Gallstone ileus represents 4% of the causes of bowel obstruction in the general population, but increases to 25% in patients above the age of 65 years. Gallstone ileus does not present with unique symptoms, making diagnosis difficult. Its management is surgical, but there is no consensus as to which of the different surgical techniques is the procedure of choice. At present, there is no recent review of this pathology.
AimTo conduct an up-to-date review of this disease.
Materials and methodsArticles published within the time frame of 2000 to 2014 were found utilizing the PUBMED, EMBASE, and Cochrane Library search engines with the terms “gallstone ileus” plus “review” and the following filters: “review”, “full text”, and “humans”.
ResultsThe results of this review showed that gallstone ileus etiology was due to intestinal obstruction from a gallstone that migrated into the intestinal lumen through a bilioenteric fistula. The presence of 2 of the 3 Rigler's triad signs was considered diagnostic. Abdominal tomography was the imaging study of choice for gallstone ileus diagnosis and the surgical procedures for management were enterolithotomy, one-stage surgery, and two-stage surgery. Enterolithotomy had lower morbidity and mortality than the other 2 procedures.
ConclusionsThe aim of gallstone ileus treatment is to release the obstruction, which is done through enterolithotomy. It is the recommended technique for gallstone ileus management because of its lower morbidity and mortality, compared with the other techniques.
El íleo biliar representa el 4% de las causas de obstrucción intestinal en la población general, pero incrementa a un 25% en los pacientes mayores a los 65 años de edad. El íleo biliar no presenta síntomas únicos, haciendo difícil su diagnóstico. Su manejo es quirúrgico, pero no hay consenso sobre cuál de las diferentes técnicas quirúrgicas es el procedimiento de elección. Actualmente, no hay una revisión reciente de esta patología.
ObjetivoLlevar a cabo una revisión actualizada de esta enfermedad.
Materiales y métodosLos artículos publicados dentro del periodo 2000-2014 se encontraron utilizando los motores de búsqueda PUBMED, EMBASE, y la Cochrane Library utilizando los términos «gallstone ileus» más «review» y los siguientes filtros fueron empleados: «review», «full text», y «humans».
ResultadosLos resultados de esta revisión mostraron que la etiología del íleo biliar se debió a la obstrucción intestinal ocasionada por un cálculo biliar que migró hacia el lumen intestinal a través de una fístula enterobiliar. La presencia de 2 de los 3 signos de la tríada de Rigler se consideró al momento de diagnóstico. La tomografía abdominal fue el estudio de elección para el diagnóstico del íleo biliar y los procedimientos quirúrgicos para su manejo fueron la enterolitotomía, la cirugía en un solo tiempo, y la cirugía en dos tiempos. La enterolitotomía tenía una morbimortalidad menor que los otros dos procedimientos.
ConclusionesEl objetivo del tratamiento del íleo biliar es liberar la obstrucción, obtenido a través de la enterolitotomía. Esta es la técnica recomendada para el manejo del íleo biliar debido a su morbimortalidad menor, comparada con las otras técnicas.
Gallstone ileus (GI) is an uncommon complication of cholelithiasis, described as a mechanical intestinal obstruction due to the impaction of one or more large gallstones within the gastrointestinal tract. It is caused by the passing of a gallstone from the bile ducts into the intestinal lumen through a fistula.1,2 The most frequent type of fistula is located between the gallbladder and the duodenum.2 Once the stone is in the intestinal lumen, it can obstruct any part of the gastrointestinal tract, but the most common place is the distal ileum.3 The gallstone ileus-associated mortality rate ranges from 12 to 27%, and the morbidity rate reaches 50%,4 due to the advanced age of the patients, the associated pathologies (usually severe), late hospital admission, and to delayed therapeutic treatment.5 GI represents 0.3-0.5% of the complications of gallstone disease,5 signifying 30-35 cases per million hospitalizations. It is more prevalent in women, with a female to male ratio of 3.5-3.6:1, and the patients are usually older than 65 years of age.1,4 As a significant clinical antecedent, only about 50% of these patients have a previous history of gallbladder disease.6 It is important to keep in mind that GI is the cause of small bowel obstruction in fewer than 4% of patients under 65 years of age, but rises to 25% in patients above 65 years of age.7
Given that gallstone ileus is a rare disease, but one that has a high risk of death, we decided to carry out an up-to-date review of the topic to bring new evidence to light on its pathophysiology, diagnostic approach, and treatment options.
Materials and methodsWe conducted an electronic search of PUBMED, EMBASE, and the Cochrane Library on articles published from January 2000 to December 2014, using the keywords “gallstone ileus” plus “review” and the following filters: “review”, “full text”, and “humans”. We examined the abstracts for relevance to the topic, obtaining the appropriate full texts. After going over the reference lists of all the full-text articles, we carried out a manual search, identifying and collecting new items. A total of 30 manuscripts were selected for the final analysis.
