The aim of the present study was to evaluate the feasibility of endoscopic submucosal dissection (ESD) and determine the clinical and pathologic characteristics of early gastric cancers and premalignant lesions treated with that technique at the Hospital Nacional of the Department of Health and a private clinic in Lima, Peru.
Materials and methodsA descriptive study of all pre-malignant and malignant gastric lesions treated with ESD at the Gastroenterology Service of the Hospital Arzobispo Loayza and the Clínica Angloamericana was conducted within the time frame of January 2012 and January 2017.
ResultsA total of 13 lesions were resected through ESD: 8 adenocarcinomas (61.53%), 3 adeno-mas with high-grade dysplasia (23%), and 2 adenomas with low-grade dysplasia (15.38%). Twelve lesions (92.3%) were located in the lower third of the stomach. Slightly elevated lesions (Paris classification IIa) (4 lesions, 30.76%) and mixed slightly elevated lesions with a depressed component (IIa + IIc) (4 lesions, 30.76%) predominated. The mean size of the resected specimens was 35mm. Complete resection of all lesions was achieved in 11 cases (84.6%) and en bloc resection was carried out in 11 cases (84.6%). Resection was curative in 6 cases (75%), from the total of 8 resected adenocarcinomas. One case of perforation was the only complication reported (7.6%) and it was surgically resolved.
ConclusionsThe feasibility and efficacy of ESD for the treatment of early gastric cancer was demonstrated at two healthcare centers in Lima, Peru. The complication rate was similar to that reported in the international medical literature.
El objetivo del estudio fue evaluar la factibilidad de la disección endoscópica submucosa (DES) y determinar las características clínico-patológicas de los cánceres gástricos tempranos y lesiones premalignas tratados con esta técnica en un Hospital Nacional del Ministerio de Salud y en una clínica particular en Lima, Perú.
Materiales y métodosEstudio descriptivo de todas las lesiones gástricas malignas y premalignas tratadas con DES en el Servicio de Gastroenterología del Hospital Arzobispo Loayza y la Clínica Angloamericana desde enero de 2012 a enero de 2017.
ResultadosSe resecaron un total de 13 lesiones con DES: 8 adenocarcinomas (61.53%), 3 adenomas con displasia de alto grado (23%) y 2 adenomas con displasia de bajo grado (15.38%). Doce lesiones (92.3%) se localizaron en el tercio inferior gástrico. Predominaron las lesiones plano elevadas (IIa de París; 4 lesiones, 30.76%) y las mixtas plano elevadas con componente deprimido (IIa + IIc; 4 lesiones, 30.76%). La media de tamaño del espécimen resecado fue de 35mm. Se consiguió resección completa, del total de lesiones, en 11 casos (84.6%), y resección en bloque en 11 casos (84.6%). En 6 casos (75%), de un total de 8 adenocarcinomas resecados, se observó una resección curativa. Se reportó una complicación (7.6%) la cual fue perforación y se resolvió por cirugía.
ConclusionesEn 2 centros de Lima, Perú, se demostró la factibilidad y eficacia de la DES para el tratamiento del cáncer gástrico precoz, con una tasa de complicaciones similar a la descrita en la literatura internacional.
Early gastric cancer is a malignant tumor confined to the mucosa or submucosa, with or without lymph node metastasis. Endoscopic submucosal dissection (ESD) is an advanced endoscopic technique developed at the end of the 1990s in Japan that enables en bloc resection, regardless of the size of the lesion.1,2Unlike mucosectomy, ESD makes en bloc resection possible, allowing better pathologic evaluation of the surgical specimen, a greater number of complete resections, and less premalignant and malignant local gastric lesions.3,4
Endoscopic therapy for early gastric cancer is indicated in carcinomas with close to 0% risk for lymph node metastasis. Initial studies determined that intramucosal differentiated carcinomas (cT1a) smaller than 2cm, that had no ulceration, met those criteria. Later studies found that the risk for lymph node metastasis was extremely low (under 1%) in the following lesions: 1) UL (-) cT1a differentiated carcinomas larger than 2cm in diameter, 2) UL (+) cT1a differentiated carcinomas smaller than 3cm in diameter, 3) UL (-) cT1a undifferentiated carcinomas smaller than 2cm in diameter, and 4) tumors smaller than 3cm involving the superficial submucosa with no lymphovascular infiltration (ly, v).5
The aim of the present study was to evaluate the feasibility of ESD and to determine the clinical and pathologic characteristics of early gastric cancers and premalignant lesions.
