Surgical site infection is defined as an infection related to the surgical procedure in the area of manipulation occurring within the first 30 postoperative days. The diagnostic criteria include: purulent drainage, isolation of microorganisms, and signs of infection.
AimsTo describe the epidemiologic characteristics and differences among the types of prophylactic regimens associated with hospital-acquired infections at the general surgery service of a tertiary care hospital.
Material and methodsThe electronic case records of patients that underwent general surgery at a tertiary care hospital within the time frame of January 1, 2013 and December 31, 2014 were reviewed. A convenience sample of 728 patients was established and divided into the following groups: Group 1: n=728 for the epidemiologic study; Group 2: n=638 for the evaluation of antimicrobial prophylaxis; and Group 3: n=50 for the evaluation of multidrug-resistant bacterial strains in the intensive care unit. The statistical analysis was carried out with the SPSS 19 program, using the Mann-Whitney U test and the chi-square test.
ResultsA total of 728 procedures were performed (65.9% were elective surgeries). Three hundred twelve of the patients were males and 416 were females. Only 3.98% of the patients complied with the recommended antimicrobial prophylaxis, and multidrug-resistant bacterial strains were found in the intensive care unit.
DiscussionA single prophylactic dose is effective, but adherence to this recommendation was not adequate.
ConclusionsThe prophylactic guidelines are not strictly adhered to in our environment. There was a significant association between the development of nosocomial infections from multidrug-resistant germs and admission to the intensive care unit.
Se define infección de sitio quirúrgico como infecciones relacionadas con el procedimiento quirúrgico en el área manipulada en los primeros 30 días. Criterios diagnósticos incluyen: drenaje purulento, aislamiento de microorganismos, signos de infección.
ObjetivosDescribir las características epidemiológicas y las diferencias entre los tipos de esquemas profilácticos asociados a infecciones nosocomiales en el servicio de Cirugía General en un hospital de tercer nivel en el periodo comprendido del 1 de enero del 2013 y el 31 de diciembre del 2014.
Material y métodosRevisión del expediente electrónico de pacientes de Cirugía General en un hospital de tercer nivel durante el periodo comprendido entre el 1 de enero del 2013 y el 31 de diciembre del 2014. Se estableció una muestra a conveniencia de 728 pacientes dividida en grupos: grupo 1 n=728, para estudio epidemiológico; grupo 2 para evaluar profilaxis antimicrobiana, n=638, y, finalmente, grupo 3, n=50 para evaluar el desarrollo de cepas multirresistentes en la Unidad de Cuidados Intensivos. Para el análisis estadístico se emplearon SPSS 19, prueba U de Mann-Whitney y ji al cuadrado.
ResultadosSetecientos veintiocho procedimientos (65.9% electivos), 312 hombres y 416 mujeres; el porcentaje de cumplimiento de profilaxis antimicrobiana fue solo del 3.98%; encontramos desarrollo de múltiples cepas resistentes en cuidados intensivos.
DiscusiónUna sola dosis profiláctica es efectiva en cirugía; sin embargo, el apego a esta recomendación no es el adecuado.
ConclusionesNo existe un adecuado apego a las guías de profilaxis en nuestro medio. Existe una asociación significativa entre el desarrollo de infecciones nosocomiales por gérmenes multirresistentes y el ingreso a la Unidad de Cuidados Intensivos.
Surgical site infections are defined as infections related to the surgical procedure that are produced near the surgical incision within the first 30 days after the surgical procedure or within one year (in the case of implants) if the implant is left in place.1 The criteria for defining surgical site infection are the following:
- a.
Superficial incisional infection: this is produced within the first 30 days after surgery and involves the skin or subcutaneous cellular tissue, presenting: 1) purulent drainage, 2) isolation of microorganisms obtained through culture with the aseptic technique, and 3) at least one of the following symptoms: signs of local infection, pain, hypersensitivity.
- b.
Deep infection: within 30 days after surgery (one year in the case of implants or prostheses) and clinical evidence of infection and/or positive culture.
- c.
Organ or surgical space infection: they include clinical data and/or positive culture of the areas manipulated during the surgical procedure.
The World Health Organization defines hospital-acquired infection as that which is contracted during hospital stay in a patient with no previous or added infection.1 They are infections that are contracted in the hospital, but manifested after release from the hospital.
Multi-drug resistant germs are those microorganisms that are resistant to 2 or more groups of antimicrobial agents.