The aim of the study was to provide current information on GI disease, according to recent publications. To accomplish this, we reviewed each article, looking for the description of the condition under the following topics: incidence, pathophysiology, diagnostic approach, treatment options, and outcomes.
PathophysiologyGallstone ileus occurs when a gallstone passes into the gastrointestinal tract through a bilioenteric fistula. The fistula appears when there are recurrent episodes of acute cholecystitis, creating widespread inflammation and adhesions between the gallbladder and the digestive tract.8 Beltrán and Csendes9 reported that an impacted stone in close contact with an inflamed mucosa first develops ischemia, then necrosis, and that because of the associated inflammation of the gallbladder wall with the hepatic or the common bile duct, the impacted stone erodes through them and eventually forms a fistula. This applies to the formation of other biliary fistulas, such as cholecysto-duodenal fistulas, which, in most cases, are needed for gallstone ileus to develop. The most frequent fistula formation takes place between the gallbladder and the duodenum, representing 85% of all types. The other 15% are hepatoduodenal, choledochoduodenal, cholecystogastric, cholecystojejunal and cholecysto-colonic fistulas.5–6,10 Other mechanisms of obstruction are the passage of small stones that migrate through the ampulla of Vater, followed by in situ growth, small stones that impact in a stenotic intestine (for example in Crohn's disease), or inadvertent migration of the gallstone during the manipulation of the gallbladder while performing a cholecystectomy.5–10 Stone size is significant for the onset of bowel obstruction and must measure at least 2cm in diameter to cause obstruction.2,5–8
Clinical presentationGallstone ileus is a mechanical obstruction of the gastrointestinal tract and therefore the site where the stone lodges will induce a variety of clinical scenarios. Barnard's syndrome occurs when the stone obstructs the ileocecal valve.5,10 Only 3% of patients have Bouveret's syndrome, which is the result of the stone lodging in the duodenum and blocking the gastric outlet.8–11 Fewer than 4.8% of the patients present with colonic obstruction.11 Presentation onset can be acute, subacute, or chronic. The acute GI patient typically arrives at the emergency room with a sudden onset of abdominal distention, vomiting, and obstipation. Subacute GI differs from the acute form in that the patient has no stool passage, but passes flatus (low-grade bowel obstruction). The chronic type, or Karewsky syndrome, is characterized by recurrent episodes of pain caused by the passage of gallstones through the bowel, along with an asymptomatic lapse of time, reaching complete obstruction in various stages.5–6,12–13
Clinical symptoms differ, depending on the site of obstruction. In cases of bowel obstruction, abdominal distention, pain, vomiting, the absence of peristalsis, constipation or obstipation, and fluid imbalance are all prevalent.5,8 The patient may also present with jaundice.14 Physical examination and laboratory tests do not point to a particular cause of bowel obstruction.5,12,14 GI diagnosis is suspected when an older patient presents with the Mordor triad5 (history of gallstone, signs of acute cholecystitis, and sudden onset of bowel obstruction). However, other more common causes of bowel obstruction, such as previous abdominal surgeries (adhesions), hernia incarceration or strangulation, and abdominal tumors need to be ruled out.14
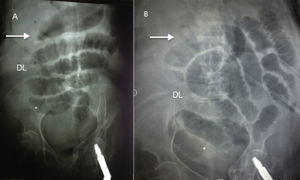
Diagnostic approachAfter the clinical history and physical examination are carefully carried out, paraclinical tests are ordered. The laboratory studies may show an elevated white cell count, abnormal liver function test, and electrolyte imbalance in only a few cases, and so have less diagnostic significance. The imaging study workup in the diagnostic approach to any cause of bowel obstruction begins with the supine and erect abdominal x-ray,15,16 which has 40-70% diagnostic sensitivity.14,17 The imaging diagnostic criteria for gallstone ileus is called Rigler's triad and consists of the presence of a radiopaque stone (presenting in fewer than 10% of the cases), pneumobilia (Gotta-Mentschler sign), and bowel loop distention (fig. 1). The presence of 2 of the 3 signs is diagnostic.6,12,18 It should be noted that pneumobilia is not pathognomonic of gallstone ileus, as it can occur after surgical or endoscopic biliary procedures, as well as in cases of incompetence of the sphincter of Oddi. Evidence of a change in stone position in a second abdominal x-ray is known as Rigler's tetrad.6 Furthermore, Balthazar and Schechter describe a fifth radiologic sign that involves the presence of various fluid levels adjacent to the upper right quadrant. The medial level corresponds to the duodenal bulb and the lateral level to the gallbladder.4,5 When water-soluble oral contrast is used, the Forchet sign (the distinctive feature known as the “snake's head”, with a clear halo made up of radiolucent calculi)5 or the Petren sign (the passage of contrast material to the biliary tract)12 can be seen (fig. 2). We emphasize that barium administration is contraindicated when bowel obstruction is suspected, because it may induce complete obstruction and aggravate the symptoms. In addition, if there is a perforation, the extravasation of the contrast material can cause a potentially fatal inflammatory response with barium peritonitis.6,14–16
Abdominal ultrasound is not very useful in the setting of intestinal obstruction.5,19 Nevertheless, regarding gallstone ileus, in the hands of an experienced radiologist, ultrasound can reveal residual cholelithiasis, the presence of a bilioenteric fistula, the location of the lodged stone within the bowel lumen, and aerobilia5,6. The use of x-rays in conjunction with abdominal ultrasound increases sensitivity to 74%.19 Lameris et al.20 reported that a conditional CT strategy, carried out exclusively after negative or inconclusive ultrasonography, yielded the highest sensitivity and missed only 6% of urgent cases. With this strategy, only 49% of patients would have CT.