Materials and methodsA descriptive, case series study was conducted within the time frame of January 2012 and January 2017 in Lima, Peru, at two centers: the Health Department's Hospital Arzobispo Loayza, which is a national referral center for gastroenterology, and the Clínica Anglo Americana. All lesions were previously diagnosed through endoscopy with biopsy. The clinical and pathologic characteristics evaluated were: sex, age, macroscopic tumor size and type, tumor location, procedure duration, en bloc resection, complications, depth of invasion, compromised lateral margins, and histologic type. Tumor location was divided into upper, middle, and lower, according to the Japanese classification of gastric cancer.
En bloc resection was defined as that which made it possible to obtain the endoscopic specimen in a single piece with no fragmentation. Complete resection was defined as the entire removal of the cancer, leaving no neoplastic components in the lateral or vertical margins and with no lymphovascular invasion in the microscopic examination and when en bloc adenocarcinoma resection was: (I) predominantly differentiated, intramucosal, with no ulcer, disease-free lateral and vertical margins, regardless of lesion diameter; (II) lesion < than 3cm, predominantly differentiated, intramucosal, and ulcerated; (III) lesion < 2cm, predominantly undifferentiated, intramucosal, and non-ulcerated; or (IV) lesion < 3cm, predominantly differentiated, up to submucosa 1 (less than 500 μm). Curative resection was considered when there was no lymphovascular invasion and lateral and vertical margins were lesion-free, according to expanded indications.5 Recurrence was defined as the reappearance of the cancer at the lesion site (local recurrence), synchronous or metachronous reappearance, or distant metastasis.
The endoscopes employed were: the standard FUJINON model EG-590WR endoscope with 0.4% of indigo carmine, and in some cases, the LASEREO model EG-L590Z magnification endoscope. Carbon dioxide instead of air was used in the procedures performed at the Clínica Anglo Americana. The ESD technique utilized consisted of the following steps: 1) marking the perimeter of the lesion; 2) submucosal injection to produce a submucosal buffering effect and to raise the lesion; 3) an incision outside of and surrounding the marked limits of the lesion; 4) submucosal dissection. In several cases, the surrounding incision was not initially complete, to maintain the tension of the specimen to be resected, and the submucosal dissection was progressively alternated with the incision. A model DH-11GZ transparent CAP was placed at the tip of the endoscope in the majority of cases. Isotonic saline solution and/or hyaluronic acid at 0.4% (Lagricel®) was injected to create a submucosal buffer. A small quantity of indigo carmine was mixed in all the solutions and injected with a 21 to 25-caliber needle. Circumferential incision and submucosal dissection were achieved with a variety of devices that included: a Hybrid knife-I, Flush knife BT-2, Hybrid knife T, and IT-knife-2. Immediate bleeding was that in which there was a descent in hemoglobin greater than 2 g/dl from the beginning of the procedure to 24 h after the procedure. Late bleeding was defined as clinical evidence of bleeding that required endoscopic treatment, such as hematemesis or melena, 0-30 days after the procedure.
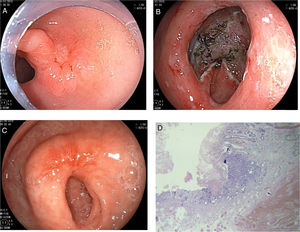
ResultsClinical and pathologic characteristicsWithin the time frame of January 2012 and January 2017, 13 early malignant and premalignant gastric lesions were treated through ESD in 13 patients (one lesion per patient). Ten (76.9%) of those procedures were performed at the Hospital Nacional Arzobispo Loayza and 3 (23%) were performed at the Clínica Anglo Americana, in Lima, Peru. Nine (69.2%) of the patients were women and 4 (30.76%) were men. Mean patient age was 70 years (range: 44-85 years). Mean lesion size was 35mm (range: 20-50 mm). Twelve (92.3%) of the lesions were located in the lower region and one (7.6%) was in the middle region. Tables 1 and 2 show the clinical and pathologic characteristics of the patients and Figure 1 illustrates a case of ESD.