Antimicrobial prophylaxis includes the administration of antimicrobial agents for preventing surgical site infection. Current antimicrobial prophylaxis guidelines1 state that studies in the literature have an important limitation for finding statistically significant differences between the efficacy of prophylactic antibiotics (cases) and controls (placebo, no treatment or other antibiotics) due to their design and the low surgical site infection rates.1
Numerous studies have shown that the administration of a single dose of chemoprophylaxis is as effective as numerous doses in a great variety of surgical procedures. Additional intraoperative doses are necessary in the following cases: patients with blood loss above 1,500ml and in surgical procedures longer than 4h, given that they require adequate levels of the antimicrobial agent at the surgical site to obtain the benefit of chemoprophylaxis.2 It has been proposed that adherence to guideline management can reduce the surgical site infection rate to under 0.5% in clean wounds, under 1% in clean-contaminated wounds, and under 2% in contaminated wounds. A recent meta-analysis that included 250 clinical trials, 4,809 patients, and 23 different types of surgery estimated a decrease in the surgical site infection rate of 0.19 to 0.82% among patients that received prophylactic treatment vs those that did not.3
The current recommendation is a single dose administered 60min before the surgical procedure.4 A cohort study showed that antimicrobial prophylaxis was discontinued within 24-h after surgery end in only 40.7% of the cases,5 showing that the use of intrahospital antimicrobial agents can be improved in 30-50% of the cases, eliminating their unnecessary use and preventing the development of resistance.6–8
The optimal prophylactic agent employed is active against the pathogens most likely to contaminate the surgical site, is administered in adequate doses and time-concentrations when potential contamination is expected, is safe, and is administered within the shortest period of time in which adverse effects, resistance, and costs can be reduced to a minimum.1
AimTo describe the epidemiologic characteristics and differences between the types of prophylactic regimens associated with hospital-acquired infections in the general surgery service of a tertiary care hospital within the time frame of January 1, 2013 and December 31, 2014.
Materials and methodsThe electronic case records were reviewed of patients that underwent surgical treatment, had nosocomial and surgical site infections, and were in the general surgery and intensive care services within the time frame of January 1, 2013 and December 31, 2014. A total of 1,875 registered procedures were found.
A descriptive, cross-sectional, retrospective study was conducted within the time frame of January 1, 2013 and December 31, 2014. A convenience sample was established using nonprobabilistic methods. Males and females ranging from 15 to 99 years of age that received surgical treatment at the General Surgery service were included. The total sample of 728 patients was divided into 3 different groups for their analysis as follows: 1) local or referred patients, with surgical intervention or re-intervention, and with or without evidence of infection, n = 728; 2) patients admitted to and operated on exclusively at our service, eliminating referred patients, dirty wounds, and patients that had completed antimicrobial prophylaxis, n = 638; and 3) exposed patients, which were those with nosocomial infections managed in the intensive care unit, and non-exposed patients, which were those with nosocomial infection not managed in the intensive care unit, n = 50.
The study variables were: sex, age, surgical procedure, surgical wound, elective or emergency surgery, prophylactic regimen (in accordance or not with that recommended in the international guidelines), antimicrobial employed, hospital stay, re-admission, re-intervention, management in intensive care unit, isolated pathogens, and death.
The statistical analysis was carried out using the SPSS version 19 software program. Frequency distribution and numerical methods, measures of central tendency, arithmetic means, and medians were analyzed. Nonparametric tests were employed, given that the sample did not show a normal distribution in the Kolmogorov-Smirnov and Shapiro-Wilk tests. The Mann-Whitney U test was used to analyze the quantitative vs the categorical variables and the Pearson's chi-square test was used for the dichotomous variables.
