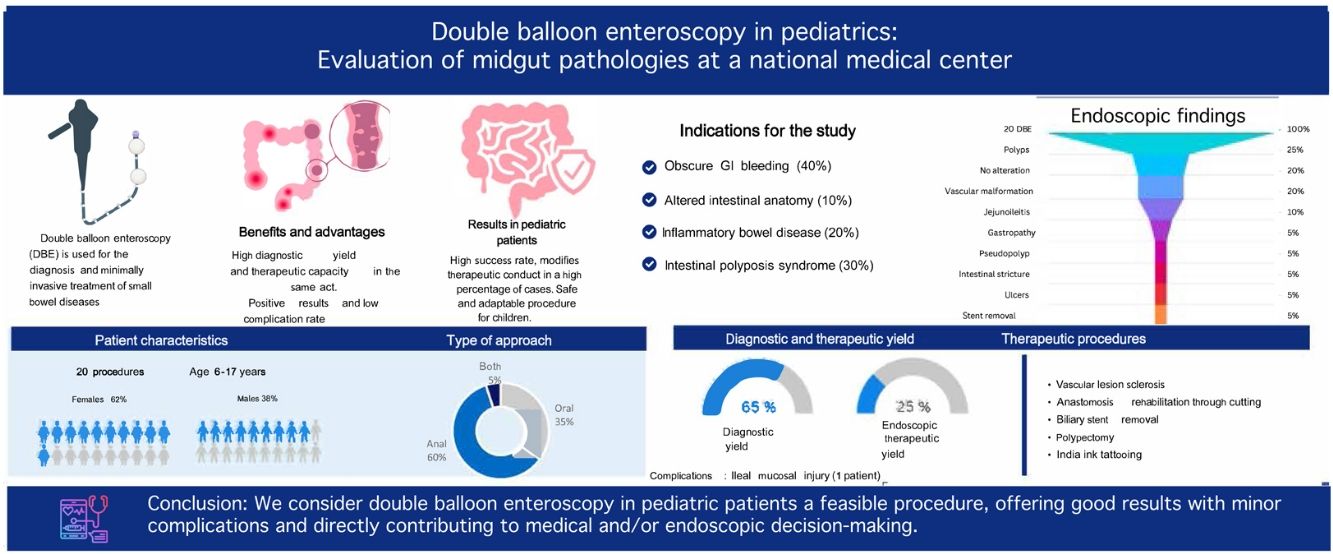
Double balloon enteroscopy is used for the diagnosis and treatment of diseases of the small bowel. It is a less invasive means for carrying out a therapeutic intervention, compared with surgical alternatives. Experience with double balloon enteroscopy in pediatrics is in the early stages of development. We believe the performance of this procedure in children has a significant clinical impact on therapeutic decision-making in diseases of the small bowel. Our aim was to evaluate double balloon enteroscopy in children for the diagnosis and treatment of midgut pathologies.
Material and methodsA retrospective, descriptive, and observational study was conducted.
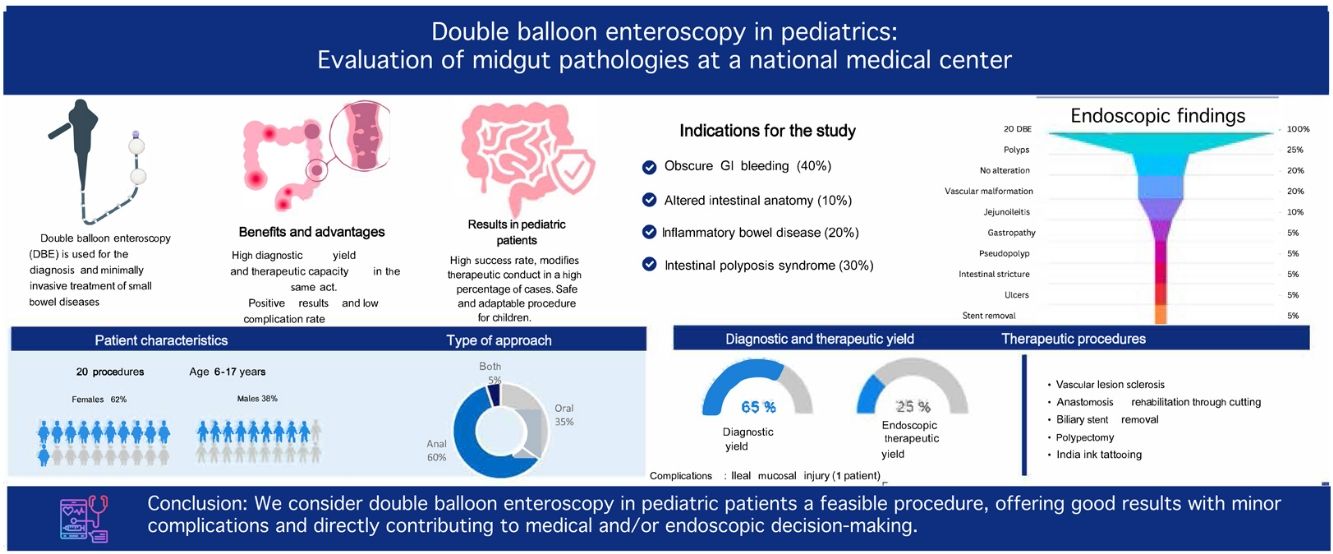
ResultsTwenty procedures were performed on patients whose ages ranged from 6 to 17 years, with a mean of 13.3 years. The most frequent indication for doble balloon enteroscopy was gastrointestinal bleeding suspected to originate from the small bowel.