Clinical and pathologic characteristics of the patients/lesions.
| Patients/Lesions | 13/13 |
| Men (%), Women (%) | 4 (30.7), 9 (69.23) |
| Mean age (range) | 70 (44-85) |
| Location, n (%) | |
| Middle | 1 (7.6) |
| Lower | 12 (92.3) |
| Macroscopic type, n (%) | |
| IIa + IIc | 4 (30.76) |
| IIa | 4 (30.76) |
| 0-Is | 2 (15.38) |
| IIc + IIa | 1 (7.6) |
| IIc | 1 (7.6) |
| III + IIc | 1 (7.6) |
| Lesion size, n (%) | |
| < 20 mm | 3 (23) |
| 20-30 mm | 5 (38.46) |
| > 30 mm | 5 (38.46) |
| Ulceration, n (%) | |
| Absent | 10 (76.92) |
| Present | 3 (23) |
| Procedure duration | |
| Mean (range), min | 109 (67-228) |
| Complications, n (%) | |
| Perforation | 1 (7.6) |
| Immediate or late bleeding | 0 |
| Mortality | 0 |
Histopathologic characteristics of the patients.
| Gastric lesions | n (%) |
|---|---|
| Premalignant lesions | |
| Total | 5 |
| Resection | |
| En bloc | 5 (100) |
| R 0 | 5 (100) |
| Histologic type | |
| Adenoma with high-grade dysplasia | 3 (60) |
| Adenoma with low-grade dysplasia | 2 (40) |
| Gastric cancer | |
| Total | 8 |
| Resection | |
| En bloc | 6 (75) |
| R 0 | 6 (75) |
| Curative | 6 (75) |
| Histologic type | |
| Well differentiated adenocarcinoma | 8 (100) |
| Non-differentiated adenocarcinoma | 0 |
| Depth of invasion | |
| Mucosa (M) | 5 (62.5) |
| Submucosa (SM1) | 1 (12.5) |
| Submucosa (SM2) | 2 (25) |
Endoscopic submucosal dissection (ESD) of pre-pylorus lesion. A) Slightly depressed lesion with 2-cm elevated edges, poorly defined edges, and irregular surface. B) Final result of the submucosal dissection. C) ESD scar 8 weeks after the procedure. D) Intramucosal well differentiated adenocarcinoma with disease-free surgical edges.
Endoscopic devices and injection solutions
The Hybrid knife-I was used in 8 cases (61.53%); the Flush knife BT-2 in 3 cases (23%); the Hybrid knife T in one case (7.7%), and the IT-knife-2 in one case (7.7%). To raise the lesions, physiologic saline serum was used in 2 cases (15.3%), methylene blue in 4 cases (30.7%), and hyaluronic acid in 7 cases (58.8%).
Histologic evaluation and macroscopic tumor typeOf the 13 resected lesions, 8 (61.53%) were well-differentiated adenocarcinomas; 5 (38.46%) were adenomas, of which 3 (23%) had high-grade dysplasia and 2 (15.38%) had low-grade dysplasia. Regarding macroscopic appearance, 4 (30.76%) lesions were described as II-a; 4 (30.76%) lesions as IIa + IIc; 2 (15.38%) lesions as 0-Is; one (7.69%) lesion as IIc + IIa; one (7.69%) lesion as IIc; and one (7.69%) lesion as III + IIc. Only 3 (23%) lesions presented with ulceration.
Cure rate and complicationsESD was indicated for 6 (75%) of the 8 patients with gastric cancer according to the expanded criteria for the submucosal dissection and 2 (25%) of the cancer patients underwent the procedure because they met the absolute criteria for submucosal dissection described by Oda et al.4 One patient with lesion ulceration had submucosal involvement (SM1) and met the cure criteria. En bloc resection was achieved in all the premalignant lesions (5 lesions) and in 6 of the 8 adenocarcinomas (75%). Two (25%) of the 8 adenocarcinomas required hybrid resection (submucosal dissection and snare resection).
