¿ Introduction
Ampullary tumors are rare with an estimated incidence of 27 cases per 100 000. The most common histological types are adenoma and adenocarcinoma, but other tumors such as lipoma, leiomyoma, carcinoid, hemangioma, fibroma and neurogenic tumors have been reported.1 In contrast to pancreatic malignancies, development of symptoms from biliary and pancreatic duct obstruction often occurs when the ampullary tumors are still very small. This accounts for earlier diagnosis, more favorable prognosis and the possibility of treatment by minimally invasive techniques in ampullary tumors. Tumors extending beyond the lamina propria or with lymph node involvement demand surgical resection (Whipple's procedure), while pre-malignant and early ampullary cancers can be successfully managed with endoscopic ampullectomy.2,3 However, complications can occur following endoscopic resection, with the incidence of pancreatitis, bleeding and perforation of 11%, 7% and 5%, respectively. We report a successful case of endoscopic ampullectomy in a patient with a villous adenoma in the major ampulla, and a peri-ampullary diverticulum.
¿ Case report
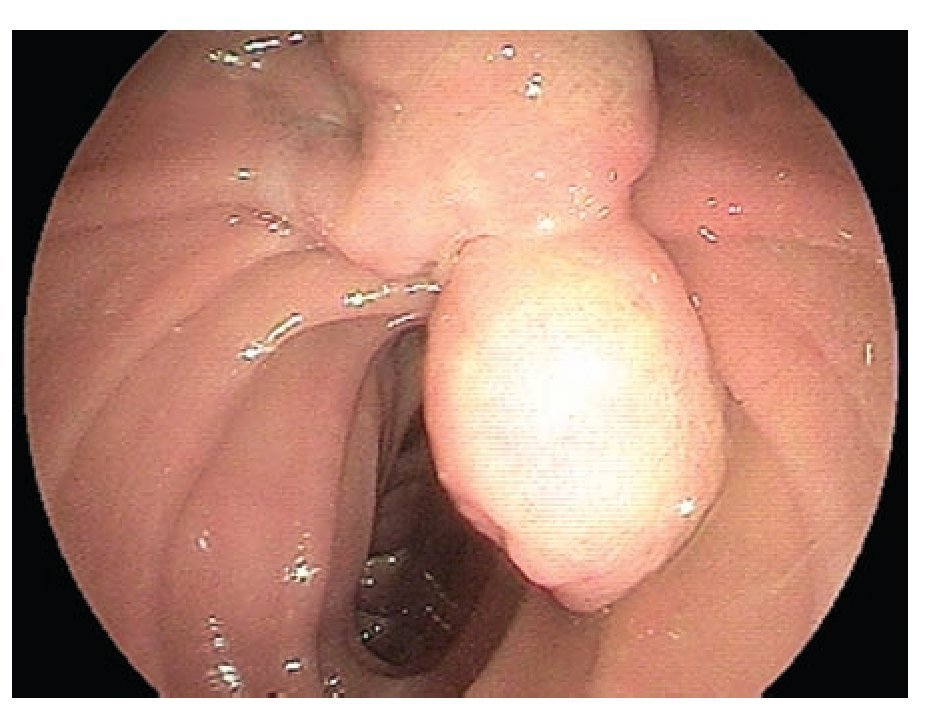
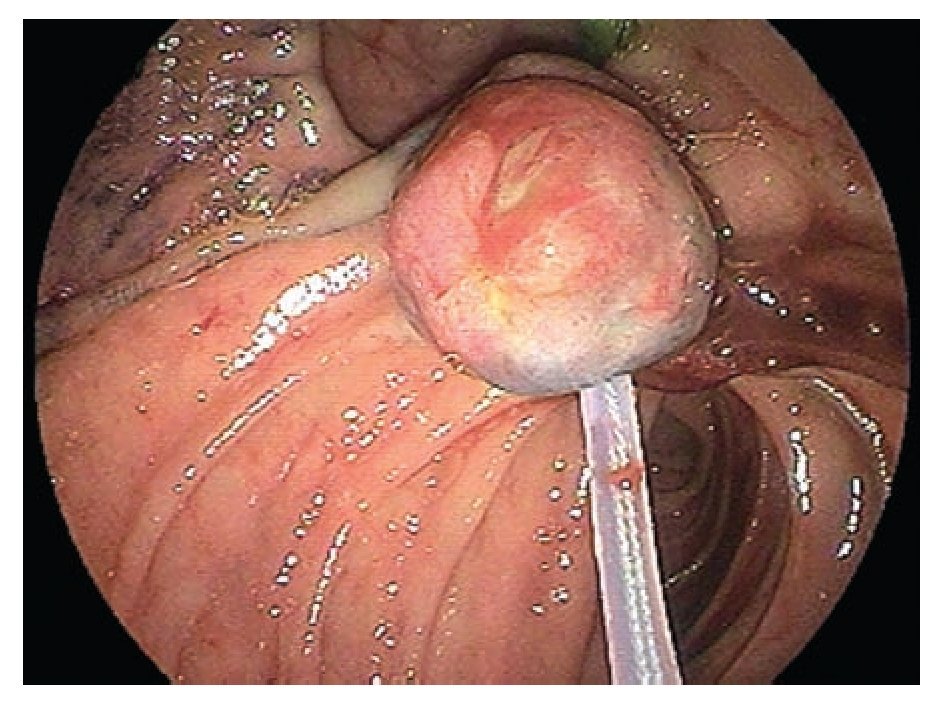
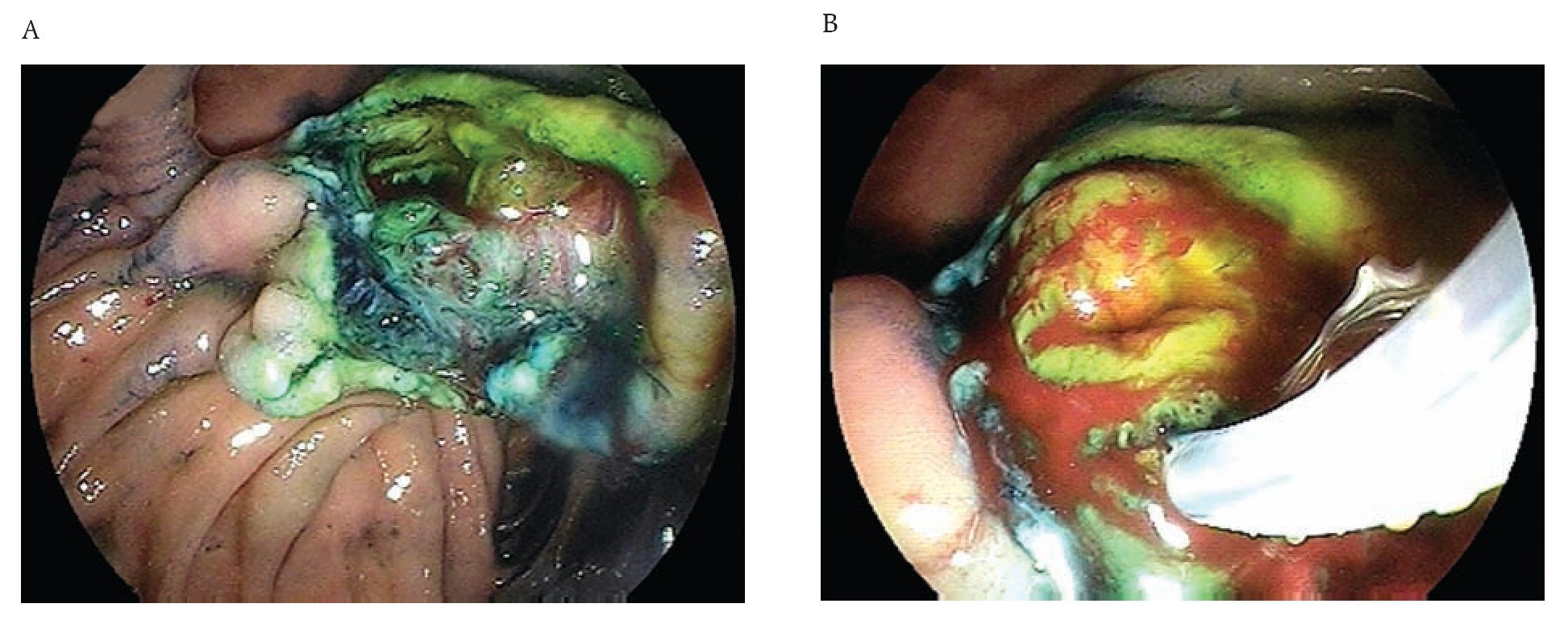
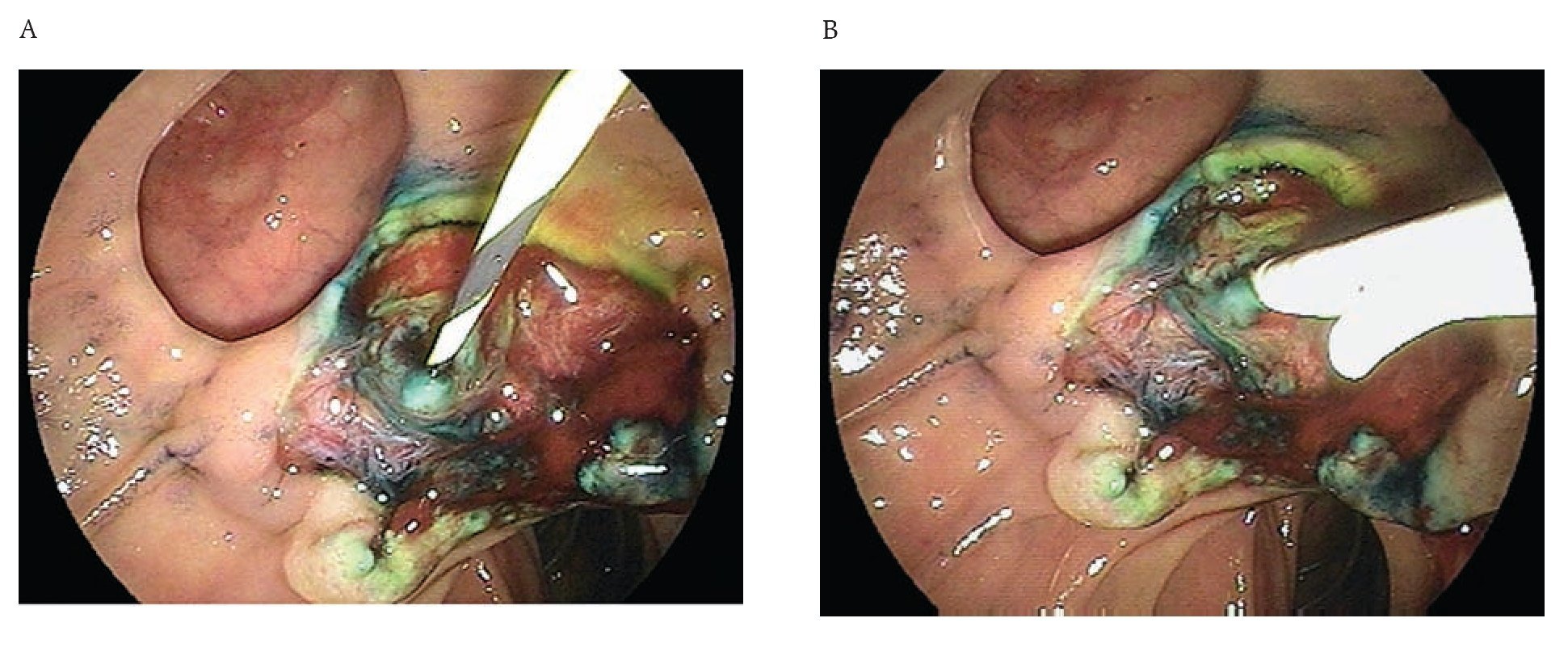
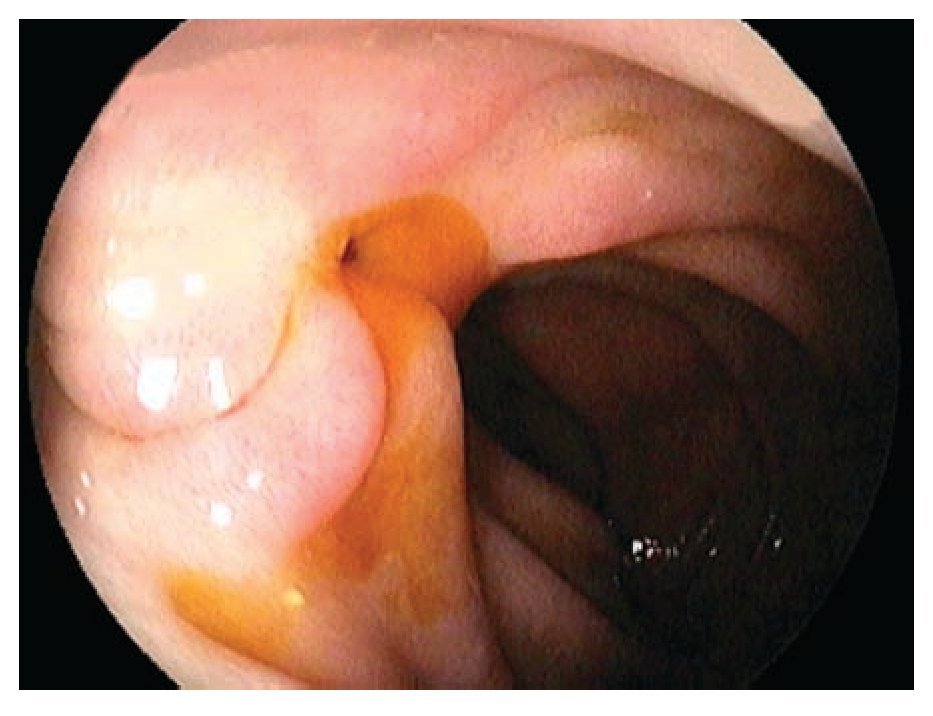
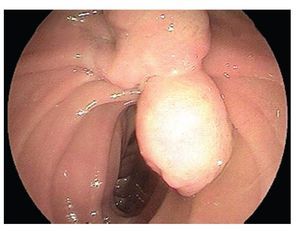
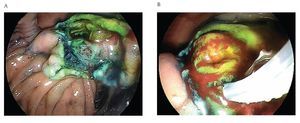
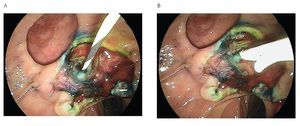
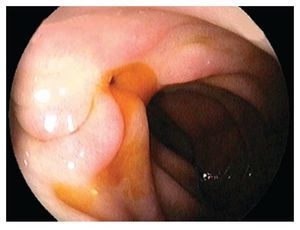
A 65 year old man was admitted with a two-month history of right upper quadrant abdominal pain and a six week history of dyspepsia and itching. Physical examination was positive for icteric sclera, and a pruritic rash. Direct bilirubin was 17 mg/dL (0.2-0.6 mg/dL) and alkaline phosphatase was 