Case report
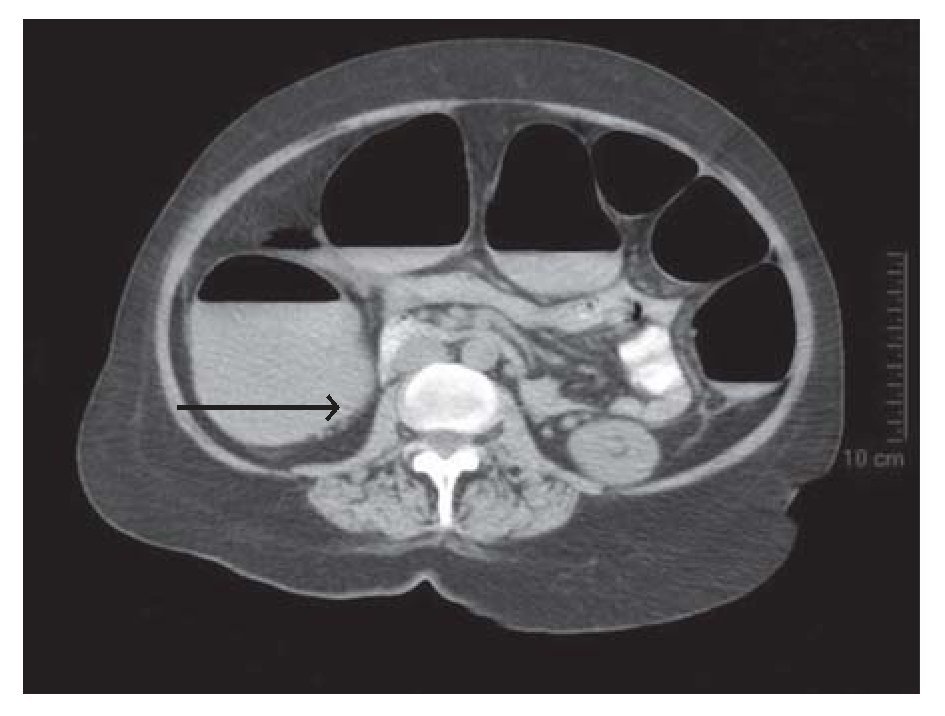
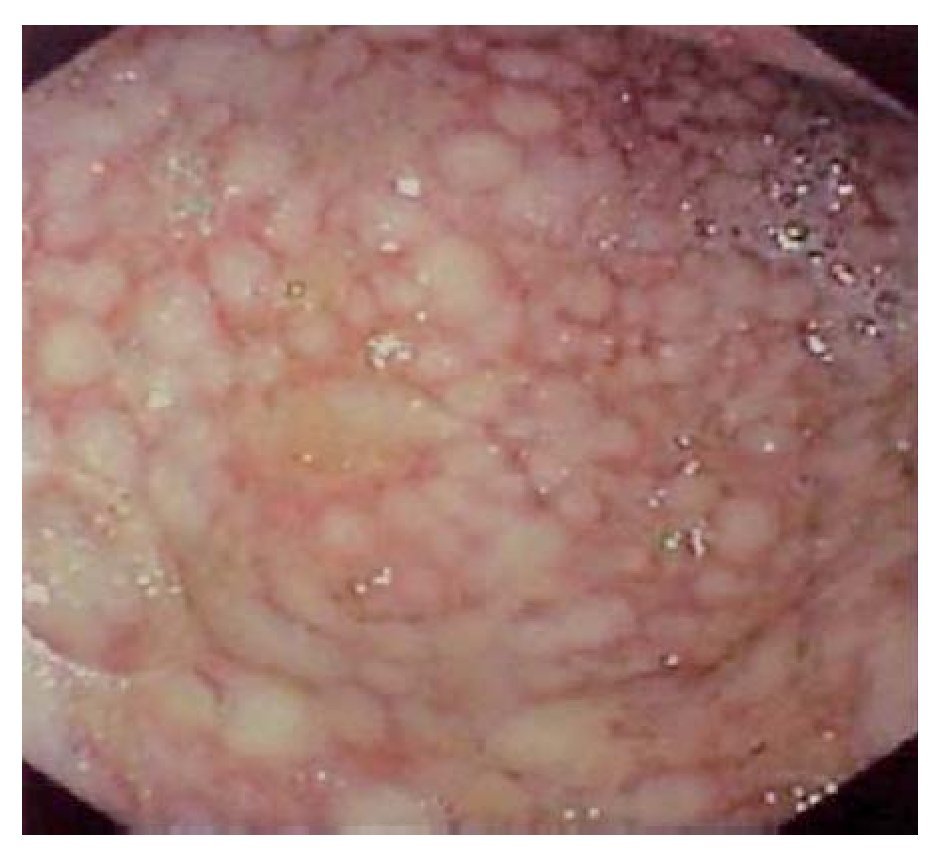
A 63-year-old woman arrived at the Emergency Room complaining of abdominal pain, bloating and diarrhea over three days. A week earlier she had had an upper respiratory tract infection and was treated with oral antibiotics (amoxicillin/clavulanate). Upon physical examination there were signs of mild dehydration and her abdomen was distended and tender on palpation in the left lower quadrant without rebound tenderness. Presumptive diagnosis of antibiotic-related diarrhea vs. gastrointestinal infection led to determination of Clostridium difficile toxin and an abdominal CT scan. A tomography showed minimal mesenteric stranding and pericecal lymphadenopathy without colonic dilation. Both Clostridium difficile toxin A and B tests were negative. The patient was hospitalized for rehydration and levofloxacine and metronidazole were administered intravenously. During the first 24 hours of hospitalization her abdominal girth and pain increased, her mental status deteriorated and eventually she developed signs of septic shock. A new abdominal CT showed a dilated colon (> 6cm) with air liquid levels in the ascending colon without signs of perforation (Figure 1). A flexible sigmoidoscopy with low pressure was performed (Figure 2). Findings in both studies were compatible with pseudomembranous-colitis and the diagnosis of toxic mega-colon was established. The patient was rushed to the operating room where exploratory laparotomy revealed a nonperforated massively dilated colon and an abdominal colectomy with ileostomy was performed. The stump of the Hartmann pouch was stapled and oversewn with interrupted Lem-bert sutures. Postoperatively the patient received intravenous meropenem and metronidazole and the rectum was irrigated with vancomycin. The patient developed respiratory failure and remained in intensive care for two weeks but was eventually dismissed from the hospital eighteen days after surgery. The patient recovered uneventfully and underwent ileorectostomy four months later.
Figure 1. Abdominal CT showing a dilated colon (> 6cm) with air liquid levels in ascending colon without signs of perforation. The arrow indicates an image compatible with neumatosis.
Figure 2. Low-pressure sigmoidoscopy shows colonic mucosa studded with adherent raised yellowish plaques.
Discussion
