Right-sided colon cancer (RSCC) is characterized by distinct clinical features and recurrence patterns. Our study aimed to develop a predictive model for distant recurrence in patients with RSCC who underwent curative surgery, employing the Random Forest machine learning algorithm, based on clinical and histopathologic variables.
Materials and methodsA retrospective analysis of 64 patients treated within the time frame of 2016–2024 was conducted. The variables included age, sex, lymphovascular invasion, and number of lymph nodes evaluated (transformed for inverse interpretation). Oversampling was employed to balance the dataset and a Random Forest model for predicting distant recurrence (defined as that occurring at least six months after surgery) was constructed. Its performance was evaluated through accuracy, sensitivity, F1 score, and area under the ROC curve (AUC).
ResultsThe model achieved an AUC of 0.76 in the test set, with 75% sensitivity and 100% specificity. The most relevant variables were low lymph node harvest, older age, male sex, and lymphovascular invasion. A simplified model with those four variables maintained 95% accuracy. A clinical risk scale based on cumulative scores was developed that classified patients into low-risk and high-risk groups, with distant recurrence rates of 8.3% and 56.3%, respectively.
ConclusionThe predictive model showed a robust capacity for stratifying the distant recurrence risk, supporting the use of machine learning algorithms as a complementary tool in the individualized management of RSCC.
El cáncer de colon derecho (CCD) se distingue por sus características clínicas y patrones de recurrencia únicos. Este estudio tuvo como objetivo desarrollar un modelo predictivo de recurrencia a distancia en pacientes con CCD operados con intención curativa, empleando el algoritmo de aprendizaje automático random forest a partir de variables clínicas e histopatológicas.
Materiales y métodosSe realizó un análisis retrospectivo de 64 pacientes tratados entre 2016–2024. Se incluyeron variables como edad, sexo, invasión linfo-vascular y número de ganglios linfáticos evaluados (transformado para interpretación inversa). Se empleó sobremuestreo para balancear los datos y se construyó un modelo random forest para predecir recurrencia a distancia (definida como aquella documentada a partir de los seis meses posteriores a la cirugía). Se evaluó su desempeño mediante precisión, sensibilidad, puntuación F1 y área bajo la curva ROC (AUC).
ResultadosEl modelo obtuvo un AUC de 0.76 en el conjunto de prueba, con sensibilidad del 75 % y especificidad del 100 %. Las variables más relevantes fueron: menor cosecha ganglionar, edad avanzada, sexo masculino e invasión linfática/vascular. Un modelo simplificado con estas cuatro variables mantuvo una precisión del 95 %. Se construyó una escala clínica de puntajes acumulativos que clasificó a los pacientes en grupos de bajo y alto riesgo, con tasas de recurrencia a distancia de 8.3 % y 56.3 %, respectivamente.
ConclusiónEl modelo predictivo mostró una capacidad robusta para estratificar el riesgo de recurrencia a distancia, respaldando el uso de algoritmos de aprendizaje automático como herramienta complementaria en el manejo individualizado del CCD.
Colorectal cancer (CRC) is one of the main causes of morbidity and mortality worldwide. It is also the third most frequent type of cancer and the second cause of cancer death. Within CRC, right-sided colon cancer (RSCC) is characterized by particular clinical, molecular, and prognostic features, in relation to left-sided colon cancer, including more aggressive behavior and a greater propensity for systemic recurrence.1,2 The RSCC recurrence rates, local or distant, vary from 10 to 30%, according to different international case series, conditioned by pathologic stage, surgical resection quality, and the presence of adverse histologic factors.3
Early identification of patients at high risk for distant recurrence is essential for guiding postoperative follow-up strategies, individualizing the indication of adjuvant treatments, and improving long-term oncologic outcomes, making the development of reliable predictive tools a clinical priority.
Recent advances in machine learning techniques have enabled predictive models to be constructed that are more accurate than conventional statistics methods, by simultaneously integrating multiple clinical, pathologic, and even molecular, variables.4,5 Algorithms, like Random Forest (RF), have demonstrated a high level of efficacy for classifying and predicting clinical events in oncology, standing out for their resistance to overfitting, robustness when facing imbalanced datasets, and capacity to capture nonlinear relationships between predictors.6,7 In addition, they have the added value of identifying variables that are accessible from clinical practice as indirect substitutes of tumor aggressiveness or biologic disease burden, even in the absence of complete TNM staging.