Double balloon enteroscopy resulted in an overall diagnostic yield of 65% and an endoscopic therapeutic yield of 25%. Endoscopic therapy was performed in 4 patients (anastomosis rehabilitation through cutting, sclerosis of vascular lesion with 1.5% polidocanol, polypectomy, biliary stent removal). No patient underwent surgical treatment after double balloon enteroscopy. Therapeutic yield, in general, including endoscopic and medical treatment, was 55%.
ConclusionsWe consider double balloon enteroscopy in pediatric patients a feasible procedure, offering good results with minor complications and directly contributing to medical and/or endoscopic decision-making.
La enteroscopia de doble balón se utiliza para el diagnóstico y tratamiento de las enfermedades del intestino delgado, proporciona un medio menos invasivo para lograr una intervención terapéutica en comparación con las alternativas quirúrgicas. La experiencia con la enteroscopia de doble balón en la edad pediátrica se encuentra en las primeras etapas de desarrollo, consideramos que la realización de este procedimiento en niños tiene un impacto clínico significativo para la toma decisiones terapéuticas en enfermedades del intestino delgado.
ObjetivoEvaluar la enteroscopia con doble balón en niños para el diagnóstico y tratamiento de patologías de intestino medio.
Material y métodosEstudio retrospectivo, descriptivo y observacional.
ResultadosSe realizaron un total de 20 procedimientos, el rango de edad de nuestros pacientes fue de 6 años a 17 años, con una media de 13.3 años. La indicación más frecuente para al EDB fue el sangrado gastrointestinal como sospecha de hemorragia digestiva media.
El rendimiento diagnostico global fue del 65%, el rendimiento terapéutico endoscópico con EDB fue del 25%; se realizó terapia endoscópica en 4 pacientes (rehabilitación de anastomosis mediante corte, esclerosis de lesión vascular con polidocanol 1.5%, polipectomía, retiro de stent biliar). Ningún paciente fue sometido a tratamiento quirúrgico después de los procedimientos de enteroscopia de doble balón. El rendimiento terapéutico en general, incluyendo el tratamiento endoscópico y médico fue del 55%.
ConclusionesConsideramos que la enteroscopia con doble balón en pacientes pediátricos es factible, obteniendo buenos resultados con complicaciones menores y contribuye directamente en la toma de decisiones terapéuticas médicas y/o endoscópicas.
Double balloon enteroscopy (DBE) is utilized for the diagnosis and treatment of diseases of the small bowel. Bleeding, polyps, and tumors are the small bowel lesions that can be visualized through the procedure. Therapeutic interventions, such as electrocoagulation, polypectomy, and stent placement, can also be performed using this endoscopic method.1 In 2007, Leung conducted the first case series on DBE in pediatric patients, after which the procedure was performed on other pediatric populations. In 2016, Yokoyama et al. reported DBE as a safe procedure in Japanese pediatric patients.2
The performance of DBE in the pediatric population is limited due to the size of the external diameters of the endoscope and overtube. Patient age and size may be limiting factors for the use of DBE, given the smaller abdominal cavity, thinner intestinal walls, and a narrower intestinal lumen. DBE is technically more complex in pediatric patients than in adults and may require a greater level of skill for its successful performance.3 Adequate patient selection, which signifies detailed information, such as age, concomitant diseases, and blood type, as well as the correct choice of the enteroscopy device to be used, are essential for successful treatment of midgut bleeding.
