objetivo secundario fue evaluar la morbimortalidad operatoria a 30 días.
ResultadosSe incluyó a 77 pacientes. La edad promedio fue de 51.17±12.80 años, la mayoría de los pacientes fueron hombres 64.9% (n=50), el IMC promedio fue de 28.24±4.06kg/m2, 63.6% (n=49) presentaron un Hinchey iii-iv. En el 58.4% (n=45) se realizó una sigmoidectomía con anastomosis primaria, específicamente en pacientes con Hinchey iii-iv, esta cirugía se realizó en el 48.8% (22/45). En pacientes con Hinchey i-ii fue más frecuente realizar una anastomosis primaria (p=0.001). La cirugía fue abierta en 85.7% (n=66) de los casos. El tiempo operatorio promedio fue más largo en pacientes con AP 181.73±68.2min vs. 152.13±65.8min (p>0.05). La cirugía fue realizada por cirujanos colorrectales en 44.2% (n=34) de los casos. Se presentaron complicaciones en el 23.4% (n=18) de los casos, hubo una tendencia a presentar más complicaciones los pacientes con operación de Hartmann. La mortalidad fue del 2.6% (n=2).
ConclusionesLa sigmoidectomía con anastomosis primaria es una operación frecuente en pacientes con diverticulitis complicada en nuestro hospital. No hay diferencia en la morbimortalidad comparado con el procedimiento de Hartmann.
The estimated prevalence of diverticulosis is 5% in persons from 30-39 years of age, and rises to 60% in those above 80 years of age.1 The risk for diverticulosis progressing to diverticulitis has recently been estimated at only 4%,2 with an estimated incidence of perforated diverticulitis in adults of 3.5 per 100,000.3 Diverticulitis is a disease with a spectrum that extends from mild inflammation with no complications to complicated disease that can go from a pericolic abscess to free perforation with fecal peritonitis. Acute diverticulitis severity is evaluated through the Hinchey classification.4 Basically, uncomplicated diverticulitis is treated conservatively, whereas Hinchey stage III and IV complicated diverticulitis requires surgical management. The recommended treatment consists of resection of the affected bowel segment and closure of the rectal stump (Hartmann's procedure [HP])5. A significant number of patients that survive this procedure never undergo restoration of intestinal continuity 6–8 and suffer considerable deterioration in their quality of life as a result of treatment of a benign disease.9 It has been suggested that it is possible to resect the perforated bowel segment and reestablish intestinal continuity (primary anastomosis [PA]) under certain circumstances, with adequate results in terms of patient morbidity and mortality.10
Given the constant evolution in the surgical treatment of this disease, the aim of the present article was to evaluate the type of surgery performed and the resulting morbidity and mortality in patients operated on for complicated diverticulitis at our center.
AimTo evaluate the type of surgery performed and the resulting morbidity and mortality in patients operated on for complicated diverticulitis at our center.
Patients and methodsAll patients that underwent sigmoidectomy within a 7-year period (2005-2012) at a single institution (Hospital Médica Sur, Mexico City) were identified through the hospital's administrative database. Those patients requiring surgery due to complicated diverticulitis were then identified. Complicated diverticulitis was defined as an episode of acute diverticulitis associated with free perforation with peritonitis and generalized sepsis or with phlegmon and/or abscess that did not respond to conservative treatment. It is important to mention that the patients with peritonitis and generalized sepsis were surgically treated immediately after diagnosis; the patients with phlegmon and/or abscess were treated conservatively (antibiotics), and if they did not respond, they were then treated surgically. Diverticulitis diagnosis was confirmed through medical history and computerized tomography findings. The Hinchey classification was determined based on the surgical operation note. In accordance with hospital policy, all patients signed statements of informed consent before the procedure.
