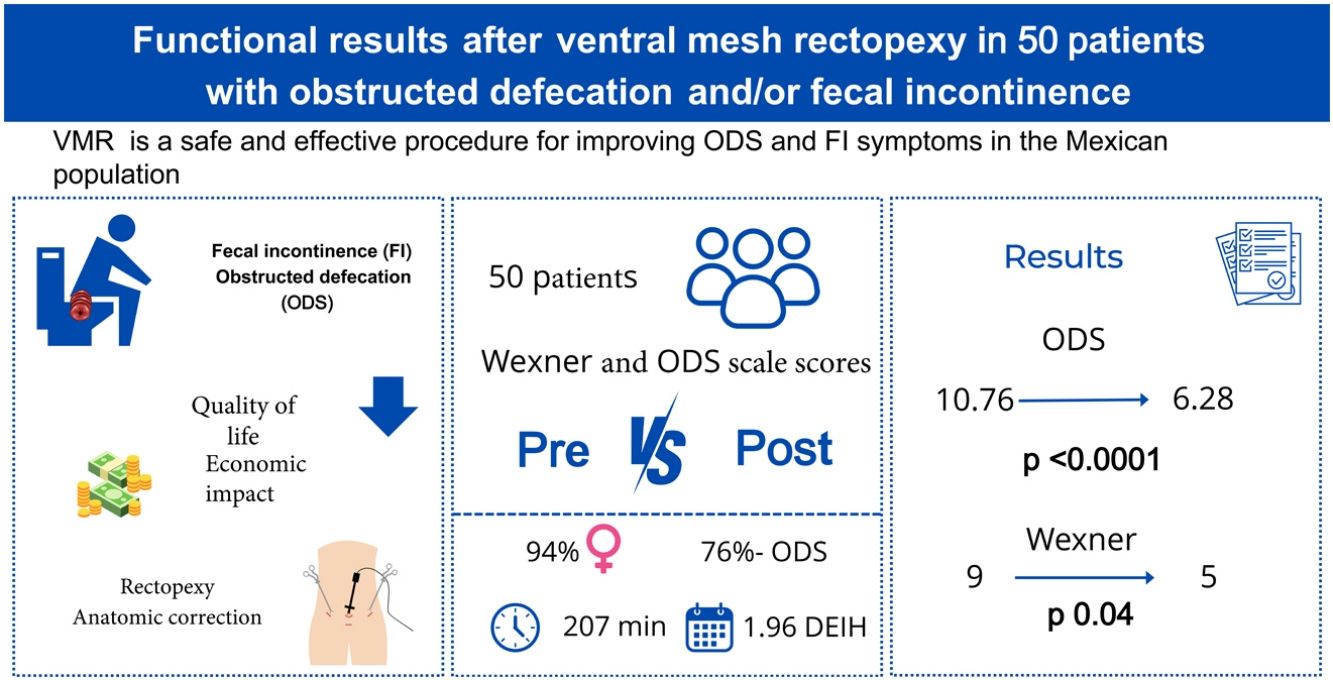
Ventral mesh rectopexy (VMR) for correcting rectal prolapse, rectocele, and enterocele improves obstructed defecation syndrome (ODS) and fecal incontinence (FI). This procedure is popular due to its minimally invasive approach and favorable clinical outcomes. Our aim was to evaluate the clinical response of patients that underwent VMR, focusing on changes in the ODS and FI scores.
Material and methodsA retrospective, observational, cohort study was conducted on patients that underwent VMR within the time frame of May 2019 and May 2024 at a high-volume hospital. Fifty case records were analyzed, measuring the changes in the scores of the ODS scale and CCF-FIS, before and after surgery. Statistical significance was set at a p < 0.05.
ResultsThe ODS scores decreased from 10.76 to 6.28 and the FI scores from 9 to 5, showing significant improvement. When analyzing individual items of each of the scales separately, all in the ODS scale were statistically significant, whereas in the FI scale, only pad use and impact on social life were significant. There were no major intraoperative complications or conversions to open surgery and the mean hospital stay was1.96 days. No significant differences in outcomes were found between the conventional and robotic laparoscopic approaches.
ConclusionsVMR is a safe and effective procedure for improving ODS and FI symptoms in the Mexican population. Long-term follow-up is required to confirm the persistence of benefits and evaluate late complications.
La rectopexia ventral con malla (RVM), utilizado para corregir el prolapso rectal, rectocele y enterocele, mejora los síntomas de obstrucción defecatoria (ODS) e incontinencia fecal (IF). Este procedimiento ha ganado popularidad debida a su enfoque mínimamente invasivo y a sus buenos resultados clínicos. En el presente estudio, se evaluó la respuesta clínica de la RVM centrándose en los cambios en los puntajes de ODS e IF.