In this context, it is clinically relevant to explore whether routinely obtained variables, such as age, sex, number of lymph nodes evaluated, and lymphovascular invasion, may be integrated into predictive models for anticipating distant recurrence in patients with RSCC.8,9 Incorporating such models, sustained by machine learning, could provide an additional tool for stratifying individual risk, guiding a more accurate and efficient personalized approach in medicine. Thus, our study aimed to develop and internally validate a distant recurrence prediction model in RSCC, utilizing the RF algorithm, based on clinical and histopathologic variables collected at a specialized center.
Materials and methodsA retrospective, observational, single center study was conducted, with the aim of identifying factors associated with RSCC recurrence and constructing a machine learning predictive model. The study included 64 patients with a confirmed diagnosis of RSCC, within the time frame of 2016 to 2024 and was conducted according to the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guideline, to ensure methodological transparency and internal validity.
All the patients underwent curative surgery at the same center, following homogeneous surgical treatment and oncologic surveillance criteria. Patients that underwent palliative surgery, presented with metastatic disease at diagnosis or residual disease, or whose clinicopathologic information was incomplete, were excluded from the study. Tumors were exclusively located in the right colon (cecum, ascending colon, or hepatic angle), enabling the formation of a clinically homogeneous cohort.
The following clinicopathologic variables were initially included: age (years), sex (male/female), lymphatic vessel invasion, vascular invasion, perineural invasion, histologic grade, surgical margin status, total number of lymph nodes evaluated, and TNM staging that was retrospectively reconstructed into the T, N, and M components. Those variables were selected for their clinical and epidemiologic relevance, previously reported in relation to tumor recurrence.
Only patients with a minimum of 24 months of clinical follow-up or with distant recurrence documented before that threshold were considered. Recurrence was operatively defined as the detection of distant disease equal to or greater than 6 months prior to surgery, confirmed through imaging studies. That temporal threshold was adopted to prevent the inclusion of residual disease, following criteria in the current medical literature. Recurrences identified before 6 months were classified as residual disease, and as such, excluded from the study.
Predictive model developmentThe RF classification algorithm was utilized to construct the prediction model, selected for its capacity to manage nonlinear relationships between variables, its low risk for overfitting, compared with other methods, and its robustness when dealing with datasets exhibiting class imbalance.
Prior to training, the data were standardized to ensure homogeneous behavior between predictors. Because the cases with recurrence were the minority, upsampling of said class was applied to balance the training dataset. A randomized stratification partition of the balanced set was then carried out, assigning 70% of the cases to the training group and 30% to the test group. A fixed random seed was employed to ensure reproducibility.
To avoid overfitting associated with the use of multiple variables in a limited cohort, stratified (5-fold) cross-validation was employed and a simplified clinical model was constructed with only four predictors: age, sex, lymphovascular invasion, and total number of lymph nodes evaluated. This last variable was treated as an inverse risk factor, meaning that a lower lymph node harvest was interpreted as a higher risk for recurrence.
Clinical TNM staging, based on the T, N, and M components, was retrospectively reconstructed. This classification was included in the initial analyses of the model. However, it showed very limited predictive capacity (AUC = 0.438, sensitivity = 0 %), and so was excluded from the final model. Cross-validation confirmed its low performance, compared with the proposed clinical model.
To minimize the overfitting risk inherent in the use of numerous predictors in small sample sizes, several specific measures were implemented: the pre-selection of relevant clinical variables, construction of a simplified model with only 4 predictors, use of stratified (5-fold) cross-validation, and use of a learning curve analysis. Those strategies enabled the stability and reproducibility of the model to be maintained, reducing the possibility of training data overfitting.
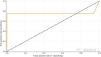
Model evaluation and clinical scale constructionThe model was evaluated through standard classification metrics: overall accuracy, sensitivity, specificity, F1 score, and area under the ROC curve (AUC). The confounder matrix was utilized to identify systematic errors and confirm the model’s stability. The learning curve demonstrated convergence after 30 cases, with a low difference between training error and validation, suggesting a low probability of overfitting.