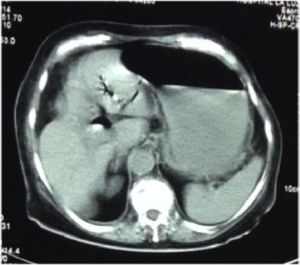
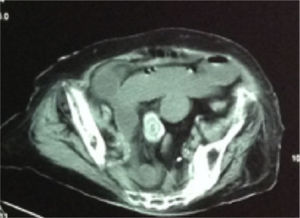
Contrast-enhanced CT scan is considered the gold standard method for GI diagnosis, with sensitivity above 90% 5,8,19,21–25 (figs. 3 and 4). Lassandro et al.25 retrospectively evaluated the clinical relevance of plain abdominal films, abdominal ultrasounds, and contrast-enhanced abdominal computed tomography scans for gallstone ileus diagnosis in 27 cases. Abdominal films identified bowel loop distention in 88.89% of the cases, pneumobilia in 37.04%, and ectopic gallstone in 33.33%. Ultrasound detected 12 patients with signs of bowel obstruction (44.44%), 15 with pneumobilia (55.56%), and 4 with a stone in the gastrointestinal tract (14.81%). Computed tomography scans confirmed signs of bowel obstruction in 96.3% of the patients, pneumobilia in 88.89%, and an ectopic stone in 81.48%. They found Rigler's triad in 4 plain abdominal films (14.81%), in 3 ultrasounds (11.11%), and in 21 contrast-enhanced abdominal CT scans (77.78%).
Finally, upper endoscopy in patients with Bouveret's syndrome,5 or colonoscopy in the event of obstruction in the ileum or colon,5,26 can be successfully performed with the therapeutic procedures described. Zielinski et al.26 reported the first case of colonic gallstone ileus resolution through electrohydraulic lithotripsy. They stated that endoscopically accessible impacted gallstones are amenable to less invasive alternative therapeutic options, including electrohydraulic lithotripsy, extracorporeal shock wave lithotripsy, intracorporeal laser lithotripsy, and endoscopic mechanical lithotripsy for fragmentation. According to Zimadlova et al.,8 colonoscopic removal of the impacted gallstone should be attempted in cases of colonic gallstone ileus. The therapeutic option of interventional endoscopy in high-risk patients is the best treatment choice.5 These procedures still must undergo the “test of time”, to be approved and correctly used. Therefore, they should only be performed in stable patients and by highly specialized and trained endoscopists.
TreatmentDiagnosis of gallstone ileus is a challenging process because the symptoms are not unique to that pathology. In fact, the manifestations of small bowel obstruction are present in many differential diagnoses (adhesions, internal hernia, tumor, volvulus, and others). There is usually an average 7-day lapse of time from the onset of bowel obstruction symptoms to surgical management, with an accurate diagnosis of GI in fewer than 70% of the cases.5–6,27–28 Surgical treatment of gallstone ileus is performed as the result of its preoperative diagnosis or as an intraoperative finding and the approach can be enterolithotomy, alone, or one-stage or two-stage surgery.
