The primary aim was to explore the epidemiologic trend of pediatric inflammatory bowel disease in Latin America, and the secondary aims were to obtain an overview of the diagnostic/therapeutic focus of the members of the LASPGHAN and examine the relation of case frequency to year, during the study period.
Materials and methodsLatin American pediatric gastroenterologists participated in an online survey, conducted through the SurveyMonkey platform, that investigated the yearly frequency of new inflammatory bowel disease patients within the time frame of 2005–2016, their disease variety, the gastrointestinal segments affected, and the diagnostic and treatment methods utilized. The correlation of new case frequency with each study year was evaluated.
ResultsA total of 607 patients were studied. The diagnoses were ulcerative colitis in 475 (78.3%) cases, Crohn’s disease in 104 (17.1%), and inflammatory bowel disease D unclassified in 28 (4.6%). The trend in ulcerative colitis was a lineal increase in the frequency of new cases related to each study year, with a significant correlation coefficient. Pancolitis was found in 67.6% of the patients. The diagnostic methods included clinical data, endoscopy, and biopsies in more than 99% of the cases, and imaging studies were indicated selectively. Drug regimens were limited to 5-aminosalicylic acid derivatives, azathioprine, 6-mercaptopurine, infliximab, and adalimumab.
ConclusionsPediatric inflammatory bowel disease in Latin America appears to have increased during the years included in the study period, with a predominance of moderate or severe ulcerative colitis. That lineal trend suggests the predictive likelihood of a gradual increase in the coming years, with possible epidemiologic and clinical implications.
El objetivo primario fue explorar la tendencia epidemiológica de la enfermedad intestinal inflamatoria pediátrica en América Latina; los secundarios, obtener una visión general del enfoque diagnóstico/terapéutico de miembros de la SLAGHNP y explorar la relación entre la frecuencia de casos y los años del período evaluado.
Material y métodosSe realizó una encuesta en línea a pediatras gastroenterólogos de América Latina con la plataforma SurveyMonkey. Se preguntó la frecuencia anual de pacientes nuevos de 2005 a 2016, su variedad, los segmentos del tubo digestivo afectados, los métodos de diagnóstico y el tratamiento utilizado. Se evaluó la correlación entre la frecuencia anual y los años de estudio.
ResultadosSe estudió a 607 pacientes; el diagnóstico de colitis ulcerativa se realizó en 475 (78.3%), de enfermedad de Crohn en 104 (17.1%) y de enfermedad intestinal inflamatoria no clasificable en 28 (4.6%). La tendencia de colitis ulcerativa tuvo un incremento lineal con coeficiente de correlación significativo entre la frecuencia de casos nuevos y el año de estudio; 67.6% tuvieron pancolitis. Los métodos de diagnóstico incluyeron datos clínicos, endoscopia y biopsias en más del 99% de los casos; los estudios de imagen se indicaron de manera selectiva. Los esquemas farmacológicos se circunscribieron a derivados del ácido 5-aminosalicílico, azatioprina, 6-mercaptopurina, infliximab y adalimumab.
ConclusionesLa enfermedad intestinal inflamatoria pediátrica en América Latina parece incrementarse en el período estudiado con predominio de formas moderadas o graves de colitis ulcerativa; esta tendencia lineal puede indicar la posibilidad predictiva de incremento gradual en la próxima década, lo que es probable que tenga implicaciones epidemiológicas y clínicas.
Inflammatory bowel disease (IBD) is characterized by a chronic inflammatory intestinal process associated with genetic factors, environmental triggers, and an aberrant inflammatory response1–2. Its syndromic varieties are ulcerative colitis (UC) and Crohn’s disease (CD). IBD unclassified (IBDU) is a subgroup that cannot be classified as either UC or CD3–5. The incidence of IBD has progressively increased over the last few decades, especially in urban populations of Western countries, with a migratory west-east and north-south trend6–9.
The perception of Latin American pediatric gastroenterologists is that the incidence of IBD has followed a course similar to that of the Western countries in the northern hemisphere, albeit with a delay of several decades. Nevertheless, the published information on the epidemiology of IBD in Latin American children and adolescents is virtually nonexistent10–13. In that context, the primary aim of the present work was to explore the epidemiologic trend of IBD in Latin America and the secondary aims were to evaluate the relation between the frequency of cases and the years included in the study period, thus obtaining a diagnostic and therapeutic overview of pediatric gastroenterologists that belong to the LASPGHAN (Table 1).
