Gastrointestinal angiodysplasias are defined as vascular dilations that communicate capillaries and veins in the walls of the digestive tract. The clinical presentation of these lesions varies from chronic occult bleeding to severe gastrointestinal hemorrhage.
AimThe primary aim of our study was to analyze lesion location, the efficacy of therapeutic endoscopy with argon plasma coagulation, and the factors associated with rebleeding in patients with gastrointestinal angiodysplasias.
Material and methodsA retrospective study of 32,042 endoscopies was carried out within the time frame of January 2012 and December 2013 at our hospital center. Gastrointestinal angiodysplasia was the diagnosis in 331 of the endoscopies. The procedures included upper gastrointestinal endoscopy, colonoscopy, sigmoidoscopy, and enteroscopy.
ResultsThe most frequent location of the angiodysplasias was the cecum (49%), followed by the ascending colon (17%) and the sigmoid colon (16%). They were most frequently found in the duodenum (60%) and gastric body (49%) at upper gastrointestinal endoscopy. Therapeutic endoscopy was performed in 163 cases (49.8%) and the most predominant methods were fulguration with argon (90%) and combination treatment (argon plasma coagulation and injection sclerotherapy) (6.7%).
The macroscopic rebleeding rate after therapeutic endoscopy was 7.4%.
Patients that had rebleeding presented with a lower hemoglobin concentration, higher mean age, and the presence of multiple angiodysplasias at endoscopy (P<.05).
ConclusionsTherapeutic endoscopy was performed in 49.8% of the patients with angiodysplasias. The macroscopic rebleeding rate after treatment was 7.4%. There were statistically significant differences in the patients with rebleeding in relation to mean age, hemoglobin values, and the presence of multiple angiodysplasias.
Las angiodisplasias gastrointestinales se definen como dilataciones vasculares que comunican capilares y venas en las paredes del tracto digestivo. La presentación clínica de estas lesiones varía desde sangrado oculto crónico a hemorragia gastrointestinal grave.
ObjetivoEl objetivo principal de nuestro estudio es analizar la localización, la eficacia de la terapéutica endoscópica con argón y los factores asociados a resangrado en pacientes con angiodisplasias gastrointestinales.
Material y métodosSe estudiaron retrospectivamente 32,042 endoscopias, 331 con diagnóstico de angiodisplasias gastrointestinales, realizadas entre enero de 2012 y diciembre de 2013 en nuestro centro. Se incluyeron endoscopias orales (endoscopias digestivas altas [EDA]) colonoscopias, rectosigmoidoscopias y enteroscopias. Se han evaluado características epidemiológicas, clínicas y analíticas, así como hallazgos y necesidad de tratamiento endoscópico.
ResultadosLa localización más frecuente de las angiodisplasias fue el ciego (49%), seguido de ascendente (17%) y sigma (16%). En las EDA fue más frecuente encontrarlas en duodeno (60%) y cuerpo gástrico (49%). Se realizó tratamiento endoscópico en 163 casos (49.8%), predominantemente fulguración con argón (90%), seguido de tratamiento combinado (argón y esclerosis) (6.7%).
La tasa de resangrado macroscópico tras terapia endoscópica fue del 7.4%.
Los pacientes que resangraron presentaron una concentración de hemoglobina menor, una edad media superior y presencia de múltiples angiodisplasias en endoscopia (p<0.05).
ConclusionesSe realizó terapia endoscópica en el 49.8% de los pacientes con angiodisplasias. La tasa de resangrado macroscópico tras la terapéutica fue del 7.4%. Los pacientes que resangraron presentaron diferencias significativas en cuanto a la edad media, la cifra de hemoglobina y la presencia de múltiples angiodisplasias.