Small bowel bleeding, which is generally not visualized in upper or lower gastrointestinal endoscopy, through gastroscope or colonoscope, is always a diagnostic challenge. Seventy-nine percent of patients with small bowel bleeding have been shown to usually require four procedures for the diagnostic location of the bleeding origin. Obscure gastrointestinal bleeding is the most common indication for DBE. The combined detection rate was reported at 68.1%.4 Obscure gastrointestinal bleeding is defined as persistent or recurrent gastrointestinal bleeding of no obvious cause after primary endoscopy (upper endoscopy or colonoscopy) and imaging studies.
In patients with chronic small bowel bleeding, the most common bleeding sources are angiodysplasias or vascular malformations. Thus, argon plasma coagulopathy (APC) is one of the most widely utilized therapeutic methods. Any type of erosion or ulceration caused by inflammatory bowel disease, polyps, or Meckel’s diverticulum are other possible sources of bleeding. Enteroscopy has also become important in patients with intestinal polyposis syndromes because it provides the option of endoscopic resection in deeper parts of the small bowel, without the need for surgery.5 In cases of familial adenomatous polyposis and Peutz-Jeghers syndrome, DBE is useful for disease detection and as a therapeutic intervention in patients with bleeding or partial obstruction. Polyps larger than 15 mm have a tendency toward intussusception and their removal is recommended. In cases of modified intestinal anatomy secondary to biliary diversions, such as a Roux-en-Y, DBE enables endoscopic retrograde cholangiopancreatography to be performed, providing both a diagnostic and therapeutic approach, such as stone extraction, dilatation, or biliary stent placement.6
Complications of double balloon enteroscopyAccording to the literature, the complication rate of diagnostic DBE is 1% and is from 3 to 4% for therapeutic DBE. Polypectomy for large polyps appears to be the intervention associated with a higher complication rate, reaching 10%. The mortality rate is estimated at 0.05%.5
Given the evidence provided and the importance of DBE for the minimally invasive detection and treatment of small bowel diseases, we consider it important to evaluate the safety and benefits of the procedure in children suspected of presenting with a disease of the small bowel, documenting the diagnostic and therapeutic yield, to know its contribution to therapeutic decision-making, in other words, its clinical impact.
Material and methodsA retrospective, observational, descriptive study was conducted utilizing the medical records of pediatric patients that underwent DBE due to suspected disease of the small bowel, seen at the Centro Médico Nacional “20 de Noviembre” ISSSTE, a tertiary care hospital, within the time frame of March 2013 and January 2024. The STROBE checklist for cross-sectional studies was employed.
The DBE system utilized (FUJI EN-530T) was 2,000 mm in length, with an external diameter of 9.4 mm and a working channel diameter of 3.2 mm, enabling its use for a variety of therapeutic goals. The overtube measured 140 cm in length with an external diameter of 13.2 mm. Balloon air pressure was 45 mmHg, which is the lowest pressure required for holding the intestine for endoscope insertion.
The choice of an oral (anterograde) versus anal (retrograde) approach depended on the suspected location of the disease and all procedures were performed under general anesthesia.
All clinical records were included that contained the following characteristics: patients suspected of having a small bowel disease, either sex, the procedure performed within the time frame of March 2013 and January 2024, patients treated at the pediatric endoscopy service of the Centro Médico Nacional “20 de Noviembre”, ISSSTE, patient files that contained a report of the DBE procedure, type of approach (anterograde or retrograde), and patients that underwent a retrograde DBE that had bowel preparation with polyethylene glycol.
Patients whose clinical records documented non-oral or non-anal enteroscopy (stoma), incomplete enteroscopy due to poor bowel preparation, and patients whose clinical records were poorly prepared were excluded from the study.
Statistical analysisNon-probabilistic convenience sampling for cross-sectional studies was utilized, considering a z alpha of 1.96, 40% prevalence, 92% accuracy, and adding 20% for possible clinical records not found in the sample, resulting in a total of 62 patients. Twenty-two clinical records were of patients that underwent DBE due to suspected small bowel disease. Our aim was to know the frequency and behavior of the characteristics of our sample population.
The data collection sheet contained the following variables: the most frequent indications for DBE, findings, complications, therapy employed, and diagnostic and therapeutic yield, for reporting the patient characteristics throughout the clinical course. Tables and graphs were made for the data analysis and results, to analyze the clinical impact of DBE in pediatric patients. The data were analyzed using IBM® SPSS Statistics 29 software.