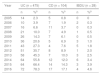
Annual frequency of inflammatory bowel disease from 2005 to 2016 in 607 Latin American pediatric patients treated by members of the Latin American Society for Pediatric Gastroenterology, Hepatology and Nutrition.
| Year | UC (n = 475) | CD (n = 104) | IBDU (n = 28) | |||
|---|---|---|---|---|---|---|
| n | %a | n | %a | n | %a | |
| 2005 | 14 | 2.3 | 5 | 0.8 | 0 | 0 |
| 2006 | 10 | 3.9 | 7 | 1.9 | 2 | 0.3 |
| 2007 | 16 | 6.6 | 11 | 3.7 | 0 | 0.3 |
| 2008 | 21 | 10.0 | 7 | 4.9 | 1 | 0.5 |
| 2009 | 26 | 14.3 | 7 | 6.1 | 0 | 0.5 |
| 2010 | 36 | 20.6 | 5 | 6.9 | 3 | 1.0 |
| 2011 | 43 | 27.3 | 4 | 7.6 | 5 | 1.8 |
| 2012 | 51 | 35.7 | 8 | 8.9 | 1 | 2.0 |
| 2013 | 58 | 45.3 | 7 | 10.0 | 3 | 2.5 |
| 2014 | 64 | 55.8 | 12 | 12.0 | 6 | 3.4 |
| 2015 | 64 | 66.4 | 14 | 14.3 | 3 | 3.9 |
| 2016 | 72 | 78.3 | 17 | 17.1 | 4 | 4.6 |
CD: Crohn’s disease; IBDU: inflammatory bowel disease unclassified; UC: ulcerative colitis.
An ad hoc survey was designed for online application that was sent to active LASPGHAN members in August 2016, November 2016, and June 2017, through the SurveyMonkey platform. The data collected were from the members that answered the survey. No sampling techniques or sample size calculations were carried out. The information requested encompassed the time frame of 2005–2016 and much care was taken to prevent data duplication.
SurveyThe name of the pediatric gastroenterologist surveyed and his/her country of residence were identified. The participants were asked to include patients with IBD from 2 to 16 years of age. The instrument included 14 items, 13 of which were multiple-choice and produced a numeric frequency value. Four of the multiple-choice items also had an open response option. The conceptual content of the survey is in a PDF document as Supplementary material that can be consulted online (Annex 1). The items were inserted into the SurveyMonkey platform and sent to the members of the LASPGHAN by email, together with the invitation to participate in the survey. The results of each survey were imported from the platform page to the Statistical Package for the Social Sciences (SPSS) program for their analysis. Items 2–8 corresponded to the number of news cases of UC, CD, and IBDU treated in each year of the study period. Item 9 dealt with the single or combined diagnostic methods utilized for the diagnosis of IBD (clinical data, endoscopy, biopsy, and imaging studies). The criteria used in making the clinical, endoscopic, and histologic diagnoses of IBD were not included in the survey. Items 10–12 referred to the single or combined medical treatment with intravenous or oral corticosteroids, 5-aminosalisylic acid (5-ASA) derivatives, 6-mercaptopurine (6-MP), infliximab, and adalimumab employed in each of the types of IBD, with an open option for identifying other drugs or biologic agents. Items 13 and 14 corresponded to the gastrointestinal segments affected in the cases diagnosed with UC and CD.
Statistical analysisDescriptive and analytic statistics were performed. Through the linear correlation between each of the study years as an ordinal variable (x) and the number of new cases per each year as a discrete variable (y), the Spearman rho and Kendall tau-b coefficients were analyzed.
ResultsSurveys were received from members from 9 countries (Argentina, Bolivia, Brazil, El Salvador, Mexico, Nicaragua, Peru, Uruguay, and Venezuela). The sample consisted of 607 patients collected from 14 pediatric gastroenterologists: 316 from Argentina, 164 from Mexico, 43 from Uruguay, 33 from Brazil, 20 from Bolivia, 14 from Peru, 10 from Venezuela, 4 from Nicaragua, and 3 from El Salvador. Because Spain and Portugal are member countries of the LASPGHAN, data on 77 patients with IBD were received from the Iberian Peninsula, but they were not included in the analysis, given that Latin America was the selected universe for the survey.