Gastrointestinal angiodysplasias are defined as anomalous vascular dilations that communicate capillaries and veins in the walls of the digestive tract. The clinical presentation of these lesions varies from chronic occult bleeding to severe gastrointestinal hemorrhage.1
Their real prevalence is difficult to establish, but some studies show angiodysplasias to have a prevalence of 0.83% in asymptomatic adults.2 This percentage increases in subjects above 60 years of age and in those that present with established pathologies, such as chronic renal insufficiency, aortic stenosis, or von Willebrand disease.3–5 Angiodysplasias can be found at any point of the gastrointestinal tract. Their most frequent location is the colon, particularly the cecum, in the western countries.6,7
The treatment of these lesions can be medical, endoscopic, or less frequently, surgical. The medical treatments studied include hormone therapy, thalidomide, and the use of somatostatin analogues. These last agents have shown the best results in cases of recurrent gastrointestinal bleeding.8,9 Therapeutic endoscopy can be carried out through argon plasma coagulation, electrocoagulation, photocoagulation, endoscopic clips, or injection sclerotherapy. Surgery is reserved for exceptionally severe cases that require intestinal resection or for patients that need valve replacement due to aortic stenosis (Heyde's syndrome).10–13 Approximately 40-50% of the hemorrhages stop spontaneously, with no need for medical or endoscopic treatment. However, other cases, despite adequate endoscopic treatment, can reach a rebleeding rate of 30-35%.14
The primary aim of our study was to analyze lesion location, the efficacy of therapeutic endoscopy with argon, and the factors associated with rebleeding in patients with gastrointestinal angiodysplasias.
Materials and methodsA retrospective analysis of 32,042 endoscopies performed within the time frame of January 2012 and December 2013 at the Gastroenterology Service of the Hospital Universitario Ramón y Cajal was carried out. Patients diagnosed with angiodysplasia through upper gastrointestinal (UGI) endoscopy, colonoscopy, sigmoidoscopy, or enteroscopy were included in the study.
“Angiodysplasia” was defined as a flat, reddish, vascular lesion with ectatic vascular branches extending from the center of the lesion.15 Therapeutic endoscopy was carried out during the procedures in which angiodysplasias with recent hemorrhage stigmata were observed, or when indicated due to the development of anemia or a previous episode of gastrointestinal bleeding.
“Endoscopic treatment failure” (rebleeding) was considered when another endoscopy was needed due to the suspicion of bleeding or to the development of anemia after the endoscopic treatment of the first episode of bleeding related to the presence of angiodysplasias during the study period.
“Significant anemia” was considered when, according to the attending physician's criterion, there was a considerable decrease in relation to the patient's baseline hemoglobin, with no other acute causes to explain it. Hemoglobin controls were carried out during clinical follow-up testing or as emergency measures when gastrointestinal bleeding was highly suspected.
All information was obtained from the clinical charts and the computerized records of the pharmacy, clinical analysis laboratory, and endoscopy unit. No previous specific calculation of sample size was performed.
The epidemiologic variables (age, sex), clinical variables (treatment with antiaggregant, anticoagulant, or somatostatin analogue agents), and analytical variables (hemoglobin, platelet, and international normalized ratio [INR] values) were collected. Follow-up time was 22 months from the first endoscopy, evaluating whether the patients required repeat endoscopies and the causes thereof.
With respect to the examinations, the total number of endoscopies performed in each patient, the number and location of angiodysplasias found, the presence of bleeding data at the time of examination, and the type of therapy if one was performed, were evaluated. All the patients in whom angiodysplasias were observed at UGI endoscopy had a complete endoscopic study with diagnostic colonoscopy. Capsule endoscopy was not evaluated.
The patients were divided into two groups: those that underwent therapeutic endoscopy for angiodysplasias, and those that did not. The patients treated endoscopically were then further divided into those whose treatment indication was for active bleeding and those whose indication was for chronic anemia.
The statistical analysis was done with the STATA version 13 software. The continuous variables were represented by mean ± standard deviation or by median and range, according to their distribution. The differences between means were analyzed using the bilateral Student's t test and the Mann-Whitney U test. The categorical variables were described through percentages and the significance tests were performed using the chi-square test and the Fisher's exact test.
A logistics regression analysis was carried out to evaluate the factors that significantly contributed to failed therapeutic endoscopy. All the statistically significant variables in the multivariate analysis were included in the regression model. A stratified analysis was employed to detect the possible interaction between variables. The missing data were not taken into account for the analysis.
ResultsOf the 32,041 endoscopies carried out within the study period, angiodysplasia was observed in 331 of them (257 patients). Eighty-three (25%) of the procedures were upper gastrointestinal endoscopies, 241 (73%) were colonoscopies, 6 (1.8%) were sigmoidoscopies, and there was 1 enteroscopy.
The mean age of the patients with angiodysplasias at the time of the examination was 65.7 years (± 22.23) and 59.5% of those patients were men. Sixty-two patients were on antiaggregant therapy (24.12%) and 38 were on oral anticoagulants (14.78%).
