The Tokyo Guidelines for the severity classification of acute cholecystitis (AC) include leukocytosis as a severity classifier, without considering C-reactive protein (CRP). Our aim was to determine which of the two variables has a greater predictive capacity for local complications in AC (LCAC).
Material and methodsA retrospective single-center study was conducted on patients that underwent emergency cholecystectomy within the time frame of June 2022 and December 2023. The variables associated with LCAC were analyzed and an ROC analysis was carried out.
ResultsThe multivariate analysis of 145 patients identified the following associations with LCAC: CRP (p < 0.001; OR 11.8), AUC of 0.88 (p = 0.029), and cutoff point of 4 mg/dl (88% sensitivity, 71% specificity); leukocytosis (p < 0.031; OR 5), AUC of 0.81(p = 0.037), and cutoff point of 11.09 x 109/l (78% sensitivity, 70% specificity).
ConclusionsCRP may have a higher predictive capacity for LCAC than leukocytosis.
En la clasificación de severidad de las Colecistitis Agudas (CA) de las Guías de Tokio se incluye la leucocitosis como clasificador de severidad sin considerar la Proteína C-Reactiva (PCR). El objetivo es determinar cuál posee mayor capacidad predictiva de complicación local en las CA (CLCA).
Material y métodosSe trata de un estudio retrospectivo y unicéntrico de los pacientes intervenidos de colecistectomía urgente desde junio de 2022 hasta diciembre de 2023. Se analizó qué variables se asociaban con la CLCA y se realizó un análisis ROC.
ResultadosDe los 145 pacientes, en el análisis multivariante se asociaron con la CLCA: la PCR (p < 0,001; OR = 11,8), ABC 0,88(p = 0,029) y punto de corte de 4 mg/dL (sensibilidad 88%, especificidad 71%); y la leucocitosis (p < 0,031; OR = 5), ABC de 0,81(p = 0,037) y punto de corte de 11,09 x 109/L (sensibilidad 78%, especificidad 70%).
ConclusionesLa PCR podría presentar una mayor capacidad predictiva para CLCA que la leucocitosis.
Acute cholecystitis is one of the most frequent surgical emergencies in our environment, and 200,000 hospital admissions are reported in the United States every year.1 Emergency cholecystectomy is the treatment of choice, if patient clinical conditions allow it, and the grade of severity is related to morbidity and mortality.2,3 The 2018 Tokyo Guidelines,2 the most extensive consensus guidelines for biliary disease management, guide us toward a different therapeutic approach, depending on the severity of the clinical picture.
In those guidelines, leukocytosis (> 18 × 109/l) is the only laboratory parameter for classifying severity as moderate (grade II), and strikingly, C-reactive protein (CRP), a laboratory test used in daily clinical practice with a demonstrated relation to intra-abdominal infection, is not included. The presence of local complications in acute cholecystitis (LCAC) is also a symptom severity marker and serves as a classifying criterion.
The primary aim of our study was to determine whether CRP or leukocytosis had the greater predictive capacity for LCAC in acute cholecystitis treated urgently.
Determining what other factors were possibly related to LCAC was the secondary aim.
Material and methodsA retrospective, observational, single-center study was conducted on patients >18 years of age diagnosed with acute cholecystitis that underwent emergency cholecystectomy within the time frame of June 2022 and December 2023.
We determined the presence of local complications (gangrene, perforation, abscess), based on the intraoperative findings during surgery.
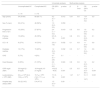
Table 1 shows the demographic variables, progression time from the onset of clinical symptoms to the intervention, mean hospital stay, the severity grade according to the Tokyo Guidelines, CRP level at admission, leukocytosis, and positive cultures of the biliary fluids obtained during the intervention analyzed.
Univariate and multivariate analyses between uncomplicated acute cholecystitis and complicated acute cholecystitis.
| Univariate analysis | Multivariate analysis | |||||||
|---|---|---|---|---|---|---|---|---|
| Uncomplicated AC | Complicated AC | OR (95% CI) | p value | β | β error | OR (95% CI) | p value | |
| n = 70 | n = 75 | |||||||
| Age (years) | 54 (50-60) | 68 (65-71) | 6.2 (4.1 - 7) | 0.012 | 0.01 | 0.6 | 1.01 (0.3 - 3.2) | 0.9 |
| Sex (% men) | 32 (41%) | 46 (59%) | 1.3 (0.6 - 2.5) | 0.059 | - | - | - | - |
| Progression time ≥ 72 h | 13 (33%) | 27 (67%) | 2.4 (1.1 - 5.3) | 0.019 | 0.5 | 0.6 | 1.9 (0.5 - 5.6) | 0.2 |
| Positive cultures | 13 (22%) | 45 (78%) | 6.5 (3 - 14) | < 0.001 | 0.8 | 0.5 | 2.4 (0.8 - 6.9) | 0.1 |
| CCI > 6 | 6 (27%) | 16 (73%) | 2.9 (1 - 7.8) | 0.032 | 0.1 | 0.8 | 1.1 (0.2 - 5.6) | 0.8 |
| Diabetes mellitus | 12 (17%) | 15 (20%) | 1.2 (0.6 - 1.2) | 0.032 | 0.3 | 0.7 | 1.4 (0.4 – 5.2) | 0.6 |
| CKD | 5 (7%) | 4 (5%) | 0.7 (0.1 - 2.8) | 0.1 | - | - | - | - |
| Heart disease | 9 (30%) | 21 (70%) | 2.6 (1.1 - 6.2) | 0.024 | 0.8 | 0.6 | 1.2 (0.3 - 4.3) | 2.2 |
| CRP mg/dl (IQR) | 3.8 mg/dl (2 - 6 mg/dl) | 18.4 mg/dl (16 - 21 mg/dl) | 16 (6.2 - 40.6) | < 0.001 | 2.5 | 0.5 | 12.5 (4.3 - 36.1) | < 0.001 |
| Leukocytosis μ x 109/l (IQR) | 9.6 μ x 109/l (8.4-10.8 μ x 109/l) | 15.7 μ x 109/l (14.3- 17.1 μ x 109/l) | 7.7 (3 - 19) | < 0.001 | 1.47 | 0.7 | 5 (1.1 - 16.7) | 0.031 |
| Hospital stay (days) (IQR) | 3.8 (2.2-4.5) | 5.4 (4-7.5) | 1.5 (0.5 – 11) | 0.09 | - | - | - | - |
AC: acute cholecystitis; CCI: Charlson comorbidity index; CKD: chronic kidney disease; CI: confidence interval; CRP: C-reactive protein; DM: diabetes mellitus; IQR: interquartile range; OR: odds ratio.