Enterolithotomy, alone, is the extraction of a stone through an enterotomy, without performing a procedure to resolve the fistula or the gallbladder disease. This technique is carried out more frequently than the others, because it achieves the primary treatment goal, without exposing the patient to a more prolonged and complicated surgery.2,28–29 Reisner and Cohen 29 conducted the largest analysis of GI cases. They compared mortality in patients that underwent an enterolithotomy procedure and in patients that had one-stage surgery. The results showed that enterolithotomy had a mortality rate of 11.7 vs 16.9% in the one-stage surgery group and so the authors concluded that enterolithotomy was the technique of choice. Even though there is a well-known recurrence rate of gallstone ileus of ≈5% (85% within 6 months after the surgical intervention)30 with enterolithotomy, alone,2–3,29–34 the recurrence of biliary symptoms after this procedure is ≈10%.2,3 Spontaneous fistula has also been described.3,28–31 Therefore, enterolithotomy is a good approach for patients with significant comorbidities, hemodynamic instability, or high-risk surgical dissection.
One-stage surgery involves a particular biliary technique (cholecystectomy or cholecystostomy), with fistula closure and enterolithotomy. The supporters of this method state that the risk of recurrence and the chance of developing gallbladder carcinoma are reduced from 15 to 1%.2,10,35–36 Rodríguez-Sanjuán et al.37 compared the results of enterolithotomy, alone, vs one-stage surgery and found that although the latter had higher morbidity, the mortality between groups was similar (the general health condition of the patients in the enterolithotomy group was worse). They concluded that even though they do not support one-stage surgery, it could be an acceptable procedure in low-risk patients. Riaz et al.23 found similar results, deducing that the choice of surgical procedure was determined by the clinical status of the patient. They performed a one-stage procedure in hemodynamically stable patients, whereas enterolithotomy, alone, was considered sufficient for unstable patients. In accordance with previous states, a one-stage procedure should be offered only to patients that have been adequately stabilized in the preoperative period, and when both the general conditions (such as adequate cardiorespiratory and metabolic reserve) and available postoperative intensive care exist, enabling a more prolonged surgical procedure to be performed.
Two-stage surgery consists of enterolithotomy, alone, with interval cholecystectomy plus fistula repair. In spite of the fact that only ≈10% of the patients that undergo enterolithotomy will have recurrent biliary symptoms,2,3 the two-stage operation has been suggested for the treatment of gallstone ileus in young patients at risk for subsequent biliary complications and in patients with retained gallstones at risk for recurrent gallstone ileus.5,38 There is no consensus on the lapse of time from the first stage to and the second stage of the procedure, and it ranges from 4 weeks to 6 months.28,38–39
Some articles report the spontaneous expulsion of the stone in feces, but they all recommend that surgical management of GI be mandatory.8,10,12,34–41 Another therapeutic modality is the laparoscopic approach, emphasizing a faster recovery time with less morbidity and mortality, as well as a shorter hospital stay.42–44 However, this procedure requires a skilled laparoscopic surgeon with the appropriate laparoscopic instruments.
DiscussionSurgical management remains the standard approach for GI, given that with medical treatment, the mortality rate increases to 26.5%.8,10,34 Nevertheless, there is no standardized definitive surgical technique. The aim of the procedure is immediate obstruction resolution (enterolithotomy, alone, accomplishes this). The most important prognostic factor in choosing the surgical approach is the duration of bowel obstruction.22,38 In patients with diagnostic delay, the primary treatment goal should be the prompt relief of the intestinal obstruction through enterolithotomy, alone. However, in younger stable patients, and at the hands of a skilled surgeon, one-stage surgery can be an option.23,37 Preoperative stabilization is essential, with particular attention given to the fluid and electrolyte balance and the management of comorbid conditions.22
As previously mentioned, the recurrence rate after the enterolithotomy procedure is ≈5%, but there is also a 1.9% risk of recurrence after one-stage surgery.30 Mir et al.30 reported that the management of gallstone ileus recurrence should be another enterolithotomy or two-stage surgery in young patients with residual gallstones. They stressed the need for careful palpation of the intestinal tract to identify other stones and thus diminish the risk of recurrence.
In conclusion, establishing a diagnostic algorithm for bowel obstruction is a mainstay for every institution, because it will improve diagnostic accuracy and surgery duration, providing a better outcome for the patient. Gallstone ileus is a condition in elderly patients that usually present with concomitant diseases. Clinicians must suspect this disease in older patients with bowel obstruction and should look for Rigler's radiologic signs. Given the uncommon nature of this clinical entity, relevant literature is limited, and there are no randomized trials to support optimal therapy. Therefore, we suggest that enterolithotomy is the safest of the current options for the management of gallstone ileus.
Conflict of interestThe authors declare that there is no conflict of interest.
Please cite this article as: Ploneda-Valencia CF, Gallo-Morales M, Rinchon C, Navarro-Muñiz E, Bautista-López CA, de la Cerda-Trujillo LF, et al. El íleo biliar: una revisión de la literatura médica. Revista de Gastroenterología de México. 2017;82:248–254.