Gastic cancer is the most frequent neoplasia of the digestive tract worldwide. Incidence rates vary according to the region or country analyzed. Variation in the different regions of Mexico is attributed to very specific dietary, environmental, and genetic patterns. The aim of the present work was to carry out an epidemiologic analysis of the cases of gastric cancer treated at the Hospital Regional de Alta Especialidad ‘Ciudad Salud’, located in Chiapas, Mexico.
Material and methodsA descriptive, ambispective, longitudinal study was conducted. Cases of gastric cancer were searched for in the database from the oncology service of our hospital, that were treated within the time frame of 2007 to 2014. The data obtained were analyzed using the SPSS v. 20 statistics program.
ResultsA total of 100 cases of gastric cancer were detected, 84 of which were included in the study. Forty-one of the cases were men, 43 were women, and their mean age was 57.3 years. Incidence was 2.14 for every 100 oncology patients released from the hospital. Of the study patients, 35.71% stated they had been alcoholics, 22.61% were smokers, and 90.16% were diagnosed with adenocarcinoma. At the end of follow-up, 18 of the study patients had died.
ConclusionThe results of the present epidemiologic analysis showed that the consumption of alcohol and tobacco played an important role in the development of gastric cancer in the patients studied, as well as having a family history of any type of cancer. Because gastric cancer is usually diagnosed in advanced stages, it would be reasonable to formulate a strategy for the prevention, early detection, and control of the disease in the State of Chiapas, Mexico.
El cáncer gástrico es la neoplasia más frecuente del tubo digestivo en todo el mundo. Las tasas de incidencia varían de acuerdo a la región o el país analizado. La variación en diferentes regiones de México es atribuida a patrones alimenticios, ambientales y genéticos muy específicos. El objetivo de este trabajo es realizar un análisis epidemiológico de los casos de cáncer gástrico atendidos en el Hospital Regional de Alta Especialidad «Ciudad Salud», ubicado en Chiapas.
Material y métodosSe realizó un estudio descriptivo, ambispectivo, longitudinal. Se analizó la base de datos del servicio de oncología de este hospital y se buscaron los casos de cáncer gástrico en el periodo de 2007 a 2014. Los datos obtenidos se analizaron con el programa estadístico SPSS v.20.
ResultadosSe detectaron un total de 100 casos de cáncer gástrico; se incluyeron 84; 41 pertenecían al sexo masculino y 43 al sexo femenino. La edad promedio fue de 57.3 años. Se encontró una incidencia de 2.14 por cada 100 egresos de pacientes de oncología. El 35.71% del total de pacientes refirió haber sido alcohólico y el 22.61% refirió ser fumador. Del total de pacientes, al 90.16% se les diagnosticó adenocarcinoma. Al final del seguimiento, del total de pacientes, 18 habían muerto.
ConclusiónLos resultados del presente análisis epidemiológico mostraron que el consumo de alcohol y tabaco tuvo un papel importante en el desarrollo del cáncer gástrico en los pacientes estudiados, así como el tener antecedentes de familiares con cualquier tipo de cáncer. Debido a que el cáncer gástrico generalmente se diagnostica en etapas avanzadas, es razonable que se elabore un plan para la prevención, la detección temprana y el control de esta enfermedad en nuestra región y estado.