Anticoagulation data could not be determined in 5 of the 257 patients.
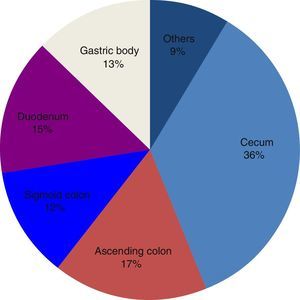
The colon was the most frequent location of the angiodysplasias. The majority of them were found in the cecum (120/241, 49%), followed by the ascending colon (50/241,17%) and the sigmoid colon (39/241, 16%). Thirty-six percent of the total of angiodysplasias found in all the endoscopic studies (331) were located in the cecum.
In the UGI endoscopies, the most frequent locations of angiodysplasias were the duodenum (50/83, 60%) and the gastric body (41/83, 49%). Fifteen percent of the total of angiodysplasias were located in the duodenum. Figure 1 shows the endoscopic characteristics of the total.
Therapeutic endoscopy was performed in 163 cases (48.3%). Forty-six of the cases had upper endoscopy and 117 had colonoscopy. Treatment was predominantly carried out through fulguration with argon (90%), followed by combination treatment (argon plasma coagulation and injection sclerotherapy with 1/10,000 diluted adrenaline) in 6.7% of the cases. Treatment was performed in 13 cases when active bleeding was observed during the examination. It was carried out in 150 cases due to the presence of anemia or a previous episode of gastrointestinal bleeding.
The rate of macroscopic rebleeding after therapeutic endoscopy was 7.4% (12 of 163 patients treated) of the bleeding episodes. Of those 12 patients, 9 had angiodysplasias in the colon, 5 had them in the stomach or duodenum, and 2 patients had them in both locations. Therefore, the rebleeding rate in the angiodysplasias of the colon was 9/117 (7.6%) and in the upper endoscopies was 10.8%.
The patients with rebleeding required a mean of 4.3 ± 3.1 therapeutic endoscopies. Of the 12 patients that had rebleeding, 4 of them needed only 2 therapeutic endoscopies and 4 of the patients required 5 or more.
Five of the 163 treated patients were given somatostatin analogues, with a mean of 5.6 therapeutic endoscopies per patient before beginning treatment. These patients were included in the analysis as part of the rebleeding group, but no specific follow-up data on them was obtained.
In the univariate analysis, comparing the group of patients that presented with rebleeding signs and those that did not, the mean age at the time of endoscopy (80.9 vs 66.64, p < 0.02), anticoagulant treatment (41.7% vs 13.5%, p = 0.02), hemoglobin value (mean 10.13g of Hb vs mean 12.35g of Hb, p = 0.05), and the presence of more than 2 angiodysplasias (78 vs 26%, p = 0. 00001) were different, with statistical significance. The differences between the platelet count, INR value, prescription of anticoagulants, or sex were not statistically significant between the 2 groups (Table 1).
Univariate analysis of factors associated with the rebleeding rate.
| Rebleeding | Cases (n) | Age (years) | HB (g/dl) | PL | INR | ACO | AA | > 2 A |
|---|---|---|---|---|---|---|---|---|
| Yes | 12 | 80.6 | 10.3 | 230197 | 1.18 | 41.7% | 41.7% | 78% |
| No | 163 | 66.4 | 12.3 | 243416 | 1.16 | 13.5% | 24.1% | 26% |
| Contrast hypothesis | p = 0.02 | p = 0.005 | p = 0.62 | p = 0.87 | p = 0.02 | p = 0.18 | p = 0.001 |
AA: antiaggregant: ACO: anticoagulaction; HB: hemoglobin (g/dl); PL: platelets; >2 A: more than two angiodysplasias in the endoscopy
The multivariate analysis carried out through logistic regression showed a statistically significant association of hemoglobin value, age at the time of endoscopy, the presence of more than 2 angiodysplasias, and rebleeding (Table 2).
Multivariate analysis of factors associated with the rebleeding rate Logistic regression.
| Factors associated with rebleeding | p (contrast hypothesis) | 95% confidence interval | Regression coefficient |
|---|---|---|---|
| Age | 0.00 | 0.043 0.135 | 0.089 |
| Location | 0.027 | 0.102 0.167 | 0.0884 |
| Anticoagulation | 0.248 | -0.317 1.23 | 0.456 |
| Hemoglobin | 0.001 | -0.449 - 1.11 | -2.80 |
Logistic regression.
