According to the Globocan 2022 estimates, colorectal cancer (CRC) is the third most common cancer worldwide and the second leading cause of cancer-related deaths.1 In Peru, it is the fourth most common malignant neoplasm and the fourth leading cause of cancer-related deaths.1 It is important to note that approximately 20% of patients with CRC present with metastatic disease.2 This pathology tends to metastasize to various sites in the body, the most frequent of which are the liver, lungs, peritoneum, lymph nodes, bones, and brain.2 Skin metastases are uncommon. The most common primary sources are lung and breast cancers. Cutaneous metastases from rectal adenocarcinoma are even rarer, occurring in less than 4% of patients, but when they do occur, it indicates that the cancer is in an advanced stage.3 These metastases usually appear in the perineal area, abdomen, or around surgical scars or fistulas, but they can also manifest in other areas of the body.2,4 Importantly, the presence of cutaneous metastases is generally associated with a poor prognosis because it indicates systemic dissemination of the cancer.2,4
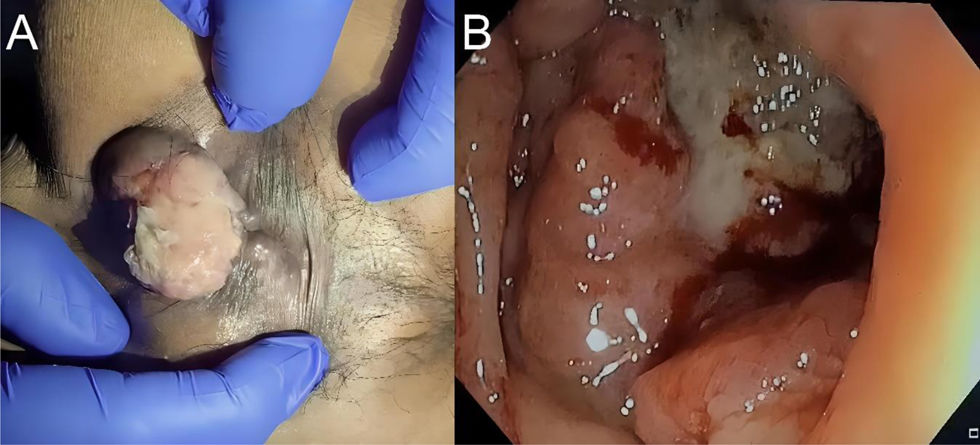
We present the case of a 62-year-old male with a 6-month history of illness characterized by pain in the perianal region and rectal bleeding. Physical examination revealed an irregular lesion measuring 3 × 5 cm on the posterior side of the anal margin. The defect was slightly mobile, painful, friable, and there were no palpable lesions in the rectum (Fig. 1A).
The colonoscopic study revealed a proliferative lesion with an irregular surface and areas of fibrosis measuring 3 × 5 cm in the region adjacent to the posterior side of the anal margin. The sphincter was normotonic, not painful, with no involvement of the pectineal line. The endoscopy also revealed an infiltrating proliferative lesion with a nodular and ulcerated surface in the rectal region, starting 8 cm from the pectineal line and extending up to 15 cm. This lesion involved the entire circumference and narrowed the lumen by 70% (Fig. 1B). Biopsies were taken from both lesions.
