In healthy adults, mucosa-associated lymphoid tissue (MALT) accounts for 80% of all immune cells of the body. MALT has 3 functions: to protect mucous membranes against pathogens; to prevent the uptake of antigens in food, commensal microorganisms, and airborne matter; and to prevent a pathologic immune response to external antigens if they cross the mucosal barrier.1,2
MALT lymphoma is a marginal zone-type indolent B cell non-Hodgkin lymphoma (NHL) There are 3 main types of marginal zone lymphomas (MZLs): splenic MZL, extranodal MZL of MALT, and nodal MZL. MALT lymphoma belongs to the extranodal MZL group. Biopsies of MALT lymphoma show perivascular and parafollicular infiltration by atypical monocytoid lymphocytes with folded nuclear edges that are positive for CD19, CD20, and CD79a, but negative for CD5, mainly, as well as CD10.2
This disease is associated with White advanced-age (>60 years) populations and patients present with lymphocytosis, with or without cytopenia and splenomegaly. They usually present with lymphadenopathy and can have fever, night sweats, and weight loss greater than 10% of their previous total body weight (known as B symptoms).3
A 66-year-old woman sought medical attention, due to colicky pain that increased during food intake. She presented with intake intolerance of 6-month progression and immediate postprandial pain, with nausea and occasional vomiting. After vomiting she had pain that was accompanied by the sensation of a hard abdominal mass. She showed no signs of bowel obstruction. A relevant fact of her medical history was that she had a second-degree relative with Hodgkin’s lymphoma. Physical examination revealed a soft depressible abdomen, increased peristalsis upon superficial palpation, and increased volume in the left hypochondrium. The rest of the physical examination was normal.
The patient had previously undergone colonoscopy for gastrointestinal symptoms and was diagnosed with lymphocytic colitis. Laboratory test results reported carcinoembryonic antigen 1.45ng/mL and CA 19–9 2.5U/mL.
Preoperative complete blood count and blood chemistry analyses, as well as coagulation tests, were within normal limits, with adequate controls.
The following laboratory work-up results stood out: glucose 92mg/dl, blood urea nitrogen 7.9mg/dl, creatinine 0.5mg/dl, blood urea nitrogen/creatinine ratio 15.8, total cholesterol 136mg/dl, and triglycerides 67mg/dl.
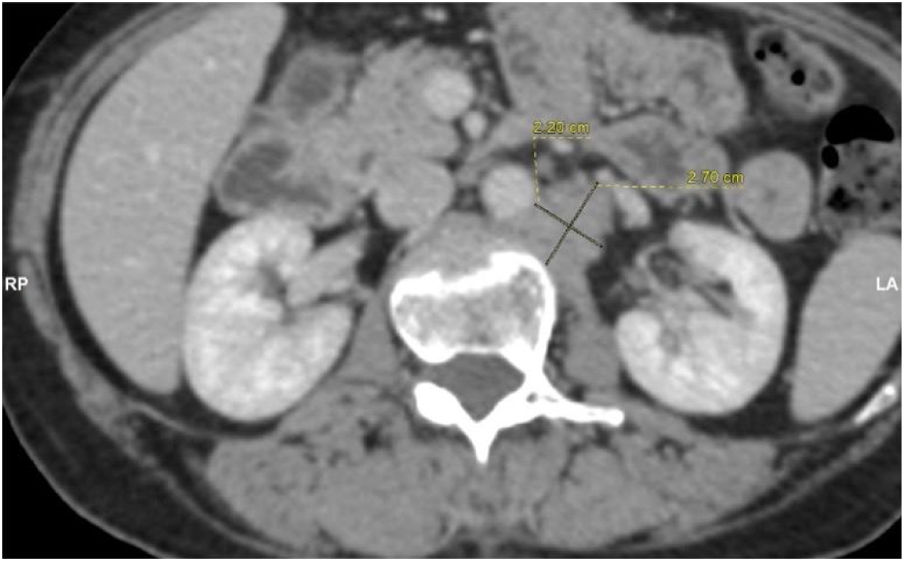
Contrast and non-contrast computed tomography (CT) of the abdomen and pelvis, with axial views and multiplanar reformation, were carried out (Fig. 1).