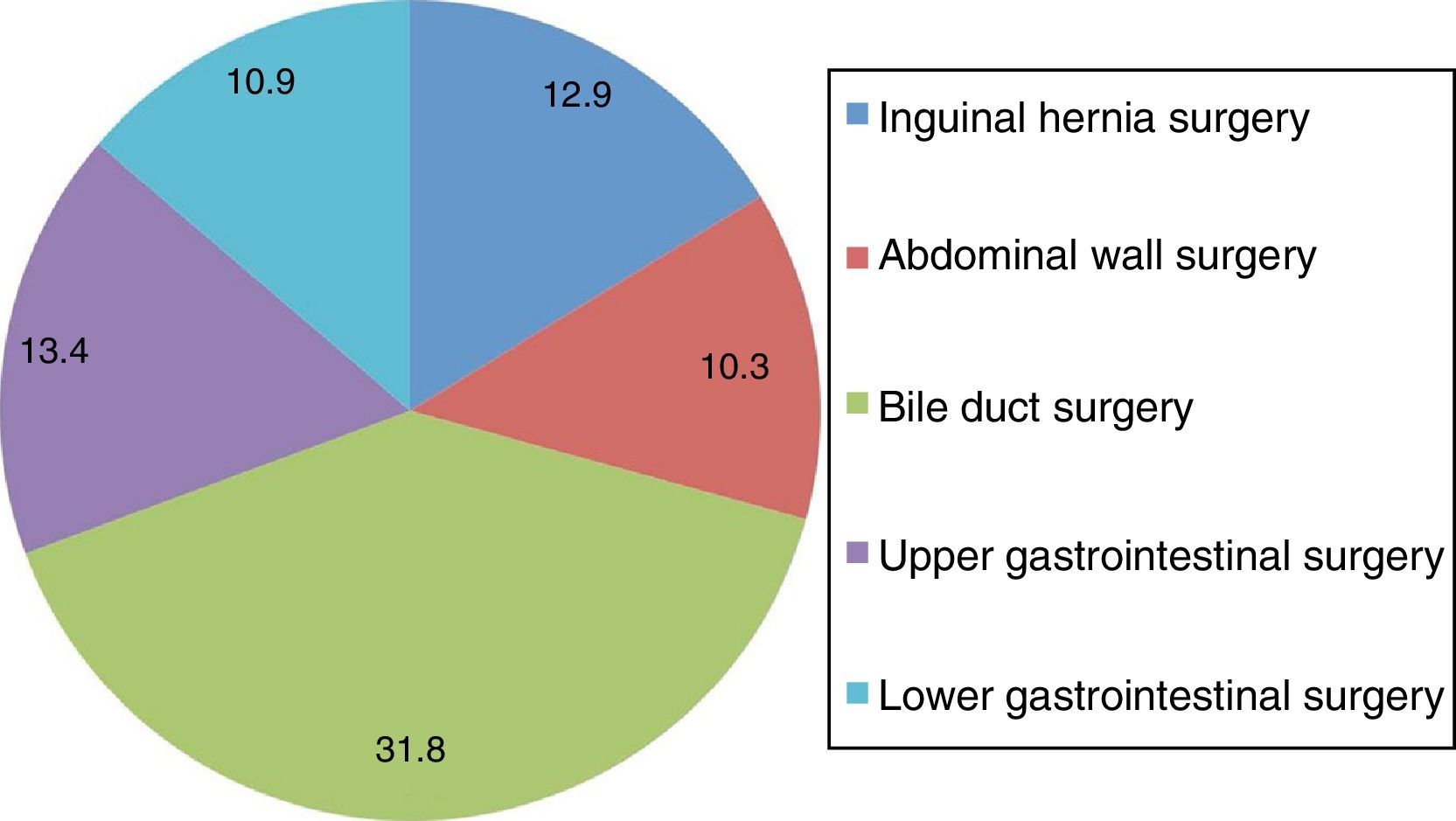
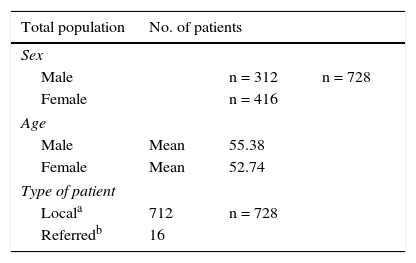
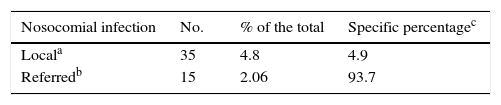
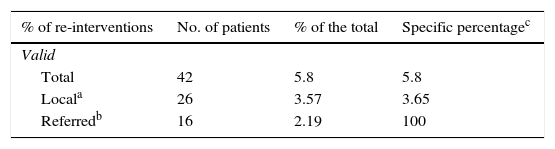
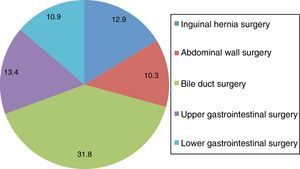
ResultsThe sample of 728 patients included 312 males and 416 females. Their approximate mean age was 55 and 52 years, respectively (Table 1A). Laparoscopic cholecystectomy was performed in 28.16% of the patients. A total of 12.23% of the patients underwent subcutaneous cellular tissue surgeries, 9% had appendectomies, 6.7% had inguinal repair with prosthesis, 5.8% underwent laparoscopic fundoplication, 4.9% had umbilical hernia repair, and 4.0% had inguinal hernia repair, among others (Fig. 1). At our hospital center, 712 patients (local) and 16 referred patients were operated on. The rate of hospital-acquired infection was 6.86%, and 4.8% corresponded to the “local” group. The surgical site infection rate was 2.6%, mean hospital stay was 32.4 vs 4.2 days for infected and non-infected patients, respectively. Mean antimicrobial cost was $20,733.00 vs $390.00 MXN in infected and non-infected patients, respectively (Table 1B). There were statistically significant differences in the infected patient group in the variables of management in intensive care, re-intervention, and death (Table 1C).