Material y métodosSe realizó un estudio de tipo cohorte observacional retrospectivo en pacientes sometidos a RVM entre el 2019 y mayo del 2024 en un hospital de alto volumen. Se analizaron un total de 50 expedientes; midiendo los cambios en los puntajes de las escalas de ODS y CCF-FIS antes y después de la cirugía. Se consideró significativa una p < 0.05.
ResultadosLos puntajes de ODS disminuyeron de 10.76 a 6.28, y los de IF de 9 a 5, mostrando mejoría significativa. Al analizar los incisos de cada una de las escalas de forma separada, todos fueron estadísticamente significativo en ODS, mientras que el IF, solo el uso de apósito y la afectación de la vida social. No hubo complicaciones intraoperatorias mayores ni conversiones a cirugía abierta, con una estancia promedio de 1.96 días. No se encontraron diferencias significativas en los resultados entre los abordajes laparoscópicos convencionales y robóticos.
ConclusionesLa RVM es un procedimiento efectivo y seguro para mejorar los síntomas de ODS e IF en la población mexicana. Se requiere de un seguimiento a largo plazo para confirmar la persistencia de los beneficios observados y evaluar complicaciones tardías.
Ventral mesh rectopexy (VMR) is a widely utilized procedure for resolving symptoms associated with pelvic floor dysfunction, specifically rectal prolapse, rectocele, and enterocele, which form part of pelvic organ prolapse (POP).
The exact prevalence of POP is difficult to establish. Studies report that approximately 50% of women who have given birth present with POP.1 Six percent of women between 20 and 29 years of age have symptomatic POP, as do 50% of women above eighty years of age.2 Eleven percent of women older than 80 years are calculated to have undergone a procedure due to POP.3
The most frequent manifestations of rectocele and enterocele are the sensation of a foreign body at the level of the vagina, obstructed defecation syndrome (ODS), and fecal incontinence (FI), whereas rectal prolapse presents as the sensation of a foreign body at the level of the anus, FI, and ODS.4–6
FI has a crucial social and economic impact and significantly affects quality of life.7 There are several widely recognized risk factors for FI and the most important are advanced age, female sex, and multiparity.8
There are several FI severity scales that are useful in its evaluation, and the most widely used is the Cleveland Clinic Florida-Fecal Incontinence Score (CCF-FIS), also known as the Wexler scale9 (Table 1), which has a minimum score of 0 and a maximum score of 20, which signifies total incontinence.10
Cleveland Clinic Florida Fecal Incontinence Score (CCF-FIS) (Wexner scale).
| Type of leak | Never | Rarely(< 1/month) | Sometimes(> 1/month and < 1/week) | Generally(> 1/week and < 1/day) | Always(> 1/day) |
|---|---|---|---|---|---|
| Solid | 0 | 1 | 2 | 3 | 4 |
| Liquid | 0 | 1 | 2 | 3 | 4 |
| Gas | 0 | 1 | 2 | 3 | 4 |
| Pad/sanitary napkin use | 0 | 1 | 2 | 3 | 4 |
| Lifestyle alteration | 0 | 1 | 2 | 3 | 4 |
ODS is one of the most frequent causes of constipation. It may result from functional questions, whether dyssynergic defecation or paradoxical puborectal muscle contraction,11 or from anatomic alterations, such as rectocele, enterocele, or rectal prolapse.12
As in FI, there are different scales for evaluating ODS that aid us in assessing the response of the treatment provided. The most widely utilized scale is the ODS score because it is consistent, validated, reproducible, and easy to apply13 (Table 2). Like the CCF-FIS, its score is from 0 to 20.
Obstructed Defecation Syndrome (ODS) scale.
| Symptoms or variables | Never | Rarely(< 1/month) | Sometimes(> 1/month and < 1/week) | Generally(> 1/week and < 1/day) | Always(> 1/day) |
|---|---|---|---|---|---|
| Excessive straining | 0 | 1 | 2 | 3 | 4 |
| Incomplete bowel movement | 0 | 1 | 2 | 3 | 4 |
| Enema or laxative use | 0 | 1 | 2 | 3 | 4 |
| Digitalization or perineal pressure | 0 | 1 | 2 | 3 | 4 |
| Abdominal discomfort | 0 | 1 | 2 | 3 | 4 |
D’Hoore et al. were the first to describe VMR for rectal prolapse in 2004.14,15 Since then, the technique has been broadly adopted, becoming the procedure of choice in rectal prolapse and rectocele.16,17 VMR returns the rectum to its anatomic position.