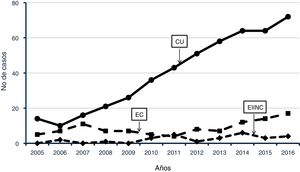
UC was diagnosed in 475 patients (78.3%), CD in 104 (17.1%), and IBDU in 28 (4.6%). The UC:CD ratio was 4.6:1. Within the time frame of the study period, the annual frequency of UC increased 5.1-fold, whereas that of CD increased 3.4-fold. IBDU appeared sporadically from 2005 to 2010 and had slight intermittent increases starting in 2011. Fig. 1 shows the yearly frequency during 2005–2016 of the cases of the IBD varieties analyzed. The percentages are presented as the accumulated percentage per IBD type and year, and the total sample (n = 607) was calculated as a percentage. In the UC group, there was a correlation between the study year and the frequency of cases corresponding to that year, with Spearman rho and Kendall tau-b correlation coefficients of 0.991 (p < 0.001) and 0.962 (p < 0.001), respectively. The R2 values were 0.98 and 0.92. The correlation coefficients of those two tests for the CD group were 0.572 (p = 0.052) and 0.420 (p = 0.067), respectively. The diagnostic methods utilized on the 607 patients evaluated were colonoscopy in all the cases (100%), ileoscopy in 65 (10.7%), and upper endoscopy in 182 (30%). In 603/607 patients (99.3%), multiple biopsies in the segments examined were taken. In 4 cases with endoscopic data consistent with UC, biopsies were not taken, and the diagnostic test was the response to the remission induction drug regimen employed. Imaging studies were performed on 374 patients with UC (78.7%), in 101 with CD (97.1%), and in all the cases of IBDU.
Frequency of ulcerative colitis (UC), Crohn’s disease (CD), and inflammatory bowel disease unclassified (IBDU) in 607 children from 9 Latin American countries treated by members of the LASPGHAN, within the time frame of 2005–2016. UC: correlation coefficients between the study years and case frequency by year, rho = 0.991 (p < 0.001) and r = 0.962 (p < 0.001), Spearman’s correlation, and Kendall tau-b. CD: rho = 0.572 (p = 0.052) and r = 0.420 correlation coefficients (p = 0.067).
In the UC group, 321 (67.6%) of the patients had pancolitis, 86 (18.1%) left-sided colitis, and 68 (14.3%) proctosigmoiditis. In the patients with CD, 62 cases (59.6%) had involvement of the colon, 24 (23.1%) of the rectum and perineum, and 20 (19.2%) of the small bowel. Of the 65 ileoscopies performed, 39 corresponded to patients with CD, and 10 of those cases presented with inflammation of the terminal ileum. In the CD group, upper gastrointestinal tract involvement was identified in 19 patients, but the specific upper gastrointestinal segment involved was not a datum included in the survey items.
In the patients with UC, the number of times oral steroids were indicated was 428 (90.1%), azathioprine 297 (62.5%), 5-ASA derivatives 267 (56.2%), intravenous corticosteroids 190 (40%), infliximab 111 (23.4%), and adalimumab 94 (19.8%). The use of intravenous steroids was followed by oral steroids in 98% of the cases. The trend in the treatment of UC was remission induction with oral or intravenous corticosteroids and maintenance with azathioprine/6-MP. Approximately half of the UC cases also received 5-ASA derivatives.
In patients with CD, drug treatment was oral corticosteroids in 58 (55.8%) cases, 5-ASA derivatives in 46 (44.2%), infliximab in 45 (43.3%), azathioprine in 42 (40.4%), adalimumab in 25 (24%), intravenous corticosteroids in 19 (18%), and 6-MP in 13 (12.5%). Corticosteroids were more frequently used for remission induction in CD than in CU. Azathioprine/6-MP, 5-ASA derivatives, and biologic agents were similarly prescribed for maintenance in the two IBD varieties.