Surgeries performed at the General Surgery Service from January 1, 2013 to December 31, 2014. Pie graph showing the surgeries performed at the General Surgery Service within the time frame of January 1, 2013 to December 31, 2014 and the percentages of each procedure.
Source: Electronic case records/ SSS-SIAH- December-2014.
Infected vs non-infected patients.
| Nosocomial infection | No. | % of the total | Specific percentagec |
|---|---|---|---|
| Locala | 35 | 4.8 | 4.9 |
| Referredb | 15 | 2.06 | 93.7 |
| Non-infected patient | Age (years) | Total antimicrobial cost | Days of hospital stay |
|---|---|---|---|
| Mean | 53.15 | 390.3 | 4.29 |
| Standard deviation | 17.2 | 1,922.9 | 4.066 |
| Minimum | 15 | 0 | 0 |
| Maximum | 97 | 42,570 | 46 |
| Infected patient | Age (years) | Total antimicrobial cost | Days of hospital stay |
|---|---|---|---|
| Mean | 63.68 | 20,733.6 | 32.4 |
| Standard deviation | 16.5 | 43,281.6 | 34.7 |
| Minimum | 19 | 12.4 | 0 |
| Maximum | 91 | 235,724 | 146 |
Infected vs non-infected patients.
| % of re-interventions | No. of patients | % of the total | Specific percentagec |
|---|---|---|---|
| Valid | |||
| Total | 42 | 5.8 | 5.8 |
| Locala | 26 | 3.57 | 3.65 |
| Referredb | 16 | 2.19 | 100 |
| % of admissions to the ICU | No. of patients | % of the total | Specific percentagec |
|---|---|---|---|
| Valid | |||
| Total | 30 | 4.1 | 4.1 |
| Locala | 20 | 2.7 | 2.8 |
| Referredb | 10 | 1.4 | 62.5 |
| Deaths | No. of patients | % of the total | Specific percentagec |
|---|---|---|---|
| Valid | |||
| Total | 12 | 1.6 | 1.6 |
| Locala | 4 | 0.5 | 0.56 |
| Referredb | 8 | 1.1 | 50 |
| Type of surgery | No. of patients | % of the total |
|---|---|---|
| Valid | ||
| Elective | 480 | 65.9 |
| Emergency | 248 | 34.1 |
| Infections by type of surgery | No. of patients | % of the total |
|---|---|---|
| Valid | ||
| Elective | 9 | 18 |
| Emergency | 41 | 82 |
| Surgical site infections | No. of patients | % of the total |
|---|---|---|
| Locala | 19 | 2.6 |
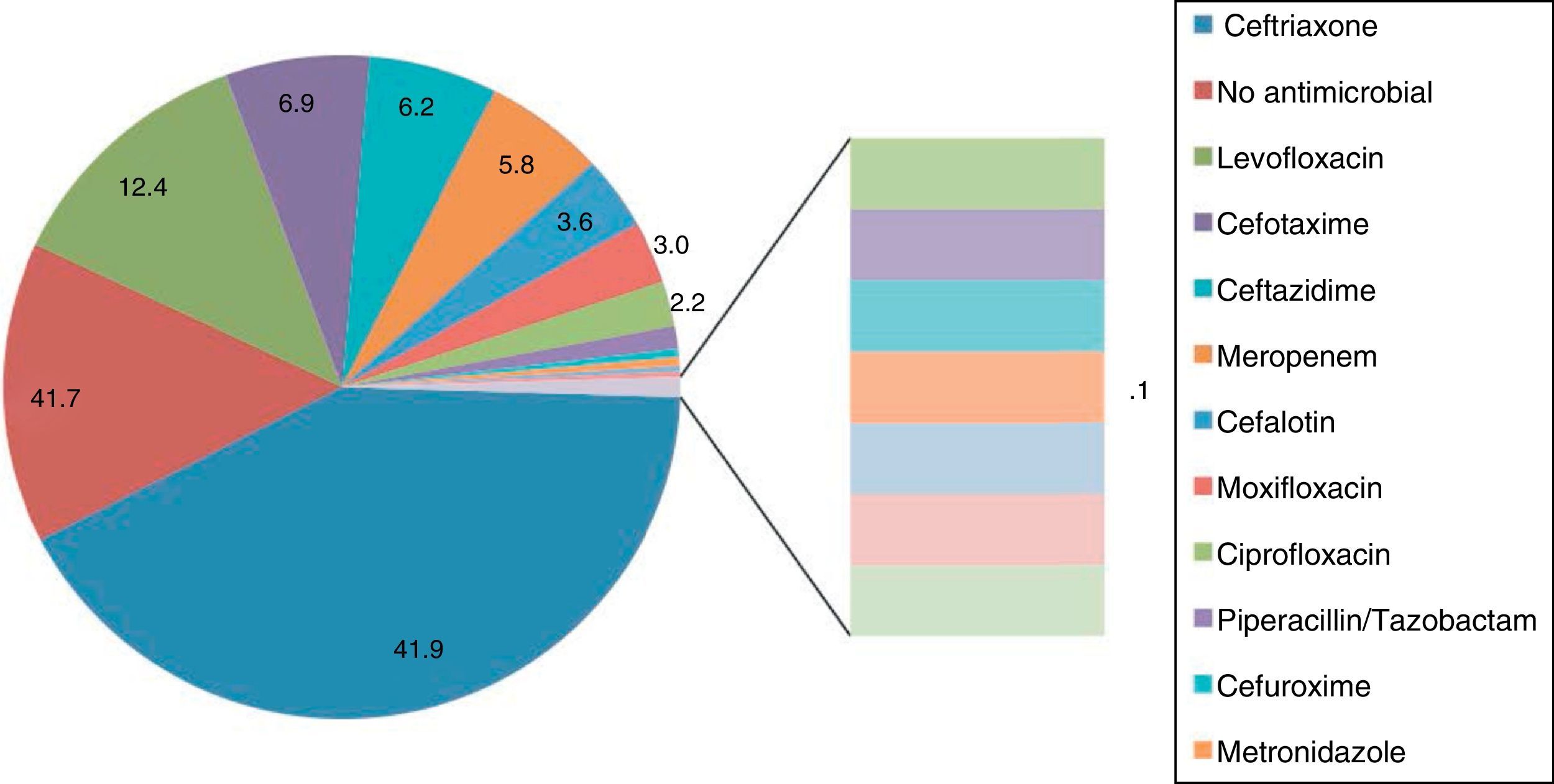
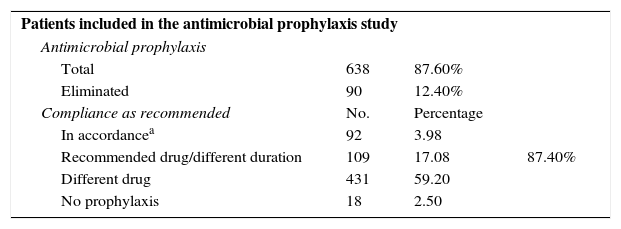