Numerous studies18–21 have evaluated the functional results after VMR performed laparoscopically and robotically, but never on a Mexican population. Most of those studies report significant improvement in incontinence and obstructed defecation, with a statistically significant decrease, according to the scales utilized.18 They also describe no major complications, conversions to open surgery, and a low recurrence rate.14,18,19
The aim of the present study was to evaluate and compare the functional results after VMR in patients who presented with rectal prolapse or rectocele, with ODS and/or FI measured using the ODS scale and CCF-FIS.
Materials and methodsA retrospective, descriptive, observational cohort study was conducted. A total of 140 cases of patients diagnosed with rectal prolapse or rectocele, who had ODS and/or FI and underwent VMR, were analyzed. Of those cases, 5 were lost to follow-up and 85 had incomplete clinical records because they did not include the corresponding scale results.
Demographic and surgical data were analyzed, along with the preoperative and postoperative scores of the abovementioned scales.
Statistical analysisFor the statistical analysis, the qualitative data were expressed as frequency and percentage, and as mean and standard deviation or median and interquartile range, according to distribution determined through the Kolmogorov-Smirnov test.
The preoperative and postoperative comparisons were made using the paired t test for parametric distributions and the Wilcoxon test for nonparametric distributions.
The least squares method was carried out to create the linear models and compare the preoperative and postoperative changes in the scales. Stratified analyses were performed for the type of surgery and the presence or absence of dyssynergic defecation, as well as a sensitivity analysis for patients with previous FI.
All tests were two-tailed and statistical significance was set at a p < 0.05.
SAS® OnDemand for Academics software was utilized for the statistical analysis of the data.
Ethical considerationsInformed consent was obtained from the patients for receiving the treatment described in this study. In addition, the research met the current bioethical regulations and was approved by the Research Committee of the Hospital Central Militar. This article contains no personal information that could identify patients.
ResultsTable 3 describes the demographic characteristics of the study patients.
Of the patient total, 38 (76%) had at least one previous delivery, 16 of which had a complication, including tears, macrosomic products, and prolonged labor. Importantly, preoperative manometry was performed on 58% of the patients with obstructed defecation, 9 of whom presented with dyssynergic defecation.
Most of the procedures (76%, 38 patients) were performed due to obstructed defecation. Seven patients had concomitant incontinence. The procedure was carried out in 13 patients due to FI and in 12 patients due to rectal prolapse.
Twenty-nine conventional laparoscopic procedures and 21 robotic-assisted laparoscopic procedures were performed. Mean surgery duration was 207 min, and bleeding was registered at a mean of 16 ml. There were no conversions or intraoperative complications but a case of mesh detachment the same day of the surgery was recorded. Mean postoperative hospital stay was 1.96 days, with a range of 1 to 4 days.
Functional results were evaluated utilizing the scores of the ODS scale and the CCF-FIS (also known as the Wexner score). The first score was registered the day of the surgery and the follow-up score at a mean of 22.5 months (range of 3-60 months).
The ODS score showed significant improvement, going from a mean preoperative score of 10.76 (4.32 SD) to a mean postoperative score of 6.28, with a statistically significant p < 0.0001. When breaking down the scores by specific items, there was improvement in all of them. Straining decreased by 2 points, incomplete bowel movement sensation by 1 point, laxative use by 2 points, and abdominal discomfort by 1.5 points, all of which were statistically significant (Table 4).
Preoperative and postoperative comparison of the Obstructed Defecation Syndrome (ODS) scores.
| Variable | Preoperative | Postoperative | p |
|---|---|---|---|
| Overall score | 10.76 (4.31) | 6.28 (4.43) | <0.0001 |
| Excessive straining | 4 (2-4) | 2 (0-3) | <0.0001 |
| Incomplete bowel movement | 3 (1-4) | 2 (0-3) | 0.005 |
| Pad or laxative use | 3 (1-4) | 1 (0-3) | 0.002 |
| Digitalization | 1 (1-4) | 0 (0-2) | 0.002 |
| Abdominal discomfort | 3 (2-4) | 1.5 (0-3) | 0.0007 |
A separate analysis was carried out on the 9 patients with the manometric diagnosis of dyssynergic defecation, and their results were comparable to those of the general study population. Of those patients, 4 received preoperative or postoperative pelvic floor rehabilitation.
