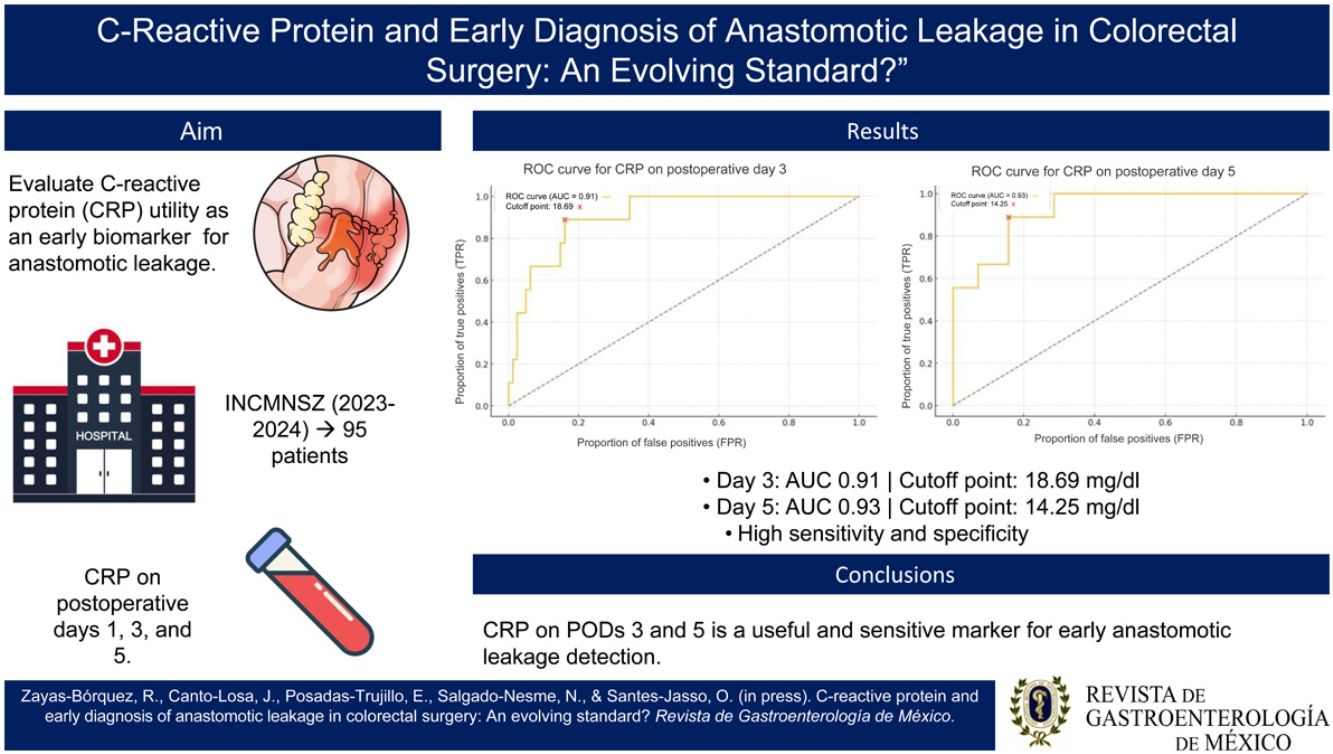
Anastomotic leakage is a critical complication in colorectal surgery, significantly associated with postoperative morbidity and mortality. Early detection of at-risk patients is essential for optimizing clinical outcomes. The present study investigates the utility of C-reactive protein (CRP) as a predictive inflammatory biomarker for anastomotic leakage.
Materials and methodsA retrospective observational study was conducted at the Instituto Nacional de Ciencias Médicas y Nutrición Salvador Zubirán, analyzing 95 patients who underwent colorectal surgery within the time frame of March 2023 and July 2024. CRP levels were measured on postoperative days 1, 3, and 5. The predictive capacity was measured through ROC curves, determining the optimum cutoff points with the Youden index.
