Lynch syndrome is the most common hereditary colorectal syndrome. It is an autosomal dominant disease caused by germline mutations in these DNA mismatch repair (MMR) genes:1,2 MLH1 (50%), MSH2 (40%), MSH6 (7-10%), and PMS2 (5%). The inactivation of both alleles in one of the MMR genes generates microsatellite instability, which is characteristic of Lynch syndrome.1 Mutations in MLH1 are associated with a higher prevalence of colorectal cancer and mutations in MSH2 with extracolonic presentation.2
Colorectal cancer is the most frequent neoplasia in this syndrome, followed by endometrial cancer.3 Patient age for colorectal cancer depends on the mutated MMR gene; MLH1 and MLH2 are related to earlier age presentation (27-46 years), and PMS2 to later age presentation (61 years).4 Other tumors forming part of the Lynch syndrome spectrum are: gastric cancer, ovarian, small bowel, urinary tract, hepatobiliary, and brain tumors.5 The most widely used screening methods are: immunohistochemistry and PCR detection of microsatellite instability. Gene sequencing is required for the definitive diagnosis.6
A 52-year-old woman had a past history of cancer in maternal second-degree relatives: an aunt with breast cancer, an uncle with bladder cancer, an aunt with lung cancer, and an uncle with esophageal cancer, none of whom were diagnosed before the age of 40 years.
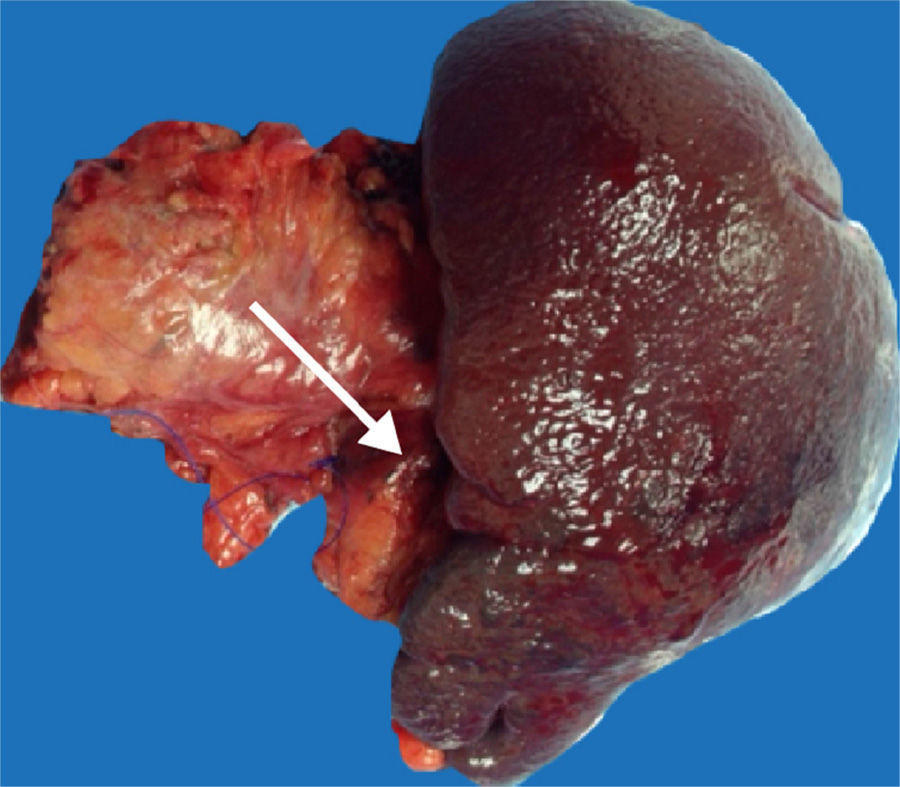
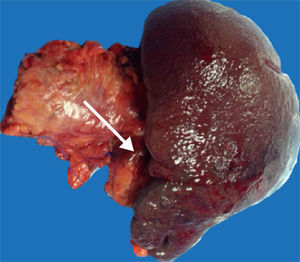
Our patient had disease onset with transvaginal bleeding. A pelvic ultrasound study and endometrial biopsy were ordered, and the biopsy reported endometrioid adenocarcinoma. Extended studies showed a BIRADS-V lesion in the right breast and a CAT scan identified a nodule in the tail of the pancreas (fig. 1) that was biopsied through endoscopic ultrasound, reporting carcinoma. CA-125 determination was carried out and resulted in 18 U/ml. Radical hysterectomy with pelvic lymph node dissection was performed and the histopathologic study reported well-differentiated stage 1 endometrioid adenocarcinoma that was positive for cytokeratin 5/6, protein 16, and for estrogen and progesterone receptors. Quadrantectomy and axillary dissection reported luminal B, grade II invasive ductal carcinoma that was HER2-negative and 13 out of 28 lymph nodes had metastasis. Three weeks later, the patient underwent distal pancreatectomy with splenectomy that revealed ductal carcinoma of 1.3cm (fig. 2), with negative lymph nodes. Immunohistochemistry of the latter was suggestive of mutation in the MMR genes: MLH1 (-), PMS2 (-), MSH2 (+), and MSH6 (+). Panendoscopy and colonoscopy were normal. The patient is currently in treatment with adjuvant chemotherapy.
The present case involves 3 primary tumors with immunohistochemistry suggestive of Lynch syndrome. However, the absence of colon cancer and the presence of breast cancer are inconsistent with this syndrome. Forty to 60% of women with Lynch syndrome may present with endometrial cancer, and the most frequent histologic type is endometrioid.7 The absence of MLH1 in the immunohistochemistry suggests a mutation in that gene that is affected in 24-40% of the cases of endometrial cancer.7 MLH1 mutation is associated with disease appearance at early ages and a predominance of colorectal cancer, therefore findings during colonoscopy suggestive of cancer in this patient would have been expected.2,4
Cancer of the pancreas is less frequent, compared with other associated tumors, and its presentation age fluctuates between 63 and 65 years.4 The association of breast cancer and cancer of the pancreas with BRCA 2 mutation carriers has been reported,8 but our patient did not have a history of early age breast cancer or ovarian cancer in her family and that mutation has not been associated with endometrial cancer. The inclusion of breast cancer within the Lynch syndrome tumor spectrum is still a subject of debate and is presently being studied.9 There is evidence that mutations in the MLH1 gene increase the risk for presenting with breast cancer and the presence of microsatellite instability is related to early age presentation of that disease.4,10
The present case suggests an atypical presentation of Lynch syndrome. Because of the immunohistochemistry findings, sequencing of the MLH1 gene is required for making the definitive diagnosis. However, access to this diagnostic test is limited in Mexico and it is expensive. Therefore, the patient will continue with yearly follow-up due to her high risk for developing colorectal cancer.
Financial disclosureNo financial support was received in relation to this study/article.
Conflict of interestThe authors declare that there is no conflict of interest.
Please cite this article as: Medina-Franco H, Pimienta-Ibarra AS, Pastor-Sifuentes FU, Ramírez-Luna MÁ. Cánceres primarios simultáneos; ¿síndrome de Lynch atípico? Revista de Gastroenterología de México. 2015;80:169–170.