Based on the relative importance of the variables, a clinical risk scale determined through cumulative scores was designed. Cutoff points were established for stratifying the patients into two risk groups:
- •
Low risk: 0–10 points
- •
High risk: 11–20 points
The recurrence rates observed were 8.3% in the low-risk group and 56.3% in the high-risk group, showing clear prognostic differentiation. This classification enabled the model’s results to be translated into a simple and reproducible clinical tool.
Statistical analysisThe continuous variables were expressed as means ± standard deviation or as medians (IQR), according to the distribution evaluated by the Shapiro-Wilk test. The categorical variables were presented as absolute frequencies and percentages. For group comparisons (recurrence versus no recurrence), the Student’s t-test and Mann-Whitney U test were employed (according to normality), and the chi-square test and Fisher’s exact-test, for the categorical variables. Statistical significance was set at a p < 0.05.
The importance of each variable in the model was estimated through the Gini importance index. The performance of the clinical model was compared with that of models incorporating the TNM classification, showing no significant improvement.
All the analyses were carried out in the Python 3.11.5 environment, utilizing the pandas, numpy, scikit-learn, matplotlib, and seaborn libraries.
ResultsSixty-four patients with a confirmed diagnosis of RSCC who underwent curative surgery were included in the study. All had a minimum of 24 months of oncologic follow-up or presented with documented recurrence within that period of time. The primary outcome measure was distant recurrence, defined as that confirmed through imaging studies, occurring from 6 months after surgery.
The predictive model developed through the RF algorithm achieved overall accuracy of 95% in the test set. The ROC curve had an AUC of 0.76, indicating acceptable discriminative capacity for identifying patients at high risk of distant recurrence (Fig. 1). In clinical terms, that implied a 76% probability that the model correctly classified a patient with recurrence versus a patient with no recurrence.
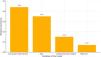
The importance analysis of the variables revealed that the most influential predictor was a low lymph node harvest (the inverse value of the number of lymph nodes evaluated), with a relative importance of 0.44, followed by age (0.35), lymphovascular invasion (0.15), and male sex (0.07) (Figs. 2 and 3). That analysis reinforced the clinical interpretation that a lower number of lymph nodes evaluated was associated with a higher risk of tumor recurrence.
Importance of the variables in the Random Forest model.
The horizontal bar represents the relative importance of each variable in predicting distant recurrence. The “low lymph node harvest” (inverse of the number of lymph nodes collected) was the most influential predictor, followed by age, lymphovascular invasion, and male sex.
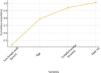
Cumulative importance of the variables in the Random Forest model.
Proportional distribution of the contribution of each variable to the overall performance of the model. “Low lymph node harvest” provided 44% of the total predictive capacity, whereas age, lymphovascular invasion, and male sex represented the rest of the explained variance.
To optimize the model’s applicability, a simplified version was constructed, based exclusively on those four variables. This model reduced complexity without sacrificing accuracy, reaching 95% accuracy, 75% sensitivity, 100% specificity, and an F1 score of 0.86. Stratified (5-fold) cross-validation showed a mean AUC of 0.81, with a low standard deviation, indicating consistent performance across numerous data subsets (Fig. 4), with a final AUC of 0.76 in the test set and a mean AUC of 0.81 in the cross-validation.
Cross-validation results of the simplified Random Forest model.
Accuracy achieved by each of the 5 stratified cross-validation folds. The model showed a mean accuracy of 95%, with a mean AUC of 0.81 and stability between iterations, supporting its reproducibility and robustness, despite the limited sample size.
In contrast, a model exclusively constructed with TNM staging as the only variable obtained an AUC of 0.438, 0% sensitivity, and an F1 score of 0.0, reflecting null predictive value. Even when integrating the TNM classification with other clinical variables, the model only reached an AUC of 0.77 and 25% sensitivity. Those results are in contrast with the performance of the simplified clinical model, which significantly surpassed conventional anatomic staging in all the metrics evaluated.