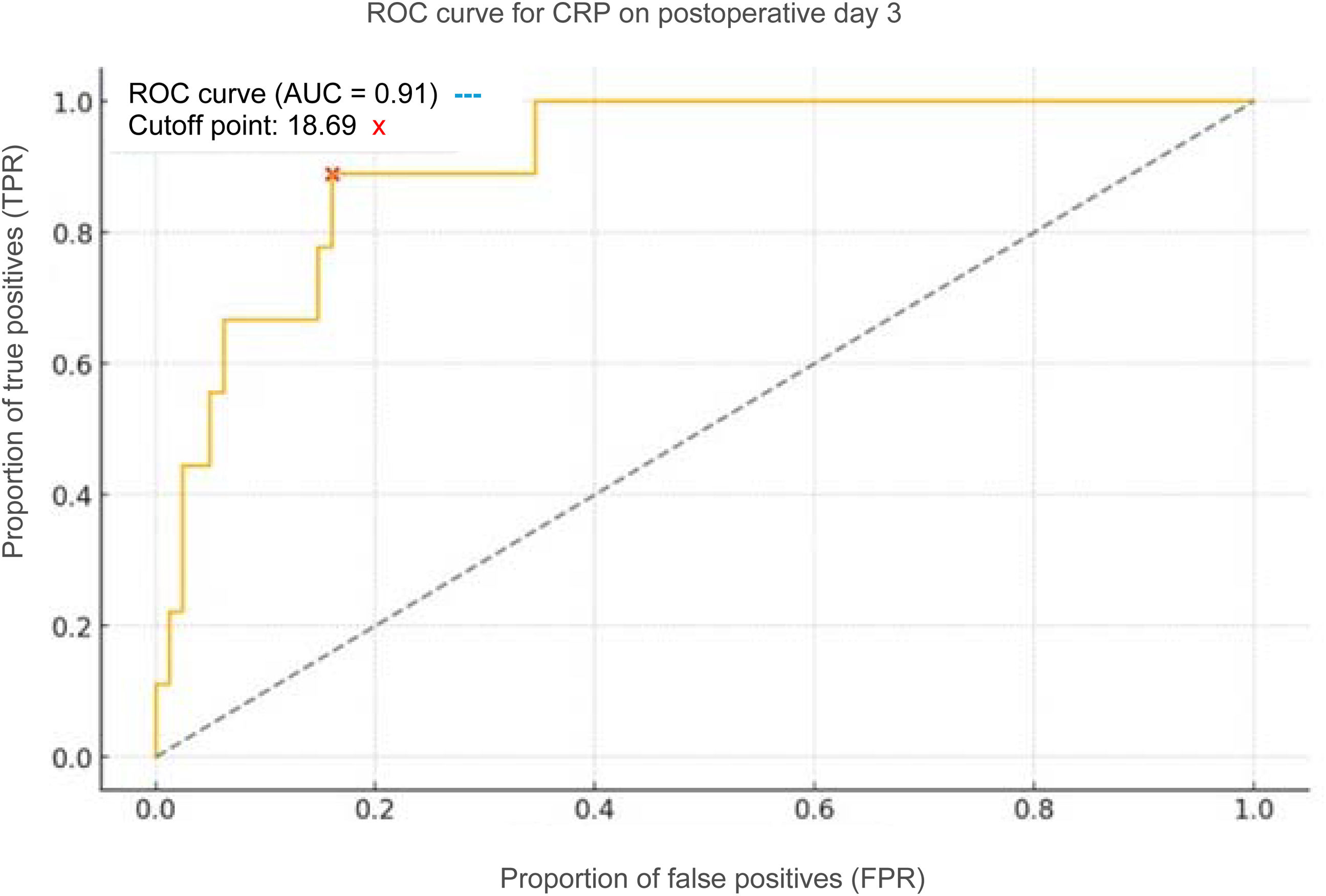
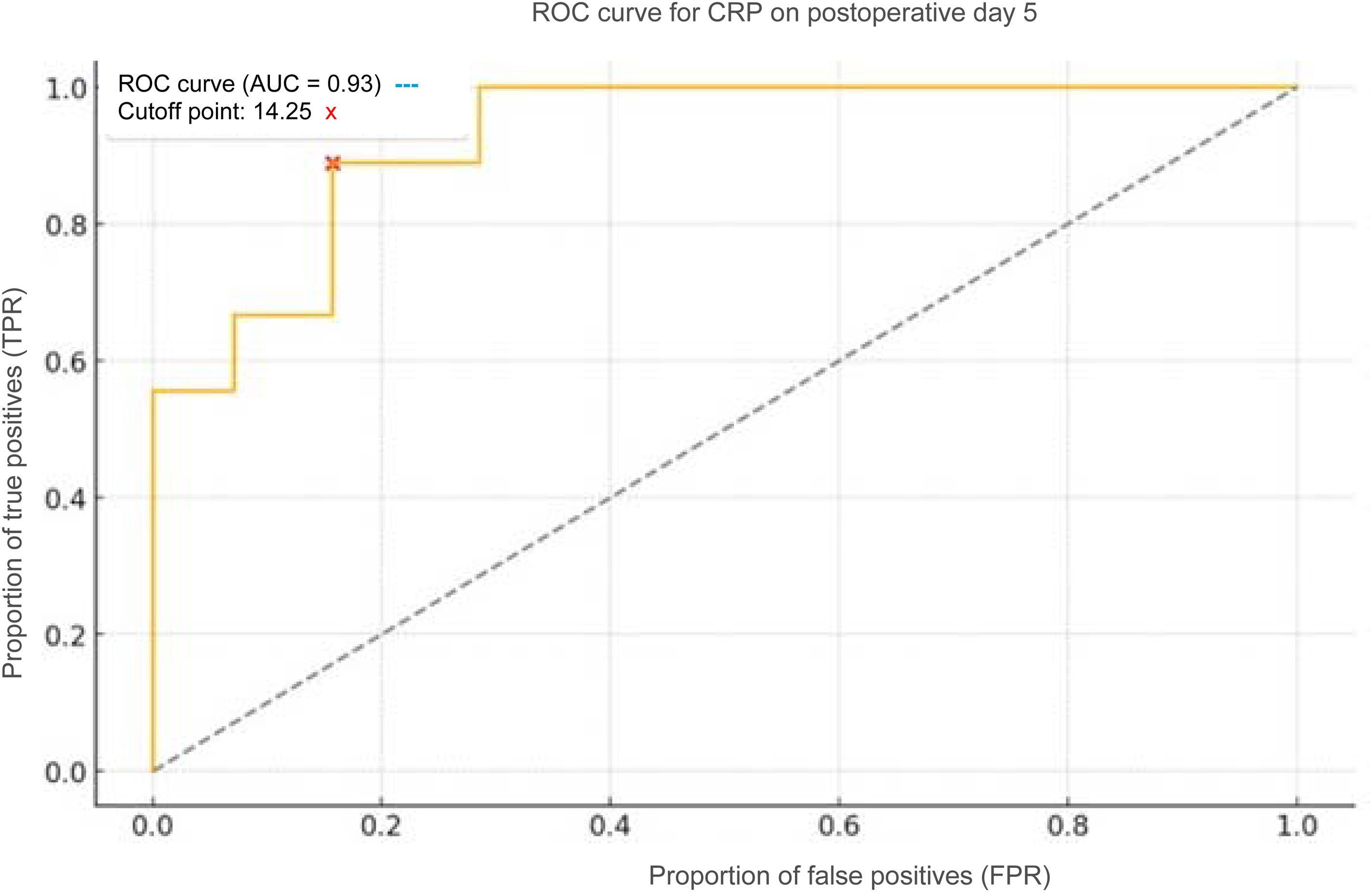
ResultsCRP on day 3 showed an AUC of 0.91, with an optimum cutoff point of 18.69 mg/l (Youden index = 0.73). On day 5, the AUC was 0.93, with a cutoff point of 14.25 mg/l (Youden index = 0.73). Both measurements showed high sensitivity and specificity for predicting anastomotic leakage.