A retrospective review was carried out by reviewers that did not participate in the treatment process. The information was registered on a data collection sheet. The primary objective was to analyze the type of surgery performed and the secondary objective was to evaluate the postoperative patient morbidity and mortality 30 days after the procedure. The latter included intra-abdominal bleeding, intra-abdominal abscess, surgical site infection, prolonged ileus, anastomosis dehiscence, respiratory failure, heart failure, kidney failure, and multiple organ failure. Hospital stay was calculated from the day of the surgery to release from the hospital. Two types of surgery were performed: 1) HP, which consisted of resection of the affected bowel segment and closure of the rectal stump, and 2) PA, which consisted of resection of the perforated segment and PA. Anastomosis dehiscence was defined through imaging studies as contrast medium extravasation or pelvic abscess around the anastomosis.
The variables analyzed were: demographic data, medical comorbidities, body mass index (BMI, kg/m2), Hinchey classification, the Amercian Society of Anesthesiology classification, and white blood cell count. The results included intraoperative data such as: the type of operation, the type of surgeon: general vs. colorectal, the surgical approach: open vs. laparoscopic, surgery duration in min, blood loss in ml, transfusion, and intraoperative complications. The postoperative data included: admission into the intensive care unit after surgery, hospital stay, transfusion, readmission rate, need for re-operation, and morbidity and mortality at 30 days.
Statistical analysisThe continuous data were expressed as means with standard deviation (SD) or medians with ranges, and the categorical data were presented as proportions. The chi-square test and the Fisher exact test were used to compare the differences between groups and the Student's t test or Mann-Whitney U test were used in corresponding cases. The data were considered statistically significant with a p ≤ 0.05. The SPSS/Mac v17 program was used for the statistical analysis.
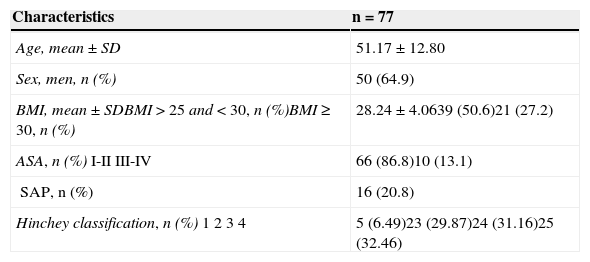
ResultsOf the 120 patients that underwent sigmoidectomy, 30 presented with a disease other than complicated diverticulitis and were therefore excluded from the study. In addition, 13 patients underwent elective surgery for previous episodes of diverticulitis, but not for complicated diverticulitis, and so they were also excluded. A total of 77 patients were included in the study. The mean age was 51.17 ± 12.80 years, the majority of the patients were men (64.9%) (n = 50), and the mean BMI was 28.24 ± 4.06kg/m2. A total of 63.6% (n = 49) patients were classified with Hinchey III-IV. Of the total number of patients with obesity (n= 21), 13 (62%) had a Hinchey III-IV, with a p = 0.52 that did not reach statistical significance. In patients with overweight (n = 39), 25 (64%) had a Hinchey III-IV, with a p = 0.56. Table 1 shows the demographic and clinical characteristics of the 77 patients in the study. The surgical characteristics are presented in Table 2.
Demographic characteristics of the study patients.
| Characteristics | n = 77 |
|---|---|
| Age, mean ± SD | 51.17 ± 12.80 |
| Sex, men, n (%) | 50 (64.9) |
| BMI, mean ± SDBMI > 25 and < 30, n (%)BMI ≥ 30, n (%) | 28.24 ± 4.0639 (50.6)21 (27.2) |
| ASA, n (%)I-IIIII-IV | 66 (86.8)10 (13.1) |
| SAP, n (%) | 16 (20.8) |
| Hinchey classification, n (%)1234 | 5 (6.49)23 (29.87)24 (31.16)25 (32.46) |
BMI= Body mass index; SAP= Systemic arterial pressure; SD= Standard deviation.