In the last decade the incidence and severity of Clostridium difficile colitis has markedly increased.1 Clostridium difficile is implicated as the causal organism in 10% to 25% of patients with antibiotic-related diarrhea, in 50% to 75% of those with antibiotic-associated colitis and in 90% to 100% of the cases of antibiotic-associated pseudo-membranous colitis.2,3 Recent use of antibiotics remains the most common risk factor for the development of C. difficile colitis4-5 and while it can occur even after a single dose of almost any antibiotic, clindamicyn, third-generation cephalosporins, and fluorquinolones lead more frequently to Clostridium difficile colitis than others.3 Our patient was treated with antibiotics one week prior the admission to the hospital. The source of infection can be either endogenous or exogenous and symptoms might arise immediately after the antibiotic is started or within 60 days of antibiotic discontinuation.2 Other risk factors associated to Clostridium difficile colitis include patient immunosupression, underlying disease, gastrointestinal surgery, older age, prolonged hospital stay, stay in the ICU and use of proton pump inhibitors or tube feeding.1,3
The characteristics of our patient were similar to those reported by Longo et al.6 These findings included the age of presentation (median 69 years vs. 63 years old, in our patient), a history of antibiotic use (97% of patients in the Longo report) and diarrhea (two thirds of patients had it in their study).
The pathogenesis of Clostridium difficile colitis is complex. The combination of a debilitating disease and antibiotic therapy (sometimes chemotherapy) is thought to alter the bacterial flora of the colon creating conditions that favor the acquisition or proliferation of preexisting Clostridium difficile infection.3 Bacterial proliferation causes acute inflammation of the colon that leads to visceral smooth muscle relaxation resulting in passive colonic dilation. In addition the inflamma-tory process alters the normal bowel absorptive function causing retention of water, sodium, and potassium in the colonic lumen resulting in systemic hypokalemia that leads to increased colonic dismotility.7 The progression of toxic megacolon associated with C. difficile infection is secondary to the breakdown of the intestinal barrier function with translocation of C. difficile toxin into the portal venous system causing cytokine production by hepatic macrophages.8
Various methods are available to diagnose Clostridium difficile-associated disease. These methods include anaerobic culture, direct toxin testing for toxins A and B, detection of the cytopathic effect of the toxins on cell culture assay, detection of Clostridium difficile antigen with subsequent toxin testing of positive samples, and nucleic acid amplification techniques.3 In the case presented, toxins A and B were negative, and this result could be attributed to the low sensitivity and specificity for detecting toxins A and B alone for Clostridium difficile infection (49-66% and 95% respectively).