ConclusionElevated CRP levels on postoperative days 3 and 5 emerged as robust predictors of anastomotic leakage, potentially guiding early interventions and improving patient prognosis.
La fuga anastomótica representa una complicación crítica en la cirugía colorrectal, asociada significativamente con morbilidad y mortalidad postoperatoria. La detección temprana de pacientes en riesgo es esencial para optimizar los resultados clínicos. Este estudio investiga la utilidad de la proteína C reactiva (PCR) como biomarcador inflamatorio predictivo de fuga anastomótica.
Materiales y métodosSe realizó un estudio observacional retrospectivo en el Instituto Nacional de Ciencias Médicas y Nutrición Salvador Zubirán, analizando a 95 pacientes que se sometieron a cirugía colorrectal con anastomosis entre marzo de 2023 y julio de 2024. Los niveles de PCR se midieron en los días postoperatorios 1, 3 y 5. Se evaluó la capacidad predictiva mediante curvas ROC, determinando los puntos de corte óptimos con el índice de Youden.
ResultadosLa PCR en el día 3 mostró un AUC de 0.91, con un punto de corte óptimo de 18.69 mg/L (Índice de Youden = 0.73). En el día 5, el AUC fue de 0.93, con un punto de corte de 14.25 mg/L (Índice de Youden = 0.73). Ambos mostraron alta sensibilidad y especificidad para predecir fuga anastomótica.
ConclusiónLos niveles elevados de PCR en los días postoperatorios 3 y 5 emergen como predictores robustos de fuga anastomótica, con potencial para guiar intervenciones tempranas y mejorar el pronóstico del paciente.
Anastomotic leakage (AL) is an important concern in colorectal surgery, with incidence rates that vary from 3 to 19%, influenced by surgical technique, anastomosis location, and patient factors.1 Radiologic anastomotic leakage is defined as the presence of extraluminal contrast material, gas, or liquid adjacent to the anastomosis, or a collection in the proximity of the anastomosis suggestive of communication with the intestinal lumen, detected through computed tomography (CT) or contrasted studies. This complication significantly contributes to morbidity and mortality, prolongs hospital stay, increases healthcare costs, and often requires additional surgical interventions.2 The reported worldwide prevalence varies from 4 to 26%, depending on the type of procedure and patient characteristics.3 Early identification is vital, given that late diagnosis may worsen clinical outcomes.4
There is growing interest in the search for reliable biomarkers for improving early detection of AL. C-reactive protein (CRP), an acute phase reactant synthetized by the liver during inflammatory responses, has emerged as a promising indicator for postoperative complications, including infections and AL.5 Persistent elevations of postoperative CRP have been linked to septic complications, turning it into a valuable marker.6 In that context, the present study aimed to evaluate the predictive capacity of CRP levels, measured on postoperative days 1, 3, and 5, for the early detection of AL in patients who underwent colorectal surgery.
Materials and methodsA retrospective, observational cohort study was conducted at the Instituto Nacional de Ciencias Médicas y Nutrición Salvador Zubirán in Mexico City. The analysis focused on the clinical records of patients who underwent colorectal surgery with anastomosis, within the time frame of March 2023 and July 2024. The study included 95 patients, selected based on the complete availability of data on CRP, albumin, globulin, leukocytes, and neutrophils corresponding to postoperative days (PODs) 1, 3, and 5.
To guarantee transparency, reproducibility, and quality of the scientific report, this manuscript was developed in accordance with the recommendations of the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) checklist, a tool designed for optimizing the presentation of observational studies.