Of the 8 patients diagnosed with adenocarcinoma, curative resections were achieved in 6 patients (75%) with gastric adenocarcinoma. The depths of invasion found were: 2 patients with SM2 submucosal invasion and one patient with SM1 submucosal invasion. The remaining 5 patients were diagnosed with adenocarcinoma limited to the mucosa. There were no neoplastic lesions found at endoscopy performed in the patients diagnosed with adenocarcinoma at the follow-up at 6 months. Mean procedure duration was 109min (range: 67-228 min). The muscularis propria layer was damaged in one of the cases, with no air observed in the abdominal cavity, and was resolved through the placement of 3 endoclips. Perforation was reported in one patient and it was surgically resolved, because technical endoscopic difficulties did not allow adequate closure of the defect. The patient had favorable progression. No deaths were reported (Table 3).
Characteristics of the study patients.
| No. | Age (years) | Sex | Location (third) | Macroscopic type | Lesion size | Ulceration | Complications | Type of resection | Histologic type | Depth of invasion | Endoscopic knife | Site |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 70 | W | Lower | IIa+IIc | 35x35 mm | Yes | No | En bloc | Well differentiated adenocarcinoma | Mucosa | IT-Knife 2 | HNAL |
| 2 | 44 | W | Lower | IIa+IIc | 50x40 mm | No | No | En bloc | Well differentiated adenocarcinoma | Mucosa | Hybrid knife I | HNAL |
| 3 | 65 | W | Lower | IIa | 41x18 mm | No | No | En bloc | Well differentiated adenocarcinoma | Mucosa | Hybrid knife I | HNAL |
| 4 | 60 | M | Lower | 0-Is | 37x30 mm | Yes | No | En bloc | Tubulovillous adenoma with low-grade dysplasia | Mucosa | Hybrid knife I | HNAL |
| 5 | 75 | W | Lower | IIa | 25x15 mm | Yes | No | En bloc | Tubular adenoma with low-grade dysplasia | Mucosa | Hybrid knife I | HNAL |
| 6 | 78 | W | Lower | IIa | 45x30 mm | No | No | En bloc | Adenoma with high-grade dysplasia | Mucosa | Hybrid knife I + REM | HNAL |
| 7 | 85 | M | Lower | IIc | 35x20 mm | No | No | En bloc | Adenoma with high-grade dysplasia | Mucosa | Hybrid knife I + REM | HNAL |
| 8 | 83 | W | Lower | IIa | 20x20 mm | No | Perforation | Hybrid | Well differentiated adenocarcinoma | Submucosa (SM2) | Hybrid knife I | HNAL |
| 9 | 75 | W | Lower | IIc+IIa | 35x20 mm | No | No | En bloc | Well differentiated adenocarcinoma | Mucosa | Hybrid knife T | HNAL |
| 10 | 63 | W | Middle | 0-Is | 26x32 mm | No | No | En bloc | Well differentiated adenocarcinoma | Submucosa (SM1) | Flush knife | Clínica Anglo Americana |
| 11 | 66 | W | Lower | IIa+IIc | 31x30 mm | No | No | En bloc | Tubular adenoma with high-grade dysplasia | Mucosa | Flush knife | Clínica Anglo Americana |
| 12 | 77 | M | Lower | IIa+IIc | 20x20 mm | No | No | Hybrid | Well differentiated adenocarcinoma | Submucosa (SM2) | Flush knife | Clínica Anglo Americana |
| 13 | 77 | M | Lower | III+ IIc | 35x23 mm | No | Microperforationa | En bloc | Well differentiated adenocarcinoma | Mucosa | Hybrid knife T | HNAL |
The first case report of submucosal dissection of early gastric cancer in Peru was presented by Vargas et al.6 in 2012, with no others reported in the country since then.