The CT scans identified small bowel segments distended with air and neutral fluid. There was homogeneously enhanced concentric wall thickening (with no stratification pattern) up to 21mm thick at the level of the distal ileum, which conditioned a narrowing of approximately 70% of the lumen, causing retrograde dilation of the ileum. Air and residual material were observed in the colon.
The thickening of the distal ileum walls ended with a retrograde obstructive defect and suspicious data of hepatic and para-aortic retroperitoneal lymph node metastatic activity, suggesting a carcinoid tumor. Exploratory laparotomy revealed a small bowel tumor at 210cm from the angle of Treitz and 160cm from the ileocecal valve that obstructed 80% of the intestinal lumen, causing wall thickening up to 10cm. Intestinal resection with a 10cm proximal and distal extension of healthy tissue was performed, along with an end-to-end intestinal anastomosis. Liver examination identified smooth edges and no superficial or deep tumors were palpated. Given the absence of bulges or macroscopic alterations, retroperitoneal exploration was not performed.
The diagnosis was extranodal marginal zone lymphoma, clinical stage II Be, low-risk MALT-IPI. The results of the complementary immunohistochemical tests were:
CD79: positive in 100% of the neoplastic cells; CD20: positive in 100% of the neoplastic cells (Fig. 2); CD43: positive in 80% of the neoplastic cells; CD5: positive in 20% of the neoplastic cells; CD10: negative; BCL-2: focally positive; Cyclin D1: negative; Kappa: negative; Lambda: negative; and CD23: negative.
The patient was released on hospitalization day 5, with adequate oral intake of food. At follow-up at the hematology service, 6 cycles of rituximab-bendamustine were started. She had complete response, with positron-emission tomography (PET) follow-up. Fifteen months after the surgery there were no signs of tumor activity.
MALT lymphoma is a non-Hodgkin extranodal marginal zone lymphoma that most commonly presents in the stomach, but other sites include the skin, salivary glands, lung, small bowel, thyroid, etc.2,3
Patients with gastric lymphoma typically present with nonspecific symptoms, frequently with the most common gastric conditions, such as peptic ulcer disease, gastric adenocarcinoma, and non-ulcerous dyspepsia.4
Like the rest of the lymphomas, diagnosis is based on lesion histology, complete blood count, and biochemical analyses. Endoscopic examination is necessary in cases of gastrointestinal or pulmonary lymphoma. Disease stage is determined through magnetic resonance imaging (MRI) and CT scanning. Bone marrow biopsy is also performed.5
The differential diagnosis includes B cell lymphoma, diffuse large B cell lymphoma, all types of non-Hodgkin lymphoma, and Helicobacter pylori infection.5
Ethical considerationsThe authors declare that this case report contains no personal information that could identify the patient, thus informed consent was not required, but nevertheless, it was obtained for the publication of this work. This case report meets the current bioethics research regulations. Given that the patient’s health was not compromised, authorization by the institution’s ethics committee was not required.
Financial disclosureNo specific grants were received from public sector agencies, the business sector, or non-profit organizations in relation to this article.
Author contributionsConcept, P.I.D.-H., C.A.C.-F., and J.G.L.-V.; Research, P.I.D.-H., C.A.C.-F., J.G.L.-V., U.V.-R., R.M.M.-L., and C.A.C.-F.; Writing/reparation of the original draft, P.I.D.-H., C.A.C.-F., J.G.L.-V., U.V.-R., R.M.M.-L., and C.A.C.-F.; Writing/review and editing, P.I.D.-H., C.A.C.-F., J.G.L.-V., U.V.-R., R.M.M.-L., and C.A.C.-F.; Supervision, C.A.C.-F.
All the authors have read and approved the present version of the manuscript to be published.
Conflict of interestThe authors declare that there is no conflict of interest.
Please cite this article as: Díaz-Hernández PI, Llanes-Villarreal JG, Valencia Rocha UR, Morales-López RM, Castro-Fuentes CA. Oclusión intestinal crónica secundaria a linfoma tipo MALT. Rev Gastroenterol Mex. 2023;88:448–450.