We have read with interest the work by Valdovinos-García et al.,1 which provides recommendations on the prescription and deprescription of proton pump inhibitors (PPIs). PPIs are widely prescribed medications in emergency services and intensive care units (ICUs), as a pharmacologic prophylaxis for ulcers due to stress and upper gastrointestinal bleeding (UGIB). Said prophylaxis has been reported to be employed in up to 84% of patients admitted to the ICU.2 However, only 2% of the patients develop clinically manifested bleeding and less than 0.1% end up presenting with clinically important bleeding,3 i.e., hemodynamic deterioration (a decrease in blood pressure of 20 mmHg or more, an increase in heart rate of 20 bpm, orthostatic hypotension, or a decrease in hemoglobin of 2 g/dl within 24 h from the bleeding).3 The pathophysiology of UGIB includes activation of the sympathetic nervous system, increased catecholamine release, vasoconstriction, hypovolemia, reduced cardiac output, and proinflammatory cytokine release.4 Stress-related responses damage the integrity of the gastric mucosa by reducing the gastrointestinal blood flow, oxygenation, and bicarbonate secretion.4 Mucosal barrier permeability is compromised and there is hydrogen ion and pepsin diffusion, damaging the epithelial mucosal layer even more.4 The slow flow of blood in the mucosa alters healing and the reduced gastric motility prolongs the time of contact of acid with the gastric mucosa.4 Another factor is damage due to reperfusion. When the blood flow is restored after long periods of hypoperfusion, elevated levels of nitric oxide synthase lead to hyperemia, cell death, and an increased inflammatory response,4 resulting in even more gastrointestinal epithelial damage and ulceration.4 Stress-related mucosal lesions are predominantly located in the acid-producing zones of the upper portion of the gastric fundus and body.4
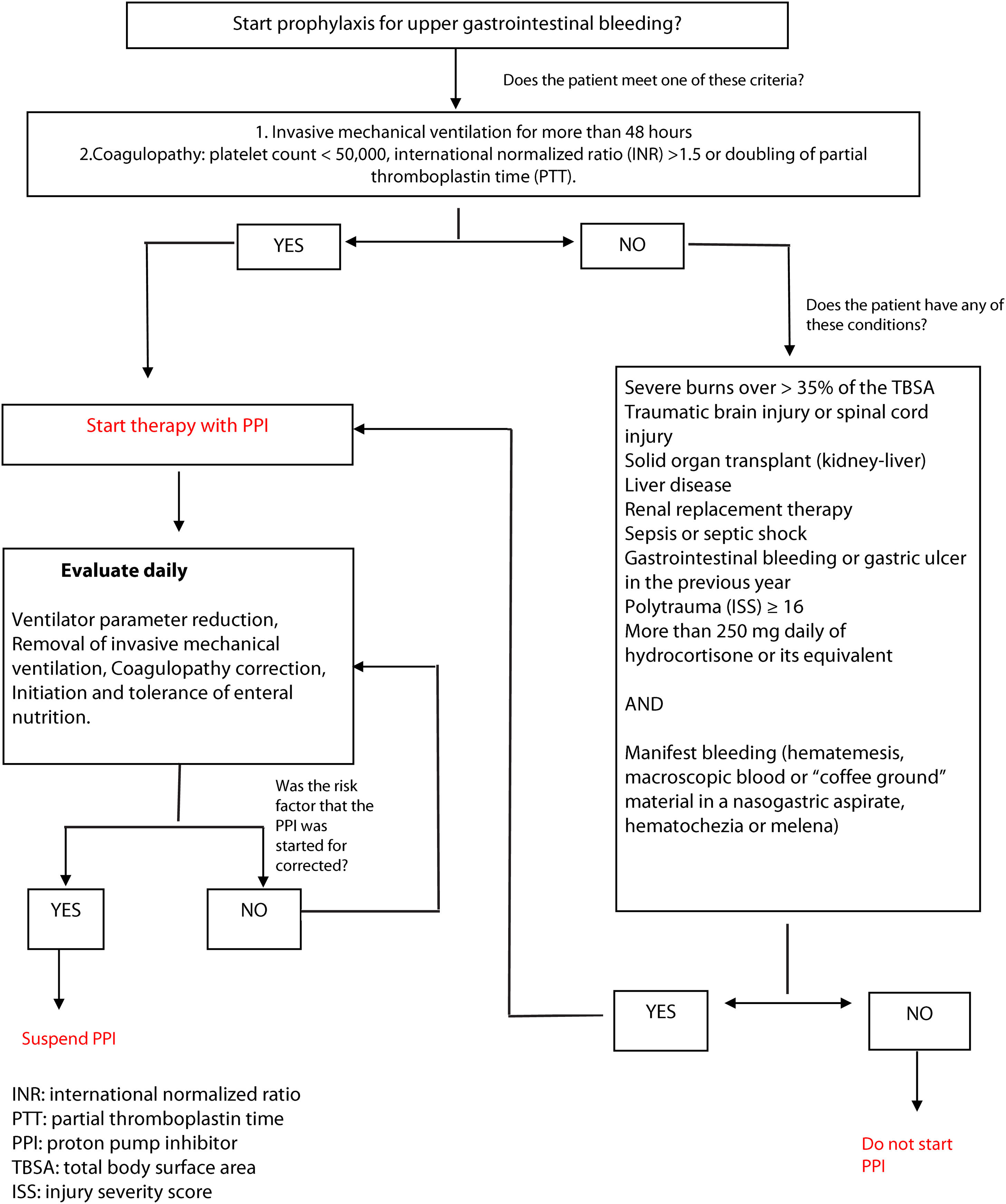
The most important risk factors for UGIB are respiratory insufficiency requiring mechanical ventilation for more than 48 h and acute coagulopathy (platelet count < 50,000, international normalized ratio [INR] > 1.5, or doubled partial thromboplastin time [PTT]).4 Other possible bleeding conditioning factors are severe burns, traumatic brain injury, history of solid organ transplantation, liver disease, implementation of renal replacement therapy, and a high sequential organ failure assessment (SOFA) score in the context of sepsis or septic shock, neurologic lesion, previous gastrointestinal bleeding, polytrauma with an injury severity score (ISS) above 16, spinal cord trauma, and the permanent use of 200 mg of hydrocortisone equivalents per day.4 Thus, we consider there should be therapeutic algorithms (Fig. 1) for selecting patients that would benefit from starting a PPI and preventing its inadequate use and consequent risks and costs.
Financial disclosureNo financial support was received in relation to this article.
The authors declare that there is no conflict of interest.