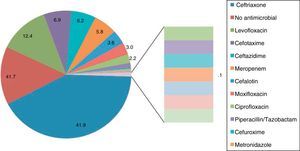
We found that compliance with the antimicrobial prophylactic regimens in the international guidelines was only 3.98% and ceftriaxone was the most widely used prophylactic agent in 41.9% of the patients. Even though the drug was chosen correctly in 20% of the patients, it was not prescribed according to the recommended regimen. Eighty-one percent of the patients were released with antibiotic treatment, even when there was no evidence of infection. Thirty-four percent of those patients received cefuroxime (Table 2). The statistical analysis showed no statistically significant differences between surgical site infection and the type of antimicrobial regimen employed (Fig. 2).
Antimicrobial prophylaxis and use of antimicrobial agents. HCSAE 2013-2014.
| Patients included in the antimicrobial prophylaxis study | |||
| Antimicrobial prophylaxis | |||
| Total | 638 | 87.60% | |
| Eliminated | 90 | 12.40% | |
| Compliance as recommended | No. | Percentage | |
| In accordancea | 92 | 3.98 | |
| Recommended drug/different duration | 109 | 17.08 | 87.40% |
| Different drug | 431 | 59.20 | |
| No prophylaxis | 18 | 2.50 | |
| Use of medications | ||
|---|---|---|
| Medications used as prophylactic agents | No. of patients | Percentage |
| Noneb | 107 | 15 |
| Ceftriaxone | 305 | 42 |
| Ceftazidime | 45 | 6 |
| Levofloxacin | 90 | 12 |
| Moxifloxacin | 22 | 3 |
| Ciprofloxacin | 16 | 2 |
| Meropenem | 42 | 6 |
| Cefotaxime | 50 | 7 |
| Cefalotin | 26 | 4 |
| Others | 25 | 3 |
| Medications indicated upon release | No. of patients | Percentage |
|---|---|---|
| Noneb | 135 | 19 |
| Cefuroxime | 246 | 34 |
| Cefalexin | 137 | 19 |
| Levofloxacin | 98 | 14 |
| Cefaclor | 36 | 5 |
| Others | 76 | 10 |
Antimicrobials used as prophylactic agents at the General Surgery Service of the HCSAE. The antimicrobials most widely used as prophylactic agents at the General Surgery Service within the time frame of January 1, 2013 to December 31, 2014 are summarized in the graph, as well as the percentages of each one. The most widely used drug was ceftriaxone.