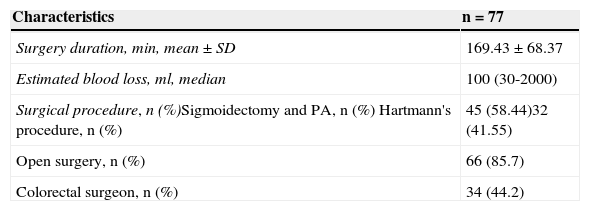
Surgical characteristics of the study patients.
| Characteristics | n = 77 |
|---|---|
| Surgery duration, min, mean ± SD | 169.43 ± 68.37 |
| Estimated blood loss, ml, median | 100 (30-2000) |
| Surgical procedure, n (%)Sigmoidectomy and PA, n (%) Hartmann's procedure, n (%) | 45 (58.44)32 (41.55) |
| Open surgery, n (%) | 66 (85.7) |
| Colorectal surgeon, n (%) | 34 (44.2) |
PA= primary anastomosis.
Sigmoidectomy with PA was performed in 58.4% (n = 45) of the patients and of those, 48.8% (22/45) had Hinchey III-IV. PA was performed more frequently in patients with Hinchey I-II (p = 0.001). Open surgery was carried out in 85.7% (n = 66) of the cases. Mean surgery duration was longer in the patients that underwent PA 181.73 ± 68.2min vs. 152.13 ± 65.8min (p > 0.05). The surgeries were performed by colorectal surgeons in 44.2% (n = 34) of the patients.
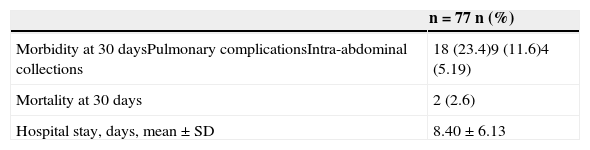
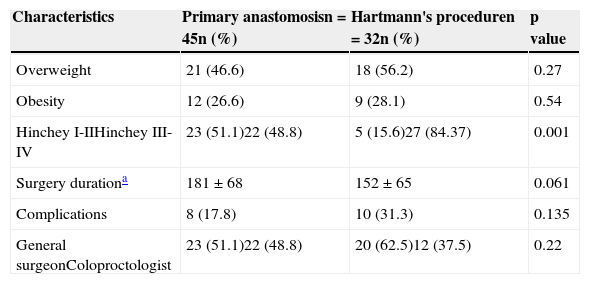
Table 3 shows the postoperative progression. There were complications in 23.4% (n = 18) of the cases. The most frequent were pulmonary problems (11.8%) (n = 9) and intra-abdominal collections (5.2%) (n = 4). There was a trend toward more complications in the patients that underwent the HP (p = 0.135). Of the total of patients with overweight (n = 39), 8 (21%) presented with complications, with a p = 0.01. Mortality was 2.6% (n = 2), due to pulmonary insufficiency and myocardial infarction. Table 4 compares the characteristics of both groups. It should be mentioned that both the majority (84%) of the patients that underwent HP and 49% of the patients that underwent PA had a Hinchey III-IV, but there was no significant difference in the complication comparison of the two groups (p = 0.135).
Patient characteristics according to surgical treatment group.
| Characteristics | Primary anastomosisn = 45n (%) | Hartmann's proceduren = 32n (%) | p value |
|---|---|---|---|
| Overweight | 21 (46.6) | 18 (56.2) | 0.27 |
| Obesity | 12 (26.6) | 9 (28.1) | 0.54 |
| Hinchey I-IIHinchey III-IV | 23 (51.1)22 (48.8) | 5 (15.6)27 (84.37) | 0.001 |
| Surgery durationa | 181 ± 68 | 152 ± 65 | 0.061 |
| Complications | 8 (17.8) | 10 (31.3) | 0.135 |
| General surgeonColoproctologist | 23 (51.1)22 (48.8) | 20 (62.5)12 (37.5) | 0.22 |
In the present study, sigmoidectomy with PA was performed in more than half (58%) of the patients, with no difference in surgical morbidity and mortality when compared with the HP group. In general, up to 25% of the patients hospitalized for diverticulitis require emergency surgical intervention, indicated for patients with diffuse peritonitis or for those in whom conservative management has failed.11 Even though the HP has become standard treatment in patients with complicated diverticulitis, there is enough evidence supporting the fact that patients with peritonitis are candidates for the performance of PA and the re-establishment of intestinal continuity in the same surgery. Reports have been published stating that PA is associated with a significant improvement in surgical morbidity and mortality, compared with the HP.10–13
A randomized, controlled clinical study was conducted on patients with Hinchey III and IV that underwent sigmoidectomy with terminal colostomy (HP) and later reconnection. They were compared with patients that underwent sigmoidectomy with PA and protection ileostomy with later ileostomy closure.14 The results showed more severe complications in the group of patients with the Hartmann's procedure reversal than in the group with ileostomy closure (20% vs. 0%). The same study also demonstrated that the patients in the HP group had significantly fewer probabilities of undergoing reconnection than the patients with ileostomy (57% vs. 90%).
