Endoscopic ultrasound-guided gastroenterostomy (EUS-GE) has recently become an alternative to surgery in the treatment of gastric outlet obstruction (GOO), mainly in patients that are not candidates for surgery or the endoscopic placement of a duodenal stent.1
We present herein the case of a 56-year-old man with advanced pancreatic cancer and oral intolerance secondary to duodenal stricture caused by tumor infiltration. Endoscopic ultrasound-guided gastrojejunostomy (EUS-GJ) was performed as part of palliative treatment.
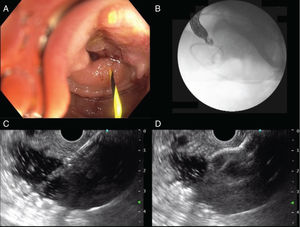
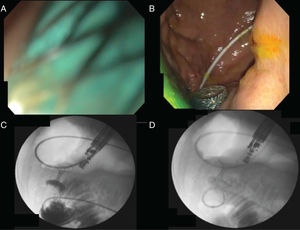
With a therapeutic gastroscope, the gastric content was initially aspirated, and the stricture site identified. A 0.035” hydrophilic guidewire (Jagwire™ Straight Tip, Boston Scientific, USA) was introduced through the stricture, using an 8.5 Fr stent introducer (Oasis® One Action Stent Introduction System, Cook Medical, USA) (Fig. 1A). When the guidewire was in front of the angle of Treitz, the stent introducer and gastroscope were removed, leaving the hydrophilic guidewire in the jejunum. A 7 Fr nasobiliary drainage catheter (Cook Medical, USA) was placed through the guidewire to instill approximately 800 cc of injectable water (Fig. 1B). Twenty milligrams of intravenous butylhyoscine were administered to reduce peristaltic movement, and the linear echoendoscope (GF-UCT180 Olympus Medical Systems, Tokyo, Japan) was introduced. The jejunal segment was identified with water in its interior, through transgastric echoendoscopic scanning, and its closeness to the nasobiliary drain was corroborated through fluoroscopy. Finally, 30 cc of contrast medium with methylene blue were instilled to opacify the targeted jejunal segment. Gastrojejunostomy was performed with the lumen-apposing stent, using electrocautery (Hot AXIOS™ Stent 20 × 10 mm, Boston Scientific, USA), through direct puncture (no guidewire) and diathermy (Fig. 1C and D). The flow of methylene blue was corroborated through endoscopic vision (Fig. 2A and B), and then through fluoroscopy (Fig. 2C and D).
A) Advance of the hydrophilic guidewire through the malignant duodenal stricture. B) Fluoroscopy-guided placement of the nasobiliary drainage catheter in front of the angle of Treitz. C) Endoscopic ultrasound-guided puncture of the targeted segment. D) Release of the first flange of the lumen-apposing stent.
A) Intra-channel release of the second flange. B) Endoscopic confirmation of the release of the second flange (note the presence of methylene blue). C) Contrast medium reflux from the jejunal segment into the stomach through the stent. D) Wash-out of the contrast medium from the stomach into the jejunal segment.
In 2002, Fritscher-Ravens et al. presented the first use of the EUS-GE technique in an animal model,2 but it was not until special devices were created several years later that the development of the procedure was completed, and it was applied in humans. In 2012, Binmoeller and Shah, utilizing a lumen-apposing stent, reported on the feasibility of the procedure in 5 pigs.3 Recently, direct puncture and balloon-assisted puncture are the 2 main techniques that have been described.1,4 In a multicenter study that included 74 patients, the 2 techniques were compared. Both were found to be equally effective, but the direct puncture technique was a shorter procedure.5
Currently, the main indication for EUS-GE is GOO due to obstruction of the antrum-pylorus region, as well as of the first, second, and third part of the duodenum. Contraindications are obstruction of the gastric corpus, obstruction of the first part of the jejunum or the fourth part of the duodenum if the proximal jejunum cannot be reached, large volume ascites, and perigastric varices that prevent an adequate puncture window.4,6
We utilized a hybrid technique, a product of the experience of the Manuel Pérez-Miranda group in Valladolid, Spain. We advanced a nasobiliary drainage catheter (without a balloon) through a hydrophilic guidewire up to the targeted segment, enabling it to be filled with water or saline solution. We then added contrast medium and methylene blue as safety measures. The use of a nasobiliary catheter can increase costs, given that water, contrast medium, and methylene blue can be directly instilled using the gastroscope. However, we believe the catheter provides better fluoroscopic vision control because it prevents erratic distribution of the contrast medium in the small bowel. The lumen-apposing stent release was direct (free-hand), aided only by the electrocautery tip.1,4
In 2017, Khashab et al. described the first 10 cases of EUS-GE in the United States.6 In 2 later multicenter studies, the technique was compared with the standard procedure of surgical gastroenterostomy. Both the Pérez-Miranda group and the Khashab et al. studies showed the safety and efficacy of EUS-GE, situating it as a therapeutic option for patients with GOO.7,8 In their study, Chen et al. compared EUS-GE with the placement of enteral stents, demonstrating that EUS-GE was an effective option, with a lower number of reinterventions in cases of malignant GOO.9 Ours is the first performance of EUS-GE reported in Mexico and we believe, with the adequate human and material resources, it is a procedure that can be performed with high success rates and few adverse effects.
Ethical considerationsThe authors declare that the present article contains no information that could identify the patient and it meets the current bioethics research regulations. Informed consent was requested of the patient.
AuthorshipRodrigo Soto-Solis, Mario R. Pineda-De Paz, Mario A. Gallardo-Ramirez, and Adriana Diaz-Coppe contributed to the concept, design, literature review, and drafting of the manuscript. Georgina Osorno-Diaz and Rodrigo Soto-Solis edited the video. Rodrigo Soto-Solis and Mario R. Pineda-de Paz collected the data and images and reviewed the manuscript to verify the intellectual content. All the authors had access to the manuscript and approved the final version.
Financial disclosureNo specific grants were received from public sector agencies, the business sector, or non-profit organizations in relation to this study.
Conflict of interestThe authors declare that there is no conflict of interest.
Please cite this article as: Soto-Solis R, Pineda-de Paz MR, Osorno-Diaz G, Gallardo-Ramirez MA, Diaz-Coppe A. Gastroenterostomía guiada por ultrasonido endoscópico en obstrucción al flujo de salida gástrico (con vídeo). Revista de Gastroenterología de México. 2021;86:101–103.