Source: Electronic case records/ SSS-SIAH- December-2014.
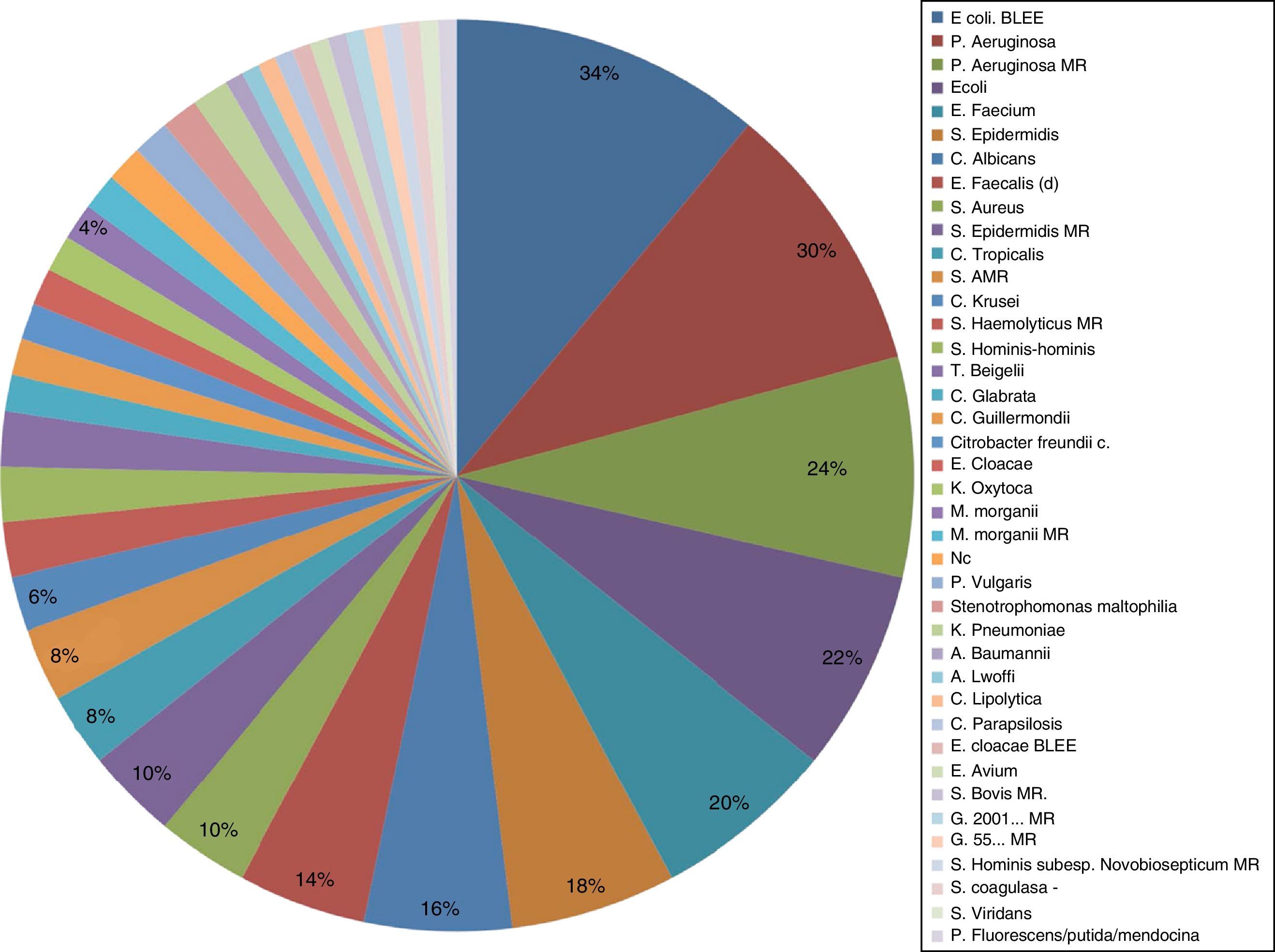
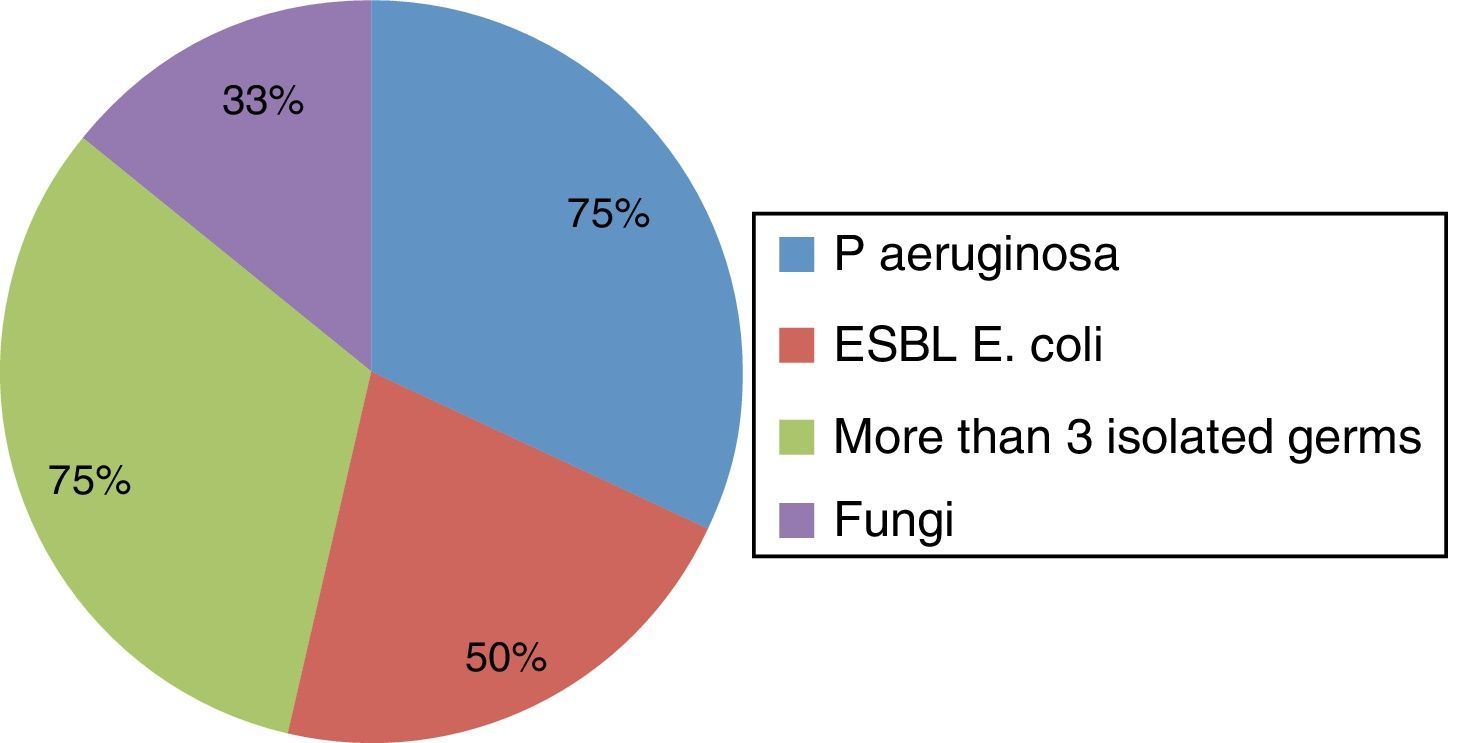
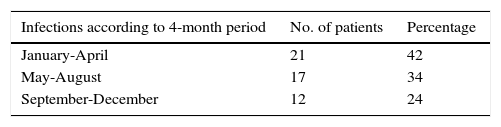
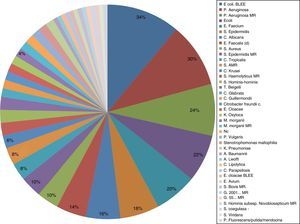
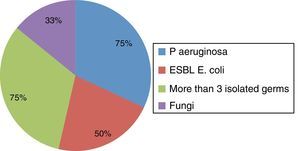
There was a reduction in hospital-acquired infections in 4-month groupings: January-April 42%, May-August 34%, and September-December 24% (Table 3), but with no statistically significant differences. The percentage of surgical site infection was 2.6%, similar to that reported in the literature. The most frequently isolated germs were: extended-spectrum beta-lactamase-producing Escherichia coli (ESBL-producing E. coli), 34%; Pseudomonas aeruginosa (PA), 22%; and multi-drug resistant PA, 12% (Table 3, Fig. 3). The highest percentage of deaths was found in the patients that presented with PA isolation, reaching 75% of the cases, followed by ESBL-producing E. coli in 33%. Likewise, 3 or more germs were isolated in 75% of the cases in the deceased patient group (Fig. 4). Finally, a statistical analysis was carried out to evaluate the association between the management of the surgical patient in the intensive care unit and the development of multi-drug resistant bacterial strains. The Pearson's chi-square test produced statistically significant differences, with a p value of 0.013 and a RR that produced a frequency 2.13-times greater for developing multidrug-resistant germs when the patient was managed in the intensive care unit (95% CI, 1.12-4.04).