Given the retrospective and exploratory nature of the study, a previous calculation of sample size was not carried out. Instead, the total number of patients who met the inclusion criteria during the established study period were included. Patients with pre-existing infections or who were receiving immunosuppressive treatment, and cases with incomplete or ambiguous clinical records were excluded. To reduce possible information biases, strict selection criteria were applied, and data were cross verified by two independent researchers.
The variables analyzed included serum levels of CRP, albumin, total proteins, and leukocyte and neutrophil counts on PODs 1, 3, and 5. The dependent variable was the presence or absence of AL. It was the only dependent variable and was considered dichotomous (0 = no leakage, 1 = leakage), standardizing the definition, for purposes of the study, as that which could be demonstrated through an imaging study.
To evaluate normality in the distribution of CRP levels between groups, with and without AL, the Shapiro-Wilk test was applied, which indicated non-normal distribution (p < 0.05). Consequently, the nonparametric Mann-Whitney U test was utilized to compare the CRP levels between the two groups. The results showed highly statistically significant differences in the CRP levels on POD 3 (p = 0.00016) and POD 5 (p = 0.000047) (p < 0.001).
Statistical analysisTo evaluate the predictive capacity of CRP levels in detecting AL, receiver operating characteristic (ROC) curves were constructed. From those curves, the optimum cutoff point was determined using the Youden index. Sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) corresponding to the cutoff points were calculated. In addition, a Pearson correlation analysis was carried out to explore the progression of the CRP levels throughout the postoperative period. That additional analysis was decided upon because the aim was to evaluate the directional consistency and relational strength between values, not to compare the values with each other.
Ethical considerationsThis study required no approval by the Research Ethics Committee of the Instituto Nacional de Ciencias Médicas y Nutrición Salvador Zubirán nor individual statements of informed consent because it is a retrospective, observational study with no contact with patients, based on the analysis of clinical records. In addition, the data were anonymized prior to their analysis to protect the identity of the subjects.
The present study conforms to the ethical principles established in the Declaration of Helsinki, the guidelines of the 2016 CIOMS (Consejo de Organizaciones Internacionales de las Ciencias Médicas), and the national regulation in health research.
ResultsOf the 95 patients included in the study, 85.26% of them underwent elective surgery and 14.74% underwent emergency surgery due to different causes, such as intestinal obstruction and perforation. Malignant disease was diagnosed surgically in 68.42% of the patients and benign disease in 31.58%.
Mean patient age was 60 years, 38 of the 95 patients studied were between 60–69 years of age, 54 of the 95 patients were women, and 41 were men.
The most frequent anastomoses performed were colorectal anastomosis, at 36.84%, and ileocolonic anastomosis, at 32.63%. The remaining procedures were ileorectal, coloanal, colocolic, and enteroenteric anastomoses, together at 30.53%.
The incidence of leakage in our study was 9.47%.
In the present analysis, there were no statistically significant differences between the groups with and without AL, in relation to serum levels of leukocytes, neutrophils, total proteins, or albumin, on PODs 1, 3, and 5 (p > 0.05 in all cases). Those findings suggest that said biomarkers lack discriminative value in the context of early diagnosis of AL in our cohort.
Importantly, procalcitonin determination is not routinely performed in the postoperative follow-up at our hospital center, and so was not included in the analysis.
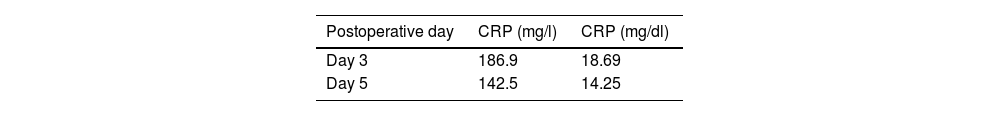
In the diagnostic yield analysis of CRP for detecting AL, serum level measurements were evaluated on PODs 3 and 5 (Table 1). The predictive capacity was analyzed through ROC curves, with both measurements providing an excellent yield.