Ethical considerationsInformed consent on the part of the children’s parents or guardians for the performance of double balloon enteroscopy was included in the clinical records analyzed.
Informed consent was not requested for the publication of this study given that it contains no personal data that could identify patients.
The protocol of the present study was first reviewed and authorized by the Biosafety in Research committee of the Centro Médico Nacional “20 de Noviembre”, ISSSTE. Data confidentiality and patient privacy were both fully guaranteed.
ResultsDBE was performed on 22 patients with small bowel disease, within the study period of March 2013 to January 2024. The electronic medical record database of the Centro Médico Nacional “20 de Noviembre”, ISSSTE, was consulted, finding 22 clinical records of patients suspected of having diseases of the small bowel. Two of those records were poorly prepared and so were eliminated, resulting in 20 clinical records as the study universe. All patients underwent outpatient procedures.
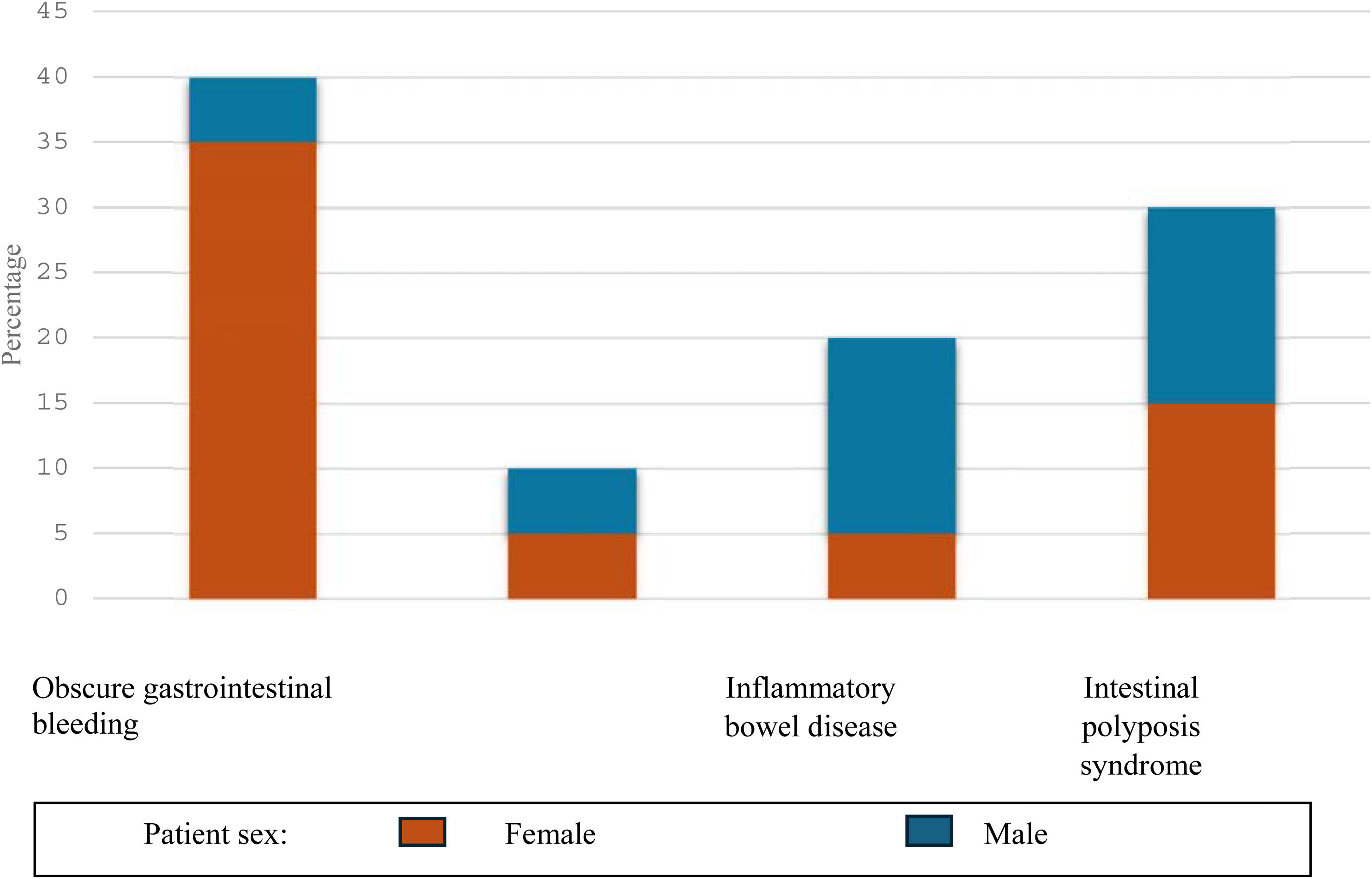
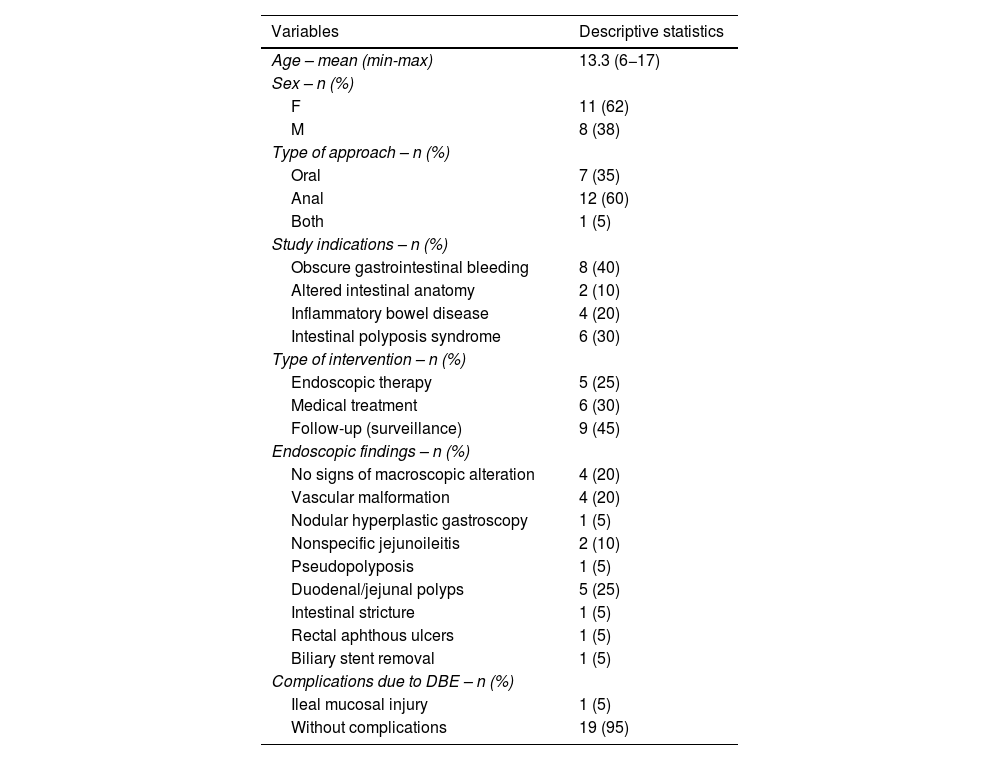