Bacteriologic analysis of surgical patients at the HCSAE 2013-2014.
| Infections according to 4-month period | No. of patients | Percentage |
|---|---|---|
| January-April | 21 | 42 |
| May-August | 17 | 34 |
| September-December | 12 | 24 |
| Bacteriologic analysis of the surgical patient | ||
|---|---|---|
| > 3 germs per patient | 21 | 42 |
| Presence of fungi | 11 | 22 |
| 3 or more antimicrobials | 32 | 64 |
| 2 or more MDR germs | 10 | 20 |
| Isolated germ | No. of patients | Percentage |
|---|---|---|
| ESBL-producing E. coli | ||
| Total | 17 | 34 |
| Local | 7 | 14 |
| Referred | 10 | 20 |
| Isolated germ | No. of patients | Percentage |
|---|---|---|
| P. aeruginosa | ||
| Total | 15 | 30 |
| Local | 6 | 12 |
| Referred | 9 | 18 |
| Isolated germ | No. of patients | Percentage |
|---|---|---|
| MDR P. aeruginosaa | ||
| Total | 12 | 24 |
| Local | 2 | 4 |
| Referred | 10 | 20 |
Germs isolated in patients at the General Surgery Service of the HCSAE. The frequency of the isolates at the General Surgery Service within the time frame of January 1, 2013 to December 31, 2014, are summarized in the graph and expressed in percentages. The most prevalent germ was ESBL Escherichia coli.
Source: Electronic case records/ SSS-SIAH- December-2014.
The prevention of surgical site infections is a much-debated medical theme, with a high variability rate, depending on the hospital center evaluated. Even though it is true that the type of prophylaxis depends on the surgical site to be treated, the bacterial resistance rate and the use of antimicrobial agents is different in each center. There are guidelines with recommendations for the most frequent microorganisms according to each likely infection site. And despite the fact that the adequate use of antimicrobial prophylaxis has been shown to importantly reduce morbidity and mortality and the complication rate after a surgical event,2 the truth is that numerous institutions, including ours, do not satisfactorily administer antimicrobials in relation to time or manner.5,6 In our hospital center, prophylactic prescription continues to be inefficient, or incorrectly carried out, whether through poor treatment adherence, absence or shortage of the recommended drug, lack of awareness of its use and action on the part of the physician, and perhaps most frequently, overuse of the agents, either due to habit or imitation.
In spite of the current recommendations, broad-spectrum antimicrobials, such as third generation cephalosporins, continue to be used on a daily basis in our environment, when it has been demonstrated that a single prophylactic dose of a first generation cephalosporin is sufficient in the majority of procedures classified as clean wounds and clean-contaminated wounds. These are low-risk infections,4 which indirectly impacts the bacterial resistance rate. Our review presented a hospital-acquired infection rate of 6.86%, with a 2.6% surgical site infection rate, similar to that reported in the literature.8 When comparing the isolated germs we found that ESBL-producing E. coli, PA, and multidrug-resistant PA increase morbidity and mortality and PA is associated with a high rate of death. Likewise, upon the evaluation of the association between surgical patient management in the intensive care unit and the development of multidrug-resistant bacterial strains, we found a 1.12-4.04 higher risk for developing multidrug resistance when there was an association with intensive care management.5
ConclusionsThe guidelines for antimicrobial prophylaxis in relation to time, form, and the type of antimicrobial agent are not adequately adhered to at our center. There was a statistically significant association between the development of hospital-acquired infections due to multi-drug resistant germs and the admission to the intensive care unit in the surgically treated patient. This was most likely associated with factors such as the type of surgery, patient age, type of wound, a past history of re-intervention, the use of unnecessary or unjustified antimicrobial therapies, and the joint use of numerous broad-spectrum drugs in the intensive care unit and hospital.
There was no statistically significant difference between the recommended prophylaxis and that used at our hospital, but the indiscriminate use of these broad-spectrum antimicrobial agents as prophylaxis favors the presence of multi-drug resistant strains. Therefore it is imperative for adequate adherence to the epidemiologic norms and therapeutic regimens to become part of the standard protocol (to become standardized ??) in the health institutions so that resistance and complications can be reduced and prevented.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that the procedures followed were in accordance with the regulations of the relevant clinical research ethics committee and with those of the Code of Ethics of the World Medical Association (Declaration of Helsinki).
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
FundingNo financial support was received in relation to this study.
Conflict of interestThe authors declare that there is no conflict of interest.
Please cite this article as: Solís-Téllez H, Mondragón-Pinzón EE, Ramírez-Marino M, Espinoza-López FR, Domínguez-Sosa F, Rubio-Suarez JF, et al. Análisis epidemiológico: profilaxis y multirresistencia en cirugía. Revista de Gastroenterología de México. 2017;82:115–122.