A 41-year-old woman with an unremarkable medical history presented with abdominal pain, associated with jaundice and weight loss of 10 kg in one month, as well as elevated transaminase levels.
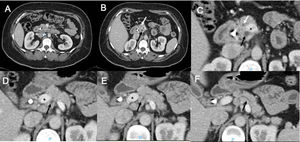
In the initial approach, endoscopic retrograde cholangiopancreatography was performed, with transpapillary biliary drainage via a stent. An ampullary lesion was identified and the histopathologic report stated moderately differentiated adenocarcinoma. The patient was referred to our hospital. A computed tomography scan revealed a dilated common bile duct secondary to an ampullary lesion. The main pancreatic duct (MPD) was situated in a retroportal position and pancreatic tissue encircled the portal vein and the splenoportal confluence (Fig. 1).
The patient underwent a pylorus-preserving Whipple procedure (pancreaticoduodenectomy), with a 2-step resection of the pancreas. First, the anteportal portion was divided, revealing an accessory pancreatic duct, with a 5 mm diameter. The retroportal portion was then divided, revealing the MPD, with a 1.5 mm diameter. Gross pathologic examination identified a tumor measuring 1.6 × 1.6 cm, located on the ampulla of Vater, 1/10 positive lymph nodes (peripancreatic), and tumor-free surgical margins. Microscopic examination showed a moderately differentiated intestinal-type adenocarcinoma. The patient’s postoperative course was uneventful, and she received 8 cycles of capecitabine/gemcitabine adjuvant chemotherapy. The patient is currently in active follow-up with the oncology service and the latest control imaging study revealed local recurrence of the disease, 27 months from the initial diagnosis.
Annular pancreas is a rare condition characterized by circumferential involvement of another anatomical structure. Portal annular pancreas (PAP) is the rarest congenital anomaly of the pancreas, with an incidence around 1.14%.1,2 This anatomic variant is the result of an aberrant fusion of the uncinate process of the pancreas, with complete portal encasement and/or splenoportal confluence.3,4 PAP is classified depending on the running patterns of the MPD: type 1 (retroportal MPD), type 2 (type 1 associated with pancreas divisum), and type 3 (anteportal MPD); or in accordance with its relation to the portal confluence: suprasplenic, infrasplenic, and mixed types, respectively.1–5
In Mexico, there are no publications related to PAP. Ours is the first report in Latin America on pancreaticoduodenectomy in a patient with the anomaly. PAP is usually asymptomatic and tends to be an incidental finding. However, its preoperative diagnosis is crucial for identifying the precise topography of the MPD and planning the surgical strategy well, thus reducing the risk of the main complication: postoperative pancreatic fistula.
Care must be taken in the parenchymal resection, so that there is a lower risk of postoperative pancreatic fistula, as well as better short-term and long-term results.6 In cases of PAP, preoperative and intraoperative confirmation of pancreatic ductal system integrity is of the utmost importance, to avoid technical problems at the time of pancreatoduodenectomy.
Ethical considerationsInformed consent for receiving treatment was requested from the patient. The authors obtained informed consent from the patient for the publication of data/images and the present scientific letter was approved by the institutional ethics committee.
Financial disclosureNo financial support was received in relation to this article.
Conflict of interestThe authors declare that there is no conflict of interest.
Please cite this article as: Castro E, Sánchez-Morales GE, Hernández-Acevedo JD, Sánchez García-Ramos E, Chan C. Adenocarcinoma ampular en un paciente con páncreas anular portal: relevancia del abordaje quirúrgico en el procedimiento de Whipple. Revista de Gastroenterología de México. 2022;87:116–118.