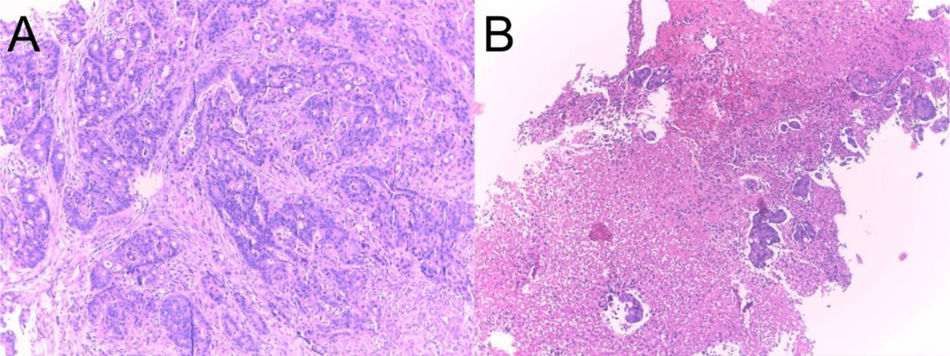
The histopathological result of the lesion adjacent to the anal margin was ulcerated low-grade infiltrating adenocarcinoma (NOS) (Fig. 2A). Similarly, the ulcerated and infiltrating lesion in the rectum was reported as ulcerated low-grade infiltrating adenocarcinoma (NOS) (Fig. 2B).
Tomography identified pulmonary metastatic involvement. Given the clinical stage (stage IV) with perianal and lung metastases, as well as the patient’s age and the tumor differentiation grade, palliative chemotherapy was chosen.
Metastatic spread of cancer can occur through various pathways. The main routes of dissemination include hematogenous, lymphatic, transcoelomic (implantation in body cavities), or anatomic continuity or implantation pathways. The latter refers to the spread and growth of cancer cells as a result of direct contact of tumor cells with adjacent tissues.2,5
Cutaneous metastases are usually associated with three mechanisms: hematogenous spread, lymphatic spread, or by contiguity or implantation. The macroscopic appearance of cutaneous metastases typically presents as solid lesions, nodular or papular in appearance, painless, and in some cases, associated with ulcers.5
Interestingly, in all reported cases in the international literature, the primary tumor was located in the left half of the colon, mainly in the sigmoid colon and the upper third of the rectum.5,6 It is also worth mentioning that they can often mimic cysts, lipomas, granulomas, or neurofibromas. Cutaneous metastases must be histologically distinguished from a primary cutaneous tumor. Making that distinction is not always easy, but there is a wide variety of immunohistochemical panels, antibodies, and genetic tests that can be useful.7 In our case, the glands were positive for the enterocyte immunohistochemical marker, cytokeratin 20, and the colorectal differentiation immunohistochemical marker, CDX-2.
Cases of metastatic carcinoma associated with anal fistula are rare.8 Most of these cases are related to gastrointestinal cancers, especially colorectal cancer. The implantation of cancer in an anal fistula occurs when cancer cells migrating from advanced colon cancer implant in an anal fistula.8,9 The pathogenesis of this type of distant metastasis remains unknown. The presence of a gap in the skin at the site of a fissure, fistula, or hemorrhoidectomy wound may explain how exfoliated tumor cells implant in those abnormal areas.9 Diagnosis is made when the implanted cells have the same histological type as the primary tumor.8,9
Treatment depends on several factors, including the extent of the disease, the location of the metastases, and the patient’s overall condition. Options may include systemic chemotherapy, radiotherapy, or surgery (with local resection),10 and when the finding is considered a sign of advanced disease, treatment is generally palliative. However, if the lesions are symptomatic, local excision or radiotherapy may be considered first-choice treatment. A report recently described the effectiveness of electrochemotherapy with bleomycin in the local control and symptomatic relief of cutaneous metastatic disease.6 Nevertheless, there is limited data on the effectiveness of different treatment modalities.
Finally, we must emphasize the fact that, in most cases, the appearance of cutaneous metastases from colorectal cancer represents a very advanced stage of the disease, and therefore treatment is usually only palliative.
Financial disclosureThe authors declare that they did not receive funding from any public or private institution for the preparation of this article.
Ethical considerationsThis case report did not include experiments on animals or humans, and the information comes solely from clinical observations made in routine professional practice, without altering the treatment of the subjects. The study complies with international ethical standards and respects the rights of individuals. We used patient data collection forms from our workplace, maintaining patient anonymity and providing informed consent.
The authors declare that there is no conflict of interest.