Clinical recurrence prediction scaleFrom the simplified model, a clinical scale, based on a cumulative scoring system proportional to the relative importance of each variable in the RF model, was designed. That system enabled the classification of patients into two clinically differentiated risk levels (Tables 1 and 2):
- •
Low risk (0−10 points): observed recurrence rate of 8.3% (4/48)
- •
High risk (11−20 points): observed recurrence rate of 56.3 % (9/16)
Scoring system based on clinical and pathologic characteristics.
| Variable | Criterion | Score |
|---|---|---|
| Lymph nodes evaluated | ≥15 lymph nodes evaluated | 1 |
| 10−14 lymph nodes evaluated | 4 | |
| 5−9 lymph nodes evaluated | 7 | |
| <5 lymph nodes evaluated | 10 | |
| Age | ≥70 years | 1 |
| 60−69 years | 2 | |
| 50−59 years | 3 | |
| <50 years | 4 | |
| Lymphovascular invasion | Present | 4 |
| Absent | 0 | |
| Sex | Male | 2 |
| Female | 0 |
The total score was obtained by adding together the scores of each variable.
Risk recurrence classification.
| Total score | Risk category | Patients (n) | Recurrences | Recurrence rate |
|---|---|---|---|---|
| 0−10 | Low risk | 48 | 4 | 8.3% |
| 11−20 | High risk | 16 | 9 | 56.3% |
Recurrence risk classification according to the total score. The patients were classified into 2 risk levels: low (0–10 points and high (11–20 points), according to the cumulative score derived from the clinical and pathologic factors.
That binary stratification displayed a robust and clinically relevant discriminative capacity. The progression of the recurrence rates observed validates the potential use of this scale as a practical tool for personalizing postoperative follow-up and intensifying surveillance in high-risk patients or considering additional therapeutic strategies.
DiscussionThe aim of the present study was to develop a predictive clinical model, utilizing machine learning, to anticipate distant recurrence in RSCC. Our results show that the model based on the RF algorithm offers a robust performance for predicting distant recurrence in patients with RSCC. The simplified model, composed of routine clinicopathologic variables, achieved 95% general accuracy, 75% sensitivity, 100% specificity, and an AUC of 0.76. Those results reflect adequate and clinically useful discriminative capacity, especially when considering sample size and the absence of complete TNM staging.
The most relevant variables identified by the model were: low lymph node harvest, advanced age, lymphovascular invasion, and male sex. Unlike that suggested by traditional models centered on lymph node positivity, our analysis identified the absolute number of lymph nodes evaluated as the most influential predictor. Said variable could reflect, not only the technical quality of the surgery or tumor aggressiveness, but also immunologic or anatomic aspects that condition lymph node harvesting, and subsequently, patient prognosis.
Previous studies on machine learning have reported performances superior to those of TNM. For example, Liu et al. achieved an AUC of 0.962, utilizing XGBoost for predicting recurrence in CRC.1 In our study, the RF algorithm produced consistent results, with less computational complexity and greater clinical interpretability. The AUC was lower, but that could be attributed to sample size and the strict selection of variables that are easily available in clinical practice.
Regarding applicability, a clinical scale derived from the simplified model was constructed. This enabled the stratification of the patients into 2 clinically distinguishable risk groups: low risk (0−10 points, 8.3% recurrence) and high-risk (11−20 points, 56.3% recurrence). The magnitude of the difference observed between the groups supports the validity of the model and its potential usefulness as a support tool for making individualized oncologic decisions, including intensifying follow-up or considering adjuvant therapeutic strategies.