No significant differences were found in the comparison of the rebleeding rate of patients that received treatment due to the presence of active bleeding (23%) and those that received it due to a later development of anemia (14.8%) (p = 0.43).
In regard to the characteristics of the patients that did not receive endoscopic treatment, the mean age was 69.28 years and 59.63% were men. The patients that did not receive endoscopic treatment presented with a higher rebleeding rate than those that received the treatment (p < 0.000). There were differences in age among those that did not receive treatment (69.28 vs 62.5 p = 0.023), but no significant differences with respect to sex, hemoglobin value, or platelets were established. The untreated patients had a higher INR value (1.2 vs 1.1 p = 0.03).
DiscussionGastrointestinal angiodysplasias are the most frequent vascular malformation located in the digestive tract. Our case series collected data from 331 endoscopies with angiodysplasia diagnosis that were performed within the time frame of January 2012 and December 2013. Our data coincides with that found in the previous literature,6 describing the cecum as the most frequent location, followed by the ascending colon and the sigmoid colon. The angiodysplasias found through upper endoscopy were more commonly situated in the duodenum or the gastric body.
The clinical symptoms that can present with this pathology vary from marked macroscopic gastrointestinal bleeding, to occult bleeding that manifests as chronic anemia,16 and can be treated medically and endoscopically. Therapeutic endoscopy is currently the first-line treatment and is indicated when the cause of bleeding or the development of anemia is attributed to angiodysplasias.
The most widely used method is argon plasma coagulation, which simultaneously releases electric current and argon gas. Several studies have evaluated the mid and long-term efficacy of this method. In our case series (331 endoscopies with angiodysplasia diagnosis) in which the predominant endoscopic treatment of 163 cases was argon plasma electrocoagulation (90%), followed by the combination treatment of argon plasma coagulation-injection sclerotherapy (6.7%), there was a macroscopic rebleeding rate of 7.4%. These results are similar to those of previously published studies. A retrospective analysis from 2006 that included 100 patients with angiodysplasias of the colon had a rebleeding rate of 2-10% (at 1 and 2 years, respectively).17 Another retrospective study by Kwan et al.18 on 100 patients showed similar rebleeding figures of 16%. In contrast, other studies have reported higher figures. In 1985, a study by Rutgeers19 on 59 patients with gastric and colonic angiodysplasias had rebleeding rates after argon plasma coagulation of 30%. In 1995, Gupta et al.20 also described a similar figure (30%) in a study on 33 patients with colonic and small bowel angiodysplasias that were followed for a 13.5-month period. A recent meta-analysis described the success of short-term endoscopic treatment, but with rebleeding rates around 36% in a period of 22 months.14 However, it included several studies in which only small bowel angiodysplasias were treated, and they had higher rebleeding rates.
The follow-up period in those studies was similar (between 1 and 2 years in the majority of the cases) and, in this respect, the data are similar to those of our patients that were followed for 22 months. The lower rebleeding rate in our case series is most likely due to its retrospective design, given that there could have been losses or unexplained reasons for which other endoscopies were not carried out in patients that could have had later rebleeding. In addition, even though our rebleeding rate figures are striking in regard to those published in the 2014 meta-analysis, many of those studies had small sample sizes and the patients had small bowel angiodysplasias, whereas our patients mainly presented with angiodysplasias in the colon. There were no statistically significant differences in the rebleeding rate comparison after treatment among the patients that presented with active bleeding or chronic anemia, despite having clearly observed a greater trend toward bleeding in the patients with active hemorrhage. One of the explanations of this finding could be the small number of patients with active bleeding data included in the study.
There have not been many studies on the efficacy of therapeutic endoscopy in angiodysplasias of the upper gastrointestinal tract, but some have shown that treatment with argon plasma coagulation is efficacious. Our data included UGI endoscopies (95) and colonoscopies (235) for the treatment of angiodysplasias. Of the 95 upper endoscopies performed, 46 were therapeutic. Rebleeding presented in 5 of those patients, that is to say, 10.8%. This figure is similar to that presented in the 2012 retrospective case series by Chiu et al.21 that reported on 27 patients with gastric or duodenal angiodysplasias treated with argon plasma coagulation. They considered rebleeding the presence of new macroscopic bleeding or the drop in hemoglobin values after therapeutic endoscopy. The rebleeding rate was 7.4%.