DiscussionThe present study did not have a population design nor was random sampling carried out. The information sent by the pediatric gastroenterologists in relation to the patients treated in their respective countries was retrospectively obtained from their clinical case records or databases, which could imply information bias, and the data analyzed came from only 9 Latin American countries.
Despite those facts, the data presented herein were consistent, in the sense that they suggest the existence of a linear trend of increase in the yearly frequency of UC in the pediatric patients treated by members of the LASPGHAN during the study period. The correlation coefficients and R2 values predispose to the predictive possibility of a gradual increase in IBD, particularly UC, in Latin America in the coming years. Those results may be consequential in relation to epidemiology, clinical training at all healthcare levels, and the planning of research studies.
There are many publications regarding the frequency, prevalence, or incidence of IBD in pediatric patients in North America14–16 and an even greater number in the European Union17–33, as well as studies from the Middle East33,34, Asia35–37, and Oceania38. The data from the majority of those publications point to a progressive increase in the incidence of IBD, especially CD, in children and adolescents.
In Latin America, an increase in the incidence of IBD has been described, mainly in adult populations in Peru, Chile, and Brazil39–41, but information on children and adolescents is scarce10–13. The trend observed in the present survey resembles that of northern countries of the Western world over the past 3 decades. A possible explanation for that trend could be that the collective microbiome of Western population groups has been substantially modified by cultural, social, and dietary changes, establishing differences between the individuals of the developed and developing countries that tend to gradually disappear42. Geography could be another factor involved in the epidemiologic trend, given that a greater frequency of IBD has been related to a higher altitude, lack of sun exposure, and vitamin D deficiency43. The data of the present survey appear to show a reasonable use of endoscopic and histologic studies for achieving a nosologic diagnosis44–45. Imaging studies, particularly those of the upper gastrointestinal tract and the small bowel, were utilized as complements to endoscopy and histology.
The fact that the clinical, endoscopic, and histologic criteria used for making the diagnoses was not covered in the survey was one of its weaknesses. However, there was a high level of use of endoscopy and biopsy, in almost all the cases, and it was assumed that all the survey participants were certified pediatric gastroenterologists in their respective countries and qualified members of the LASPGHAN.
The majority of the pediatric gastroenterologists surveyed had access to the usual drugs, including biologic agents. The trend, with respect to remission and maintenance regimens, was that the traditional regimens based on corticosteroids and thiopurines were more frequently indicated. The more limited use of biologic agents could be due to availability or cost, but those aspects were not included in the survey. Nevertheless, it is known that public health insurance does not cover that type of treatment in some Latin American countries. The high level of use of intravenous or oral corticosteroids, particularly in CD, was striking. That finding should lead to the discussion of reducing corticosteroid prescription and promoting enteral nutrition for remission induction. The prolonged use (more than 12 weeks) of corticosteroids in children with IBD has been associated with a reduction in growth velocity and an excessive increase of adiposity12.
In summary, the results of the present brief survey suggest that IBD in the pediatric populations of some Latin American countries appears to have increased over the past few decades, with a predominance of moderate and severe forms of UC, and is a problem seen in the daily clinical practice of pediatric gastroenterologists.
Financial disclosureNo external financial support was received in relation to this article.
Conflict of interestThe authors declare that there is no conflict of interest.
Ethical considerationsThe authors declare that no experiments were conducted on humans or animals in the present research, and the protocols on the publication of patient data of each work center of the nine participating countries were followed. The collaborating physicians applied the standards, ethics requisites, and informed consent of each country in relation to the diagnosis and management of their patients. Due to the retrospective, multicenter design of the work, informed consent was not required and no personal data that could identify the patients, such as names or initials, were included.
Please cite this article as: Larrosa-Haro A, Abundis-Castro L, Contreras MB, Gallo MJ, Peña-Quintana L, Targa Ferreira CH, et al. Tendencia epidemiológica de la enfermedad intestinal inflamatoria en pacientes pediátricos en América Latina: Grupo de Trabajo en Enfermedad Intestinal Inflamatoria, Sociedad Latinoamericana de Gastroenterología, Hepatología y Nutrición Pediátrica (SLAGHNP). Rev Gastroenterol México. 2020. https://doi.org/10.1016/j.rgmx.2020.07.010