These false negative results make this test not useful for diagnosis in some cases, such as ours. The gold standard test for diagnosis of C. difficile infection would be the combination of a direct cytotoxi-city assay with a cytotoxic culture in which sensitivity and specificity increase almost to 100%.9 Longo et al. reported the stool cytotoxin assay negative in 18% of their population.6
The clinical presentation of the disease ranges from asymptomatic colonization to fulminant colitis associated with multiple organ failure and shock.1,2,4 Nevertheless, the most common presentation is Clostridium difficile-associated diarrhea, with or without pseudo-membranes in the wall of the colon.5 Mild to moderate disease usually causes lower cramping abdominal pain but can occur even in the absence of abnormal symptoms or physical findings. Moderate to severe colitis usually causes profuse diarrhea, abdominal distension with pain and occult colonic bleeding in some cases. Systemic findings such as fever, nausea, anorexia and malaise are usually also present in the latter.3 Our patient progressed rapidly from mild colitis to toxic megacolon with an abrupt clinical deterioration.
Toxic megacolon is an unusual but well-recognized presentation of the C. difficile colitis spectrum.1 Toxic megacolon is a life-threatening complication of C. difficile colitis characterized by acute segmental or total dilation of the colon to a diameter greater than 6cm associated with signs of systemic toxicity.1,6 Although toxic megacolon is more commonly related to inflamma-tory bowel disease (1 to 2.5% lifetime risk) and occurs in 10% of patients admitted to a hospital for ulcerative colitis in developed countries, it also occurs in 0.4% to 3% of patients with C. difficile colitis1,3 and these figures may underestimate the incidence of infectious toxic megacolon in developing nations. Risk factors for the development of toxic megacolon include discontinuation of pharmacotherapy for inflammatory bowel and the use of barium enemas, endoscopy, or medications that slow down colonic motility such as narcotics or anticholinergic drugs.1,6 Typical CT findings include segmental or total dilation of the colon with increased wall thickness, the presence of an "accordion sign" (trapped contrast material and thickened haustral folds lining up in parallel fashion), "target sign" (consisting of three concentric rings of alternating high, low and high density) as well as pericolonic stranding, ascites, pleural effusion and subcutaneous edema. The colon diameter often exceeds the 6cm required to establish radio-graphic compatibility with toxic megacolon.1,4,10 Endoscopic features of pseudo-membranous colitis are pathognomonic for this disease showing a colonic mucosa studded with adherent raised yellowish plaques that can easily be dislodged.4-5 If mucosal examination of the colon is performed for diagnostic purposes it should be limited to sigmoidoscopy with minimal insufflation to reduce the risk of perforation.1
Surgery is required in most cases (65 -71%) of toxic megacolon due to C. difficile pseudo-membranous colitis8 and carries elevated mortality rates (35% to 80%).1,4 Obvious indications for surgery in this setting include the development of peritonitis, colonic perforation and fulminant colitis refractory to medical treatment, but the sole presence of toxic megacolon might dictate immediate surgery because delaying such treatment may lead to multiple organ dysfunction syndrome with mortality rates approaching 100%.8
In this case, the remaining colon was irrigated with intracolonic vancomycin (ICV) after surgery. This procedure was used because the review of the archived literature for ICV for C. difficile colitis, showed that 83 percent of all reported C. difficile cases had clinical and microbiological response to adjunctive therapy.2,11
In conclusion, patients admitted to the hospital with pseudo-membranous colitis must be followed closely for signs of disease progression. Patient condition deterioration must prompt diligent reevaluation to exclude toxic megacolon. Toxic megacolon due to C. difficile colitis must trigger immediate surgical consultation and operative intervention to save the patient's life.
Correspondence author: Miguel Ángel Sánchez Pérez.
Carlos Graef Fernández 154-517, Col. Tlaxala, CP 05300, Mexico City.
Tel/Fax: (5255) 1664 7164.
E mail:wfrguitarma@hotmail.com