Patient characteristicsA total of 20 procedures were performed on 19 patients (11 females and eight males). The age range was from six to 17 years, with a mean age of 13.3 years, a mode of 12 years, and a median of 14 years (Table 1).
General sample characteristics.
| Variables | Descriptive statistics |
|---|---|
| Age – mean (min-max) | 13.3 (6−17) |
| Sex – n (%) | |
| F | 11 (62) |
| M | 8 (38) |
| Type of approach – n (%) | |
| Oral | 7 (35) |
| Anal | 12 (60) |
| Both | 1 (5) |
| Study indications – n (%) | |
| Obscure gastrointestinal bleeding | 8 (40) |
| Altered intestinal anatomy | 2 (10) |
| Inflammatory bowel disease | 4 (20) |
| Intestinal polyposis syndrome | 6 (30) |
| Type of intervention – n (%) | |
| Endoscopic therapy | 5 (25) |
| Medical treatment | 6 (30) |
| Follow-up (surveillance) | 9 (45) |
| Endoscopic findings – n (%) | |
| No signs of macroscopic alteration | 4 (20) |
| Vascular malformation | 4 (20) |
| Nodular hyperplastic gastroscopy | 1 (5) |
| Nonspecific jejunoileitis | 2 (10) |
| Pseudopolyposis | 1 (5) |
| Duodenal/jejunal polyps | 5 (25) |
| Intestinal stricture | 1 (5) |
| Rectal aphthous ulcers | 1 (5) |
| Biliary stent removal | 1 (5) |
| Complications due to DBE – n (%) | |
| Ileal mucosal injury | 1 (5) |
| Without complications | 19 (95) |
max: maximum; min: minimum.