977 IU/L(10-40 IU/L). Abdominal ultrasound showed dilation of the intra and extrahepatic biliary systems. Upper endoscopy with a duodenoscope (Fujinon FD7XL) showed an enlarged major ampulla, which measured approximately 2.5 cm and localized in a peridiverticular papilla. Biopsies from the ampulla reported a villous adenoma (Figure 1). The patient returned a few days later and underwent an en-bloc endoscopic ampullectomy. Under conscious sedation, a duodenoscope was passed to the second portion of the duodenum and the major ampulla was located. A sphincterotome was used to access the pancreatic duct which was injected with 4 cc of methylene blue. A polypectomy snare was then used to grasp the base of the ampullary tissue and, with 40 watts pure cut electrosurgical current (ERBE, Marietta, GA), ampullectomy was performed (Figure 2). No immediate bleeding was observed. The specimen was successfully retrieved and submitted to pathology analysis that showed villous adenoma without invasive malignancy. The pancreatic orifice was still canullated and injected methylene blue facilitating a recannulation of the pancreatic duct (Figure 3 a-b) and placement of a 5Fr x 3 cm straight pancreatic stent (Figure 4 a-b). The patient tolerated the procedure well and was discharged home the same day. Following the endoscopic ampullectomy, normalization of the liver enzymes and complete resolution of symptoms were observed. The patient remained asymptomatic, with no evidence of abnormalities by 18 months after the procedure (Figure 5).
¿ Figure 1. Biopsies from the ampulla reported a villous adenoma.
¿ Figure 2. Ampullectomy was performed using a polipectomy snare.
¿ Figure 3 A-B. The pancreatic orifice was still canullated and injected methylene blue facilitating a recannulation of the pancreatic duct.