In our study, there were no statistically significant differences in morbidity and mortality between the patients with HP and those with PA. Nevertheless, there was a trend toward more complications in the patients with the HP (31%), with a p = 0.135.
Delayed morbidity and disability associated with the HP reversal, compared with ileostomy closure, should also be taken into account. It is known that up to half of the patients that undergo HP end up with permanent colostomy. Approximately 90% of the patients that undergo PA with loop ileostomy are able to undergo ileostomy closure.15 We have not been able to compare these procedures in our patients due to a lack of information, but it is an interesting point in deciding whether to perform PA or HP. Although the primary goal is to perform a safe and efficacious surgery for the patients with complicated diverticulitis, the morbidity and mortality of HP reversal should be considered.
Curiously, the majority of patients in the present study with complicated diverticular disease were overweight or obese, at 50.6% and 27.7%, respectively. Although it was not the aim of our study, we observed a relation between overweight/obesity and complicated diverticular disease. A retrospective analysis found that patients with uncomplicated diverticulitis had a significantly lower BMI that the patients that presented with perforation (p = 0.001) or recurrent disease (p = 0.002).16 The authors of a prospective cohort study published in 2009 specifically observed the cases of diverticulitis and diverticular bleeding and analyzed the weight, waist circumference, and waist-to-hip ratio of the patients.17 Men with a BMI ≥ 30 had a relative risk of 1.78 for presenting with diverticulitis and of 3.19 for presenting with diverticular bleeding, compared with men with a BMI ≤ 20 (95% confidence interval (CI), 1.08 to 2.94; 1.45 to 7.00). Waist circumference and the waist-to-hip ratio were also associated with a higher risk for presenting with diverticulitis and diverticular bleeding. In our study we found that the patients with obesity presented with more complications than the patients with overweight (p = 0.01), and in general the patients with overweight and/or obesity had more complications than the rest of the group.
We recognize that our study had the following limitations: its retrospective design with the small number of patients. The limited number of patients could have introduced error in the comparison of the statistical groups. In addition, the patients were operated on by surgeons with varying experience in colorectal and laparoscopic surgery. However, the aim of the study was to determine the type of surgery performed in patients with complicated diverticulitis and the surgical morbidity and mortality at our center. Furthermore, ours is the first study on this topic conducted at a Latin American center.
ConclusionsPA is a common surgery for patients with complicated diverticular disease with no statistical difference in morbidity and mortality when compared with HP. PA can be the optimum strategy for selected patients with complicated diverticular disease.
Ethical responsibilitiesProtection of persons and animalsThe authors declare that no experiments were performed on humans or animals for this study.
Data confidentialityThe authors declare that they have followed the protocols of their work center in relation to the publication of patient data.
Right to privacy and informed consentThe authors have obtained the informed consent of the patients and/or subjects referred to in the article. This document is in the possession of the corresponding author.
Financial disclosureNo financial support was received in relation to this article.
Conflict of interestThe authors declare that there is no conflict of interest.
Please cite this article as: Reyes-Espejel L, Ruiz-Campos M, Correa-Rovelo JM, García-Osogobio S. Sigmoidectomía con anastomosis primaria para diverticulitis complicada. Revista de Gastroenterología de México. 2015;80:255–259.