The study population was predominantly female. Gastrointestinal bleeding of obscure origin with no alterations in endoscopy was the most frequent disease in females, with five cases. In males, the most frequent disease was intestinal polyposis syndrome.
Ninety-five percent of the DBEs performed were complete. The approach (oral, anal, or both) was determined by the endoscopist, based on clinical judgement, given that at the time of the study, capsule endoscopy for guiding the type of approach was not available. The double balloon endoscope was inserted until the target lesions were reached, the enteroscopy was completed, or until it was not able to advance any further. A combination of both approaches was used in one patient diagnosed with Peutz-Jeghers syndrome (intestinal polyposis syndrome) because inspection of the entire length of the small bowel was needed. An India ink tattoo was placed at the deepest intersection point reached during the first enteroscopy. In one patient (5%) the procedure was not completed because the ileal mucosa was injured, and the decision was made to withdraw the equipment.
The most frequent indication for DBE was gastrointestinal bleeding with the suspicion of midgut bleeding, at 40% of patients, followed by intestinal polyposis syndrome in 30%, four of whom underwent DBE with a known diagnosis of Peutz-Jeghers syndrome. The frequency of inflammatory bowel disease was 20% and of altered intestinal anatomy was 10% (Table 1, Fig. 1).
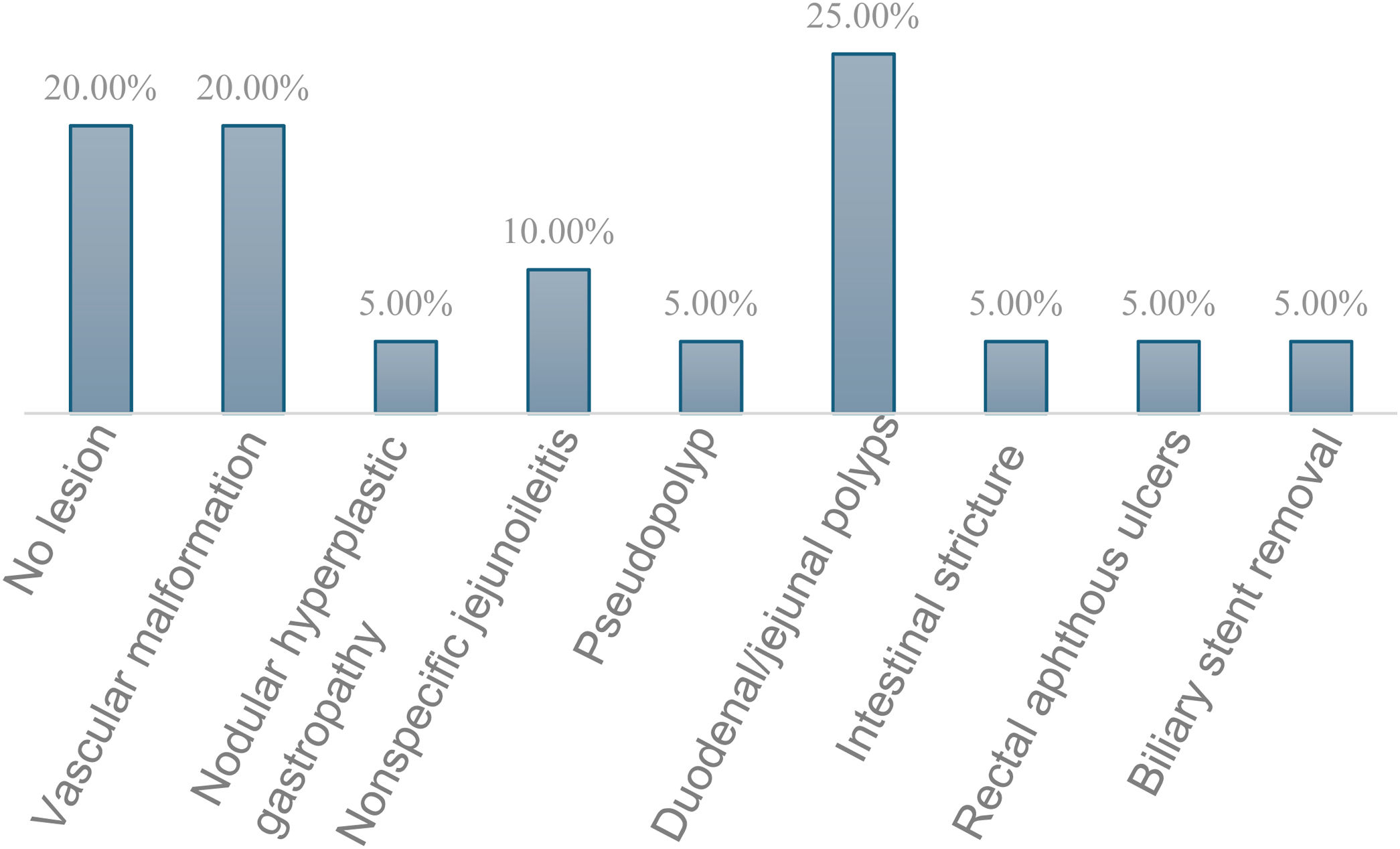
Endoscopic findingsTable 1 shows the endoscopic findings, of which the most common were mucosal lesions in the form of polyps, at 25% (Table 1, Fig. 2). No macroscopic lesion was seen in 20% of the patients. Of the 16 patients with lesions identified through DBE, 18.5% presented with lesions within the reach of a gastroscope or colonoscope; one with nodular hyperplastic gastropathy, one with a pseudopolyp in the duodenum, and one with rectal aphthous ulcers, reducing the number of findings in the midgut.