¿ Figure 4 A-B. Placement of a pancreatic stent.
¿ Figure 5. Endoscopic aspect 18 months after the procedure.
¿ Discussion
Villous adenoma is the most important benign tumor of the ampulla of Vater and is known to be premalignant. Although the rate of developing malignancy in these tumors is controversial, it has been estimated that 30-60% develop in situ or invasive carcinoma if left untreated.2 In addition, adenomatous component is found in 30-35% of all carcinomas of the ampulla of Vater. These tumors originate from the epithelium arising from the bile duct, the pancreatic duct or terminal section of duodenal mucosa. Histologically they show varying levels of differentiation from well to moderate to poor. The growth pattern of some types has been associated with better prognosis, but this has not been confirmed by subsequent reports. It is important to identify these lesions early so that appropriate intervention can be performed.
Malignant tumors of the ampullary region are also uncommon and seen at a rate of 0.02-5% among all gastrointestinal tumors. Operable pancreatic-duodenal tumors are seen at a rate of 10.2-36%. They can be seen in all age groups but the highest frequency is between the ages of 50 and 70 years. They are more common among men with a male/female ratio of 3/1.1,4 The most common clinical finding of ampulla of Vater tumors is obstructive jaundice, which occurs in 80% of the cases. Initially, jaundice shows fluctuation and abdominal pain is quite common (40-60%). Common findings of malignant diseases include fatigue, loss of appetite (in 30% of the cases), nausea and vomiting. Melena, occult blood in the stool with anemia and painless jaundice with dilatation of the gall bladder is a common triad. Blood loss and anemia are not common. In patients who present with jaundice, the period between the onset of jaundice and diagnosis is usually 30 days, whereas in those presenting with complaints such as abdominal pain, nausea and loss of appetite, the period between the onset of symptoms and diagnosis can be almost two months. Local resection is appropriate for patients with small malignant tumors, benign tumors of the ampulla of Vater, or in those patients with high surgical risk. Surgical mortality is low (approximately 10%), and the five year survival ranges between 17% and 40% in patients with advanced lesions.
The most critical point in endoscopic papillectomy is the assessment of its indication. Adenoma of the duodenal papilla without extension into the bile or pancreatic duct is an accepted indication. Cancer in adenoma without invasion of the muscularis propria of the duodenum, pancreas, or extension along the bile or pancreatic duct is also a possible candidate for this treatment, however dysplasia adenoma does not give to EUS a suitable technique condition to determine the loco regional invasion because it is an in situ cancer, so in some occasions, endoscopic papillectomy may be indicated as a total biopsy. The procedure is similar to that in polypectomy of the digestive tract. Following insertion of a duodenoscope into the descending portion of the duodenum, a tumor at the papilla of Vater is caught in a snare loop which is delivered via the channel of the scope, as deep as possible. To achieve this, specially in peridiverticular situation, the tip of the snare should first be put on the top of the oral protrusion as a fulcrum. Then, the entire tumor is trapped in the snare, and the snare is tightened so that it can grasp the bile duct and the pancreatic duct terminals adjacent to the base of the tumor. We apply the 'cut' current for electrocautery to avoid infiltration of the energy to the pancreatic parenchyma. After resection of the tumor, a stent is placed in the pancreatic duct, which will prevent obstruction of the outlet of pancreatic juice that leads to acute pancreatitis, but before that we injected around 2-3 mL of methylen blue solution to facilitate the posterior access. Detailed histological examination is mandatory for the evaluation of the quality of the resection. It is ideal to obtain cut margins, including the bile duct and pancreatic duct terminals, be free of neoplastic cells. Sometimes it is not possible to confirm such free margins due to burn of the tissue. In such occasions, follow-up in a short term is required and when a remnant tumor is recognized, surgical resection or ablation should be added based on the depth of invasion of tumor. Further data and longer follow-up is necessary to justify this procedure as a treatment of choice for the tumors mentioned here.
Correspondence: Everson L.A. Artifon, MD.
Department of Gastroenterology, São Paulo University. Medicine School. Av. Dr. Enéas de Carvalho
Aguiar 255, 9º andar sala 9159, São Paulo, Phone: 05403-000, SP, Brazil.
E mail: eartifon@hotmail.com