As expected, we found that the rebleeding rate in the group of untreated patients was significantly higher that in the treatment group. Likewise, we observed a trend to not perform treatment in older patients with a higher INR. This could be because, in the opinion of the endoscopist performing the examination, the untreated patients were at greater risk or had a lower probability of benefitting from treatment at the time of the endoscopy. In this respect, the 2009 study by Saperas et al.22 also found that patients treated with argon plasma coagulation presented with approximately half the risk for recurrence.
Somatostatin analogues have been described as beneficial treatment in patients with bleeding recurrence secondary to angiodysplasias after therapeutic endoscopy, reducing the bleeding episodes and the need for transfusions.23 Only 5 of our patients were treated with this drug. We did not obtain specific follow-up data on those patients, given that it was not contemplated in the study aims and the number of patients was very small. Given that the patients had a mean of 5.6 therapeutic endoscopies before beginning treatment, we did not feel that this datum significantly influenced our results on the efficacy of therapeutic endoscopy.
Many factors associated with a higher risk for rebleeding in patients such as ours have been described in the literature and the results of the different studies vary greatly. One retrospective study published in 2009 that included 62 patients identified anticoagulant treatment and a higher number of lesions seen at endoscopy as associated factors.22 The 2006 study by Kwan et al.18 mentioned above included 100 patients with angiodysplasias of the colon and the only factor statistically associated with rebleeding was the presence of multiple (> 3) angiodysplasias at endoscopy. In the univariate analysis in our study, the factors associated with rebleeding that were statistically significant were low levels of hemoglobin at the time of the endoscopy, advanced age, receiving anticoagulant treatment, and the presence of more than 2 angiodysplasias. Only age, hemoglobin value, and multiple angiodysplasias were confirmed. Low hemoglobin levels at endoscopy could reflect more severe bleeding, according to the 2009 study by Saperas et al.22 Alterations in the analytic parameters of coagulation and the number of angiodysplasias also coincided with previously published reports. Likewise, other factors that could be associated were analyzed, such as antiaggregant treatment, platelet level, INR, or sex, but they were not statistically significant. The lack of significance in relation to antiaggregant treatment could be due to the fact that the number of patients with rebleeding that were treated with those drugs was insufficient for detecting differences. The identification of factors that predispose to a higher rebleeding rate could be of help in clinical practice when deciding on medical or endoscopic treatment and their follow-up.
The main limitations of our study in relation to follow-up and data analysis of the patients are due to its retrospective design, which made it impossible during the follow-up to know why other endoscopies were not performed after initial treatment in patients considered not to have presented with new bleeding. The rebleeding rate in other previous studies is much higher. This may be due to the fact that in our study we only took into account the cases of rebleeding that required a new endoscopy, the data were collected with respect to the need for colonic surgery or aortic valve replacement (very severe bleeding) or only the development of anemia (milder bleeding), and that our study had a short follow-up period. The retrospective design prevented us from knowing the exact iron therapy regimen utilized in those patients, which could affect the findings, so we did not include it in the analysis. Finally, there is no information on the grade of colonic clearance (important in angiodysplasia detection) and the examinations were performed by different endoscopists with distinct levels of experience, which can also influence the detection rate and quality of the therapeutic endoscopy applied. Our case series had a higher number of patients than other studies, but the sample size was not specifically calculated beforehand.
In conclusion, the overall macroscopic rebleeding rate was 7.4% and the factors associated with rebleeding were older patient age, lower hemoglobin level, and the presence of multiple angiodysplasias.
Ethical responsibilitiesProtection of persons and animalsThe authors declare that no experiments were performed on humans or animals for this study.
Data confidentialityThe authors declare that they have followed the protocols of their work center in relation to the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Financial disclosureThe present study did not require specific funding. No financial support was received in relation to this article.
Conflict of interestThe authors declare that there is no conflict of interest.
Please cite this article as: Arribas Anta J, Zaera de la Fuente C, Martín Mateos R, González Martín JA, Cañete Ruiz A, Boixeda de Miquel D, et al. Evaluación de la eficacia terapéutica endoscópica en hemorragia digestiva secundaria a angiodisplasias. Revista de Gastroenterología de México. 2017;82:26–31.