Gastric cancer (GC) is one of the most common neoplasias. It holds first place in malignant tumors of the gastrointestinal tract, fourth place in frequency, and second place in death by cancer.1 Incidence rates vary depending on the region or country analyzed. The highest rates are in Japan, with values of 77.9 per 100,000 in men and 33.3 in women. The lowest rates are in North Africa, the United States, and Canada, with rates of 5.9 to 9.0 per 100,000 in men and 2.6 to 5.3 in women.2
In Mexico, GC is the fourth cause of death by cancer in men and the fifth in women,3 whereas the crude GC-associated mortality rate is 8.8%, or 5.0 per 100,000 inhabitants, with a greater predominance in persons above 50 years of age. For the year 2012, GLOBOCAN reported GC as the third cause of death in relation to the different types of cancer. Some geographic areas of the Mexican Republic have higher GC-associated mortality rates, such as the State of Chiapas, with 6.4 per 100,000, compared with Mexico City (4.5 per 100,000), and the State of Mexico (2.5 per 100,000).3
Risk factorsThe origin of GC is considered multifactorial.4–6 The frequency of the different neoplasias of the digestive tract worldwide varies in relation to geographic location, ethnicity, genetic and environmental factors, dietary habits, and exposure to carcinogenic agents.7
Diet has a strong influence. The present risk factors described are: salt, salted meat, carbohydrates, and coffee. Fruit, carotene-rich vegetables, vitamin C, and refrigeration for food storage have been described as protective factors.4–6,8
Vegetables contain abundant nitrates that are converted into nitrites by bacteria in the saliva. Nitrites transformed into nitrosamines in the stomach damage the inflamed mucosa. Vitamin C neutralizes the nitrosamines, which is why smoking is also a risk factor, given that it decreases vitamin C levels. Consuming fruits and vegetables, together with cured foods, has a similar protective effect.5 The consumption of capsaicin, the irritating element in chili peppers, has been studied in Mexico and is considered a risk factor for the development of GC.4
Alcohol consumption has a harmful effect on the stomach by sensitizing the mucosa in the presence of carcinogenic agents, and is attributed to the nitrosamine content in alcoholic beverages.9 Smoking has also been described to increase the risk for GC 1.5 to 1.6 times.4 Cigarette smoke contains N-nitrosamines and nitrogen oxides, both gastric carcinogens, because they form free radicals with an elevated oxidizing potential. Another risk factor is infection from viral and bacterial oncogenic agents that trigger chronic inflammatory reactions due to their proclivity for establishing life-long infections.10
The frequency of gastric cancer has been reported to significantly increase after 50 years of age,10,11 rarely presenting in patients under 30 years old. GC mortality is closely related to socioeconomic conditions in the first years of life, consistent with a greater prevalence of Helicobacter pylori (HP) infection in childhood in poor populations.2HP is the main determining factor in the appearance of GC.2,3,5 The risk for developing GC is 6 times higher in the population with HP infection. The appearance of atrophic chronic gastritis, intestinal metaplasia, and dysplasia is postulated to be a long process that takes years or decades.3 A high frequency of GC and its association with HP infection has been identified in the population in the State of Chiapas, Mexico.2
Another risk factor is the Epstein-Barr virus (EBV), which has been detected in an average of 10% of cases in association with GC.9,11 Some of the highest incidence rates are in Latin America: in Chile with 23.6% and in Colombia with 13%. Incidence in Mexico is close to 8%.9
Workplace risk factors from different industries have also been observed in workers exposed to silicon, lead, and asbestos, which irritate the gastric mucosa and act as carcinogens.3,4
The increase in proximal digestive tract cancer in developed countries appears to be related to the increased incidence of Barrett's esophagus.12
ClassificationThere are two histologic types of GC classified by Lauren as intestinal and diffuse.3,11,12 The intestinal type develops from precancerous lesions, such as atrophic gastritis and intestinal metaplasia. It is more frequent in males, in older age groups, and in zones in which GC is epidemic.11 The diffuse type does not originate in recognizable precancerous lesions and is predominant in endemic zones. It is more frequent in women,3 as well as in persons with type A blood.11,13
Clinical manifestationsUnfortunately, clinical symptoms are nonspecific, resulting in clinical diagnoses after symptoms have become obvious.4 Most patients have weight loss,4,6 anorexia, fatigue, anemic syndrome, epigastric discomfort, postprandial fullness, gastrointestinal bleeding, a palpable mass, and/or acute abdomen due to gastric perforation.3
Given the high mortality rate of GC, the present study was conducted. Its aim was to perform an epidemiologic analysis of the cases of GC seen at the Hospital Regional de Alta Especialidad «Ciudad Salud» (HRAECS) in the State of Chiapas, Mexico.
Materials and methodsA descriptive, ambispective, longitudinal study was conducted. The registers from the oncology service database of our hospital were reviewed, searching for cases of GC within the time frame of 2007-2014. The study included all the patients with a histologically confirmed diagnosis and complete clinical information. The patients were then located by telephone to find out about their disease progression. A database was created in Excel with the information of the patients that fit the inclusion criteria.
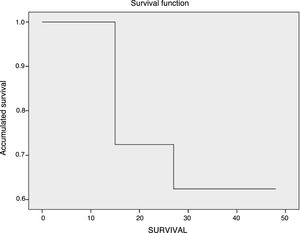
Statistical analysisThe study results were expressed through means (±SD), ranges, percentages for dichotomous variables, and Kaplan-Meier curves for survival with statistical significance of 0.05. Some variables were compared using the chi-square test. The survival curve was calculated through the Kaplan-Meier estimator. The analysis was carried out using the Windows SPSS (v. 20.0) statistics package.
The present study was approved by the Research and Ethics Committee of the HRAECS, with registration number 010/2017.