Regarding the Wexner scale (CCF-FIS), the mean preoperative score was 9 points, and the mean postoperative score was 5 points. However, when analyzing the items individually, only pad use and lifestyle alteration were statistically significant (Table 5).
Changes in the preoperative and postoperative Cleveland Clinic Florida-Fecal Incontinence scale (CCF-FIS) scores.
| Variable | Preoperative | Postoperative | p |
|---|---|---|---|
| Overall score | 9 (2-11) | 5 (1-9) | 0.04 |
| Solid | 2 (0-4) | 2 (0-3) | 0.14 |
| Liquid | 0 (0-2) | 1 (0-2) | 0.24 |
| Gas | 0 (0-2) | 0 (0-2) | 0.57 |
| Pad/sanitary napkin use | 0 (0-1) | 0 | 0.04 |
| Lifestyle alteration | 1 (0-4) | 0 (0-3) | 0.02 |
In the functional outcome comparison, according to surgical approach, we found that the results of conventional laparoscopy were similar to those of the general study population (Tables 6 and 7). In contrast, robotic-assisted surgery showed no significant differences in any of the CCF-FIS items (Tables 8 and 9).
Changes in the preoperative and postoperative ODS scores in patients who underwent conventional laparoscopy.
| Variable | Preoperative | Postoperative | p |
|---|---|---|---|
| Overall score | 10.75 (4.7) | 6.28 (4.4) | <0.001 |
| Excessive pushing | 4 (2-4) | 2 (0-3) | <0.0001 |
| Incomplete bowel movement | 3 (1-4) | 2 (0-3) | 0.0062 |
| Enema or laxative use | 3 (0-4) | 1 (0-3) | 0.0081 |
| Digitalization | 1 (1-4) | 0 (0-2) | 0.002 |
| Abdominal discomfort | 3 (2-4) | 1.5 (0-3) | 0.0008 |
Changes in the preoperative and postoperative Wexner scale scores in patients who underwent conventional laparoscopy.
| Variable | Preoperative | Postoperative | p |
|---|---|---|---|
| Overall score | 10 (4-11) | 5 (1-9) | 0.005 |
| Solid | 2 (0-4) | 2 (0-3) | 0.05 |
| Liquid | 1.5 (0-2.5) | 1 (0-2) | 0.09 |
| Gas | 1 (0-2) | 0 (0-2) | 0.14 |
| Pad/sanitary napkin use | 0 (0-1) | 0 | 0.06 |
| Lifestyle alteration | 4 (0-4) | 0 (0-3) | 0.004 |
Changes in the preoperative and postoperative ODS scale scores in patients who underwent robotic-assisted laparoscopic interventions.
| Variable | Preoperative | Postoperative | p |
|---|---|---|---|
| Overall score | 10.8 (3.6) | 6.3 (4.42) | 0.03 |
| Excessive pushing | 4 (3-4) | 5 (1-9) | 0.0007 |
| Incomplete bowel movement | 3 (1-4) | 2 (0-3) | 0.03 |
| Enema or laxative use | 3 (2-4) | 1 (0-3) | 0.003 |
| Digitalization | 1 (1-4) | 0 (0-2) | 0.002 |
| ODS abdominal discomfort | 3 (2-4) | 1.5 (0-3) | 0.014 |
Changes in the preoperative and postoperative Wexner scale scores in patients who underwent robotic-assisted laparoscopic interventions.
| Variable | Preoperative | Postoperative | p |
|---|---|---|---|
| Overall score | 4 (0-11) | 6 (2-9) | 0.38 |
| Solid | 2 (0-3) | 2 (0-3) | 0.29 |
| Liquid | 1 (0-2) | 1 (0-2) | 0.36 |
| Gas | 0 (0-2) | 0 (0-2) | 0.31 |
| Pad/sanitary napkin use | 0 (0-1) | 0 | 0.06 |
| Lifestyle alteration | 0 (0-3) | 0 (0-3) | 0.47 |
The goal of surgical correction of rectal prolapse and symptomatic rectocele is not only to restore the anatomy but also to recover function. Currently, VMR is considered the procedure of choice due to the low recurrence rate and better functional results reported.22 Numerous studies have shown that that ODS and FI improve with VMR, but those benefits have not been confirmed in Mexican or Latin American populations.
The data obtained in the present study revealed significant improvement in ODS, concurring with reports in the international literature.