Diagnostic yield and therapeutic interventionOverall diagnostic yield was 65% (13 of the 20 patients). The absence of a pathologic finding in the midgut also played an important role for ruling out small bowel lesions in four patients.
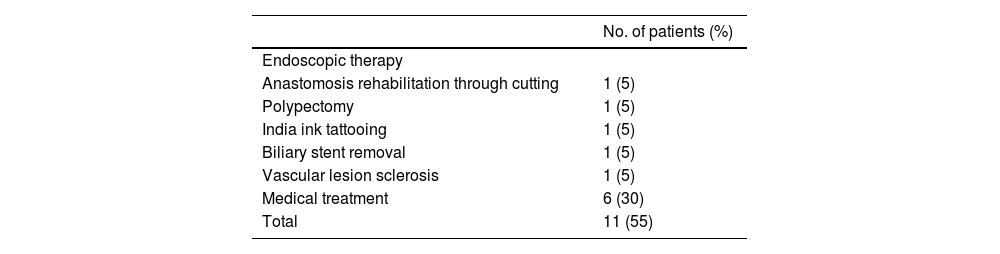
A therapeutic intervention was performed in 11 patients and was divided between endoscopic therapy and medical treatment.
Five patients required endoscopic therapy through anastomosis rehabilitation, India ink tattooing, polypectomy, biliary stent removal, and sclerotherapy with polidocanol. Endoscopic therapeutic yield with DBE was 25% (5 of the 20 patients) (Table 1).
Findings in the DBE led to medical treatment in 35% (seven of the 20 patients). No patient underwent surgical treatment after DBE. The overall therapeutic yield of DBE in therapeutic decision-making, including endoscopic and medical treatment, was 55%.
The rest of the patients (45%) required no type of intervention and will be followed as outpatients.
Gastrointestinal bleedingDBE was positive in 62.5% of the patients referred for gastrointestinal bleeding. Three patients had vascular malformations that included one patient with blue rubber bleb nevus syndrome, who underwent therapeutic endoscopy with sclerotherapy with polidocanol of lesions in the jejunum and ileum (Table 2). Two patients had an ulcerous lesion and nonspecific jejunoileitis and received only medical treatment. No lesion was detected in 25% of the patients and one patient (5%) had an incomplete DBE due to a tear in the mucosa of the ileum (Table 1). According to the literature, diagnostic yield increases when the study is performed within two weeks of bleeding (maximum yield between 48 and 72 h).7 Nevertheless, performing the procedure within that time interval is not possible in all patients because our hospital is a referral center and previous clinical, laboratory, and endoscopic (gastroscopy and/or colonoscopy) data must be corroborated, which may prolong the diagnostic approach, consequently resulting in a lower diagnostic and/or therapeutic yield.
Therapeutic intervention.
| No. of patients (%) | |
|---|---|
| Endoscopic therapy | |
| Anastomosis rehabilitation through cutting | 1 (5) |
| Polypectomy | 1 (5) |
| India ink tattooing | 1 (5) |
| Biliary stent removal | 1 (5) |
| Vascular lesion sclerosis | 1 (5) |
| Medical treatment | 6 (30) |
| Total | 11 (55) |
Anterograde DBE was performed on one patient with a history of biliary atresia, finding a portoenterostomy with a bile duct stricture. The patient underwent therapeutic endoscopy, rehabilitating the anastomosis through a longitudinal cut.