In contrast, the model based solely on the TNM classification displayed limited performance in our analysis (AUC = 0.438; sensitivity = 0 %; F1 score = 0.0). Even when combined with clinical variables, its predictive capacity continued to be inferior (AUC = 0.77; sensitivity = 25%). Those findings are in line with current evidence supporting the fact that even though the TNM classification is the international standard for the staging and prognosis of colon cancer, it has important limitations in individual outcome predictions, particularly those of recurrence and survival. Different studies have shown that the TNM predictive performance is modest, when used on its own. For example, the AUC for models based exclusively on TNM tends to vary from 0.60 to 0.64, indicating limited discriminative capacity for predicting recurrence or mortality, at the individual level.10–12 In addition, its sensitivity for predicting recurrence is suboptimal and the values reported in the literature rarely surpass 60%.13
The incorporation of additional clinical variables (such as age, sex, tumor grade, number of lymph nodes examined, vascular/perineural invasion, and molecular markers, such as MSI, BRAF, and KRAS) has been shown to significantly improve the predictive capacity of the models. By integrating said variables, the AUC may increase up to 0.71−0.74, with consistently improved agreement in the models.10,11,13 Nevertheless, even those traditional multivariable models show limitations regarding individual prediction.
In recent years, models based on artificial intelligence and machine learning have been shown to significantly surpass the TNM system, as well as conventional clinical models. Large volumes of clinical, pathologic, molecular, and even histopathologic image data can be integrated using those strategies, achieving superior AUCs (e.g., between 0.77 and 0.86) and improving sensitivity and accuracy in predicting oncologic outcomes.14,15 In addition, the relative importance of traditional clinical staging tends to decrease when additional variables and advanced modeling techniques are employed.14,15
Methodologically, robust strategies were applied to mitigate the risk of overfitting, including the pre-selection of clinically relevant variables, class balancing through oversampling, 5-fold cross-validation, and designing a simplified model with clinical interpretability. The model’s stability was confirmed by a mean AUC of 0.81 in the cross-validation.
Finally, recurrence was defined as new disease detected ≥ 6 months after surgery, in concordance with recent studies that recommend said threshold for differentiating true recurrence from residual disease.16 That definition strengthens the validity of our results, enabling comparability with the international literature.
ConclusionThe predictive model developed through the RF algorithm displayed solid performance for anticipating distant recurrence in patients with RSCC, with an AUC of 0.76, 75% sensitivity, and 100% specificity. The most relevant variables were low lymph node harvest, age, lymphovascular invasion, and male sex.
From those findings, a simplified clinical scale was constructed that stratified the risk of recurrence into two levels:
- •
Low risk (0−10 points): observed recurrence of 8.3%
- •
High risk (11−20 points): observed recurrence of 56.3%
Our study results support the potential use of machine learning models as accessible clinical tools for the individual stratification of oncologic risk, surpassing the traditional TNM staging. The model was validated internally through stratified cross-validation, but we recognize that its usefulness must be externally corroborated.
LimitationsThe present study should be interpreted as an exploratory and hypothesis-generating pilot analysis. Even though the model showed robust performance in the cross-validation, its findings must be replicated and externally validated in larger cohorts, before being considered applicable in clinical practice.
Limitations include those inherent in the study’s retrospective design and small sample size (n = 64), which restrict its statistical power, the capacity to detect higher-order interactions, and the external generalization of the model. Even though machine learning algorithms, such as RF, enable training with small samples, there is a latent risk of overfitting, despite the measures adopted to prevent it (class balancing, cross-validation, model simplification).
Because the study was carried out at a single center, the patients included may not completely represent the variability seen at other institutions or in other regions. Even though the variables employed are standard clinical variables, we recognize that demographic characteristics or local institutional practices could influence results. Therefore, external validation in more diverse cohorts is essential, before considering the model’s generalized application.
Likewise, the use of variables derived from clinical records limits control over data collection homogeneity and the retrospective reconstruction of the TNM staging may introduce classification biases.
Therefore, the results presented herein must be considered exploratory and their clinical application externally validated in prospective multicenter studies with larger samples and greater clinical diversity. Only then, will it be possible to confirm the predictive value of the scale and its potential impact on improving the individualized management of RSCC.
Ethical considerationsGiven the study’s retrospective and observational design, based on anonymized clinical records, individual informed consent was not required. Confidentiality was guaranteed at all times. The ethical principles of the Declaration of Helsinki were met, together with the current national health research regulations. The protocol met the criteria established by the COFEPRIS and the General Health Law regulations on scientific research.
Financial disclosureNo specific grants were received from public sector agencies, the business sector, or non-profit organizations in relation to this study.
The authors declare that there is no conflict of interest.