When the patients with ODS and dyssynergic defecation diagnosed through manometry were individually analyzed, there was statistically significant improvement in the ODS score in both the total score and in each item when evaluated separately. No studies with comparable results were identified in a review of the available literature. Notably, dyssynergic defecation has only been evaluated in the context of the Delorme procedure, in which no clinical improvement was reported.23
The improvement observed in our study may be inferred to be related to preoperative or postoperative rehabilitation, but in the review of the clinical records, only 4 of the 9 patients went to rehabilitation sessions, and 3 of them did so in the preoperative period. Thus, it may be assumed that, in those cases, the predominant component of obstructed defecation was anatomic rather than functional, which explains the improvement seen in the patients. However, the subsequent performance of a manometric control would be essential for determining if there was improved function.
Regarding the evaluation of preoperative and postoperative FI improvement, there was a decrease in the score from 9 to 5 points. However, when analyzing the items individually, the difference was not significant in relation to the involuntary leakage of solid or liquid stools or gas (incontinence). Similar results were reported in the studies by Solari et al.24 and Kremel et al.25 It could be supposed that incontinence was not resolved through VMR in those patients due to there being a different pathophysiology, such as sphincter hypotonia, but the low percentage of patients who underwent a previous manometric evaluation makes that impossible to confirm.
In the comparison of the robotic-assisted and conventional laparoscopies, their results were similar, except in the difference in the Wexner score, which was not significant in the robotic procedures. That is inconsistent with reports in the international literature, in which there was no difference between the two approaches.26,27
A distinction was made between anatomic and functional recurrence. Of the 4 patients with recurrence, 2 were cases of recurrent complete rectal prolapse and two were recurrent rectocele with ODS. One of the cases of recurrent rectocele was immediate, due to detachment of the mesh from coughing. The other 3 patients had anatomic (clinically) and symptomatic improvement, with recurrence at 2-3 years. In the patients with full-thickness rectal prolapse, 14.2% (2 out of 14 patients) had recurrence, one of whom had undergone previous surgery for prolapse, with a perineal approach. This was a higher rate than the 8% reported in the literature.28,29 However, in studies evaluating prolapse in the posterior compartment, including rectocele, recurrence was 11.7%.30
In the systematic review and meta-analysis conducted by Emile et al. in 2019, there was a 12.4% complication rate. The most frequent were urinary complications, with the presence of postoperative urinary tract infections, urinary retention, ureteral injury, and bladder injury,31 none of which were present in our study.
The most dreaded complications are those related to the mesh in the pelvic hollow. In a study by Evans et al., more than 2,000 postoperative patients who underwent VMR were analyzed. Mesh-related complications were reported in 2%. Upon analyzing the patients in whom a polypropylene mesh (the same material used in our study) was used, there was a 1.7% frequency of mesh erosion.32 In another meta-analysis carried out by Emile et al., there was a mesh-related complication rate of 0.96%.31 There were no mesh-related complications in our study patients but our follow-up was short-term.
Few studies evaluate the predictors of VMR failure.24,25,30 In a study that included 61 patients who underwent VMR, most diagnosed with ODS, the risk factors identified for symptom persistence were grade of prolapse, presence of dolichocolon, and pre-existing constipation. However, that study had a maximum follow-up period of four years.24 Regarding the prediction of recurrence in full-thickness rectal prolapse, prolonged terminal motor latency of the pudendal nerve has been pointed out as a risk factor,30 which in most cases are pudendal nerve lesions secondary to a prolonged vaginal delivery.33 Nevertheless, in a study by Kremel et al., they reported that the obstetric history was not a risk factor for recurrence following VMR.25 In addition, numerous studies have coincided on male sex being an important risk factor for recurrence. This is due to the surgical technical difficulty in men because of the android pelvis, the difficulty in dissecting the prostatic rectus plane and the vesical rectus plane, and autonomic nerve injury that can result in sexual dysfunction.31
LimitationsOur study had several limitations. Functional results can vary over time, thus a single measurement may not adequately reflect those changes; our sample size was relatively small, given the low response rate of the scales utilized, signifying that our results cannot be generalized; and importantly, we had no systematized follow-up.
The patients were analyzed assuming that anatomic defects were surgically corrected, based only on clinical follow-up. However, a more thorough follow-up that includes objective anatomic and functional evaluations, such as defecography or anorectal manometries, is recommended. This would enable anatomic corrections to be compared with the symptomatic improvement measured through the scales utilized. Likewise, measuring health-related changes in quality of life, employing the appropriate scales, such as the SF-12, would be useful.
ConclusionsVMR is an adequate treatment for patients with ODS and/or FI and showed significant improvement measured by the CCF-FIS and the ODS scoring scales.
Financial disclosureNo financial support was received in relation to this study/article.
The authors declare that there is no conflict of interest.