The second case was a patient with a history of liver sarcoma with a Roux-en-Y, who presented with a bile duct leak managed with a biliary stent. Anterograde DBE was performed, and the biliary stent was removed endoscopically (Table 2).
Inflammatory bowel diseaseDBE was performed on four patients diagnosed with inflammatory bowel disease. The procedure was positive in 50% of them, with findings of nodular hyperplastic gastropathy and nonspecific jejunoileitis that warranted medical treatment. DBE revealed no alterations in the remaining 50%.
Intestinal polyposis syndromesDBE was performed on six patients with an intestinal polyposis syndrome, whose diagnoses were known at the time of the procedure; four were diagnosed with Peutz-Jeghers syndrome and two with familial adenomatous polyposis. The reported findings were polyps in 83% and pseudopolyps in 16% at the level of the duodenum and ileum.
One of the patients with polyps was treated endoscopically through hot snare polypectomy, which was performed with no complications. One of the patients with Peutz-Jeghers syndrome underwent anterograde and retrograde DBE and had an India ink tattoo placed endoscopically (Table 2).
SafetyThere was a mucosal tear in the ileum in one patient, for which the procedure was ended. There were no major complications related to the insertion of the double balloon endoscope, such as perforation, bowel obstruction, bleeding, or pancreatitis.
DiscussionDBE has confirmed utility in adult patients suspected of presenting with diseases of the small bowel. Improvements in techniques and operational skills, as well as technologic advances, have resulted in the applicability of this procedure in pediatric patients.
The diagnostic yield of DBE in pediatric case series is reported at 88%.8 The overall diagnostic yield in our study was 65% (95% CI 63–96%), which is lower than that described in the literature, but the difference is not significant. Obscure gastrointestinal bleeding is reported as the most frequent indication for DBE and was present in 40% of our patients.
Modified intestinal anatomy is not frequent in the pediatric patient but 40% (95% CI 63–96 %) of the therapeutic procedures were performed in patients with stricture of the hepaticojejunal anastomosis that was repaired through cutting. Modified intestinal anatomy also occurred in a patient with a history of liver resection secondary to liver sarcoma and a Roux-en-Y procedure for biliary stent removal. There were no complications in any of the cases.
Peutz-Jeghers syndrome is a dominant autosomal hereditary disease characterized by hamartomatous gastrointestinal polyps and mucocutaneous pigmentation; 70–90% of those patients have polyps in the small bowel. Endoscopic polypectomy through DBE enables efficacious management without bowel resection, avoiding the risk for developing short intestine syndrome. DBE is useful for surveillance and treatment of hereditary polyposis syndromes.
There were no major complications in our study patients. DBE was ended in one patient due to a mucosal tear in the ileum. According to the literature, the complication rate of bleeding after polypectomy is high.9 Our study was limited for determining the safety of the procedure by the small number of patients in our sample and the fact that the study was conducted at a single center. Much attention should be paid to endoscopic therapy in the small bowel in pediatric patients, given that the small intestine is longer and more tortuous than the colon.
DBE in the pediatric patient should be performed with appropriately sized endoscopes for a satisfactory exam. According to the literature, the adequate external diameter in the pediatric population is 5.9 mm and the external diameter of the overtube is 8 mm, with a total length of 150 cm.8 The device utilized in our study was the FUJI EN-530 T, with a length of 2,000 mm. Its external diameter was 9.4 mm and the external diameter of the overtube was 13.2 mm, enabling successful procedures, given that we are a specialized center with trained personnel. However, DBE is still an infrequently performed study and can be a little-known procedure for pediatric patients. According to our results, the therapeutic endoscopic procedures were performed only once, as they were carried out at a referral center, which is a limitation for gaining hands-on experience.
ConclusionsWe consider enteroscopy assisted with a double balloon device to be a useful tool for studying midgut diseases. In our experience, DBE in pediatric patients has been shown to be feasible. Our patients received specific medical and/or therapeutic treatment, as well as targeted endoscopic treatment with minor complications, thus avoiding the performance of unnecessary studies or more invasive surgical procedures.
The importance and good results of this minimally invasive procedure should be emphasized, given that, in the majority of cases, DBE determined the therapy to be followed, directly influencing patient prognosis.
Financial disclosureNo financial support was received in relation to this study/article.
The authors declare that there is no conflict of interest.