The data analysis was carried out using the IBM SPSS Statistics v20.0® program.
Nonparametric distribution of the quantitative variables was confirmed through the Kolmogorov-Smirnov test and analyzed using the Mann-Whitney U test. The qualitative variables were analyzed using the Pearson chi-square test.
We performed a univariate analysis on each of the factors associated with LCAC, after which we ruled out confounding factors with a multivariate analysis. We determined the 95% confidence intervals (CIs). A p ≤ 0.05 was considered statistically significant.
A receiver operating characteristic (ROC) analysis was carried out on CRP and leukocytosis to compare their area under the curve (AUC), and a cutoff point offering the best sensitivity and specificity was established for the two parameters.
We divided the following variables into 2 groups: Charlson comorbidity index (CCI) scores, progression time, cultures obtained, CRP levels, and leukocytosis values. Cholecystitis present for more than 72 hours was considered to have progressed and a CCI score > 5 signified a patient with important comorbidity.2 Patients with negative cultures and those in whom no cultures were carried out (due to having uncomplicated cholecystitis) were placed together in the control group. For CRP, the established cutoff point of 7.6 mg/dl was considered elevated (based on the cutoff points established by Bouassida et al.4 and by Kabul et al.5), and for leukocytosis, the cutoff point was 18 × 109/l, based on the 2018 Tokyo Guidelines.
Ethical considerationsNo experiments on animals or humans were conducted for the present article and the data publication protocols of our work center were followed, preserving patient anonymity.
ResultsOf the 145 patients included in the study, 70 presented with uncomplicated acute cholecystitis and 75 with complicated acute cholecystitis. As shown in table 1, the simple univariate analysis revealed a significant association with LCAC: CRP > 7.6 mg/dl (p < 0.001; OR 16), leukocytosis (p < 0.001; OR 7.7), CCI > 5 (p = 0.032; OR 2.9), history of heart disease (p = 0.024; OR 2.6), progression time (p = 0.019; OR 2.4), age (p = 0.012; OR 6.2), diabetes mellitus (p = 0.032; OR 1.2), and biliary fluid culture positivity (p < 0.001; OR 6.5).
The multivariate analysis revealed significant differences only in CRP (p < 0.001; OR 12.5) and leukocytosis (p < 0.031; OR 5).
An ROC analysis was then carried out on CRP and leukocytosis, regarding the presence of LCAC. For leukocytosis, we obtained an AUC of 0.81, establishing a cutoff point of 11.09 × 109/l that provided 78% sensitivity and 70% specificity for predicting LCAC. For CRP, the AUC was 0.88, with a cutoff point of 4 mg/dl that had 88% sensitivity and 71% specificity for said prediction.
DiscussionThe CRP level regarding the presence of intra-abdominal infection has been previously studied, and thanks to studies such as the one by Bouassida et al.4 or by Mok et al.,6 we know that the CRP level is significantly related to the presence of LCAC and conversion rates to open surgery, offering a greater predictive capacity than leukocytosis. Strikingly, some of the scores that have been described for predicting gangrene in acute cholecystitis, such as those of Yacoub et al.7 and Bouassida et al.,4 do not include CRP as a predictive factor of local complications either, knowing that the accessibility and cost of the test is similar to those of the leukocytosis test.
Our cutoff point for CRP (4 mg/dl) as a LCAC predictor is close to those found in other studies, such as the analyses by Mahmood et al.8 (5.5 mg/dl), Bouassida et al.4 (7.6 mg/dl), and Kabul et al.5 (7.6 mg/dl), albeit sensitivity and specificity is somewhat higher in our study than in theirs. Higher CRP cutoff points reported in the studies by Mok et al.6 (20 mg/dl) and Díaz-Flores et al.9 (11 mg/dl) increased sensitivity but resulted in lower specificity. Díaz-Flores et al. obtained high specificity and sensitivity (82% and 92%, respectively) but the discrimination between groups was based on the technical difficulty perceived by the surgeon, which may be modified by factors different from the presence of local complications.
On the other hand, even though a high level of leukocytosis was a less sensitive marker than CRP in our sample, it had a similar specificity and was also significantly associated with LCAC. A score that includes CRP and evaluates the cost-effectiveness of other acute phase reactants related to intra-abdominal infection severity, such as procalcitonin, could be of interest.10
ConclusionDespite our study’s limitations, its results suggest that CRP may be a more sensitive biomarker than leukocytosis, with a greater capacity for predicting LCAC and determining the severity grade, which would aid us in providing more adequate clinical management and decision-making.
Financial disclosureNo financial support public or private, was received in relation to this article.
The authors declare that there is no conflict of interest.