The incidence of lymph node metastasis was studied by Gotoda et al., who analyzed more than 5,000 gastrectomies with D2 lymph node dissection. That study published both the absolute and expanded criteria for ESD of early gastric cancer lesions. According to those criteria, lymph node metastasis incidence is below 1%.7 In our study, 3 patients had submucosal invasion: one patient up to SM1 and 2 patients to SM2. In the patient with SM1, conservative treatment was decided upon, given that all the Godota criteria were met: well differentiated lesion smaller than 3cm (it measured 1.2cm in diameter and only 300μm in depth).
The importance of early gastric cancer diagnosis is that if the lesion is resected and meets the curative criteria defined by Oda et al.,45-year survival can be greater than 95%, similar to that for surgery.5 Fukunaga et al. demonstrated greater survival (97.1 vs 85.8%; p = 0.01) and fewer adverse effects (6.8 vs 28.4%; p < 0.01) in patients that underwent ESD, compared with those that had surgery in a study that evaluated follow-up at 5 years in patients with differentiated early gastric cancer according to the expanded criteria.8 The incidence of gastric cancer recurrence after submucosal dissection has been reported at 0-1%.9 In our population, curative resection (6 out of 8 patients diagnosed with adenocarcinoma) was 75%, which is close to that reported in the international literature. We believe that was due to the experience of the endoscopist in performing the procedure and the adequate patient selection which was carried out following the Godota criteria, as well as working in two well-equipped endoscopic centers with the necessary resources for resolving any immediate complication and a team skilled in performing advanced endoscopic therapy.
Serious complications of the ESD procedure are bleeding and perforation, and incidence of the latter is 0-5%. Oka et al. reported the incidence of perforation at 9.7%, when ESD was performed in cases of non-ulcerated lesions.10 In our study on 13 patients, there was only one perforation and it was not resolved endoscopically (7.6%). Despite having detected the defect during the procedure, endoscopic closure was not achieved, due to technical difficulties. The patient progressed favorably after the surgery.
Oka et al. described an incidence of bleeding of 22.6% for ulcerated lesions and 6.2% for non-ulcerated lesions. Likewise, lesion size and location were found to be risk factors for bleeding (lesions at the greater curvature tend to bleed more). In our experience, one third of the lesions were larger than 30mm, but bleeding was not reported. Most likely that was due to the fact that both study sites had the necessary equipment for stopping immediate bleeding, such as Coagrasper forceps and other instruments, as well as having strict intra-procedural hemodynamic monitoring. The majority of lesions were located in the lower third of the stomach (92.3%) and were non-ulcerated lesions (76.9%), which could have reduced the risk for bleeding.
Our study is important because it is the first published case series on patients from 2 centers in Lima, Peru (the Hospital Nacional of the Health Department [MINSA, the Spanish acronym] and a private clinic) that demonstrates the feasibility and efficacy of the endoscopic technique in a larger number of cases with tumors of different sizes and locations, as well as a complication rate that coincided with international experiences. One of the study's limitations was the reduced sample size and the short follow-up period. However, we believe it is relevant to communicate the advances made with this effective technique. More studies should be conducted to evaluate patient follow-up and assess disease recurrence.
In conclusion, ESD is an advanced endoscopic technique that enables early extraction of gastric cancer in a single specimen with no fragmentation, even in large or ulcerated lesions, favoring a lower rate of local disease recurrence and gastric cancer cure in selected cases. The procedure was performed at two centers in Lima and showed complete, curative, en bloc resection rates, together with complication rates similar to those reported in the international literature. Endoscopic submucosal dissection enables the reduction of surgery in selected patients with gastric cancer and paves the way for the detection of more cases of early gastric cancer through screening programs in Peru.
Ethical disclosuresProtection of human and animal subjects.The authors declare that the procedures followed were in accordance with the regulations of the relevant clinical research ethics committee and with those of the Code of Ethics of the World Medical Association (Declaration of Helsinki).
Confidentiality of data.The authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consent.The authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Financial disclosureNo financial support was received in relation to this study.
Conflict of interestThe authors declare that there is no conflict of interest.
Please cite this article as: Chirinos Vega JA, Vargas G, Alcántara C, Zapata J. Disección submucosa endoscópica como tratamiento de cáncer gástrico temprano: experiencia en 2 centros de Lima, Perú. Revista de Gastroenterología de México. 2018;83:393–399.