On POD 3, the ROC curve produced an area under the curve (AUC) of 0.91, indicating high diagnostic accuracy. The optimum cutoff point determined through the Youden index was 18.69 mg/dl, with 85% sensitivity and 88% specificity (Fig. 1). On POD 5, the AUC was even higher, at 0.93, with an optimum cutoff point of 14.25 mg/dl, with 90% sensitivity and 85% specificity (Fig. 2). Those results reflect improvement in the discriminative capacity of CRP, with the increased number of PODs.
There was a strong positive correlation between CRP levels on POD 3 and POD 5 (r = 0.82, p < 0.001). That finding suggests a consistent progression in CRP levels in patients with poor progression, which could support its clinical utility as a dynamic marker for postoperative follow-up.
DiscussionThe primary aim of our study was to evaluate CRP utility as an early predictive marker of AL. This design involves evaluating the diagnostic or predictive capacity of a single biomarker (CRP), with no initial multivariate adjustment that could introduce unnecessary overadjustment in a model whose aim is to maintain diagnostic simplicity.
Our findings concur with those of previous studies that highlight the potential of CRP in the early detection of AL. The elevated CRP levels on PODs 3 and 5 showed high sensitivity and specificity, similar to that reported by Messias et al.,3 who documented an AUC of 0.82 for CRP on POD 4, with a NPV of 97.2%.
Similarly, Almeida et al.2 identified a CRP threshold of 140 mg/l on POD 3, as optimal for balancing sensitivity and specificity. García-Granero et al.4 reinforced PCR and procalcitonin utility in major AL, with AUC values above 0.80 between PODs 3 and 5.
Nevertheless, there are discrepancies regarding the ideal cutoff points. Pantel et al.5 reported a threshold of 147 mg/l on POD 3, with a NPV of 99%. Stephensen et al.6 highlighted the predictive value of the CRP trajectory, demonstrating an AUC of 0.961. Reisinger et al.7 pointed out that combining CRP and calprotectin improved diagnostic accuracy in the early detection of AL.
Other studies, including the analysis by García-Granero et al.,4 suggest that procalcitonin could surpass CRP in the detection of major AL, promoting a multimodal approach. Almeida et al.2 emphasize that variations in surgical techniques and postoperative care impact CRP interpretation, underlining the need for individual adjustments in the cutoff points, similar to that found in other studies.8–12
Together, those findings lend support to CRP as an essential biomarker for the early detection of AL. However, careful interpretation that takes into account individual surgical and clinical factors is crucial.
LimitationsThe main limitations of our study are its retrospective design and small sample size, which could limit the generalization of the results. In addition, other inflammatory biomarkers that could complement or reinforce the predictive capacity of CRP were not considered. Those limitations provide opportunities for future research, particularly prospective and multicenter studies to validate current findings. Likewise, future lines of research could focus on evaluating the combination of CRP and other markers, such as procalcitonin or calprotectin, as well as the development of predictive models that integrate clinical and laboratory data to improve early AL detection.
ConclusionsOur study confirms CRP as a reliable predictor of AL in colorectal surgery, especially on PODs 3 and 5. Systemic monitoring of CRP could facilitate early detection, enabling the performance of early interventions to reduce the morbidity and mortality associated with this serious complication.
Adequate CRP value monitoring should alert the physician as to possible complications, of which AL is one of the most dreaded, and motivate the performance of imaging studies to rule out or confirm AL, providing timely management even before clinical manifestations are evident.
The serial measurement of CRP values is increasingly becoming an evolving standard for the early surveillance of AL in colorectal surgery, and the accumulating evidence suggests it is in the process of becoming a reality.
Financial disclosureNo financial support was received in relation to this study/article.
The authors declare that there is no conflict of interest. There were no personal or financial relations with other persons or organizations that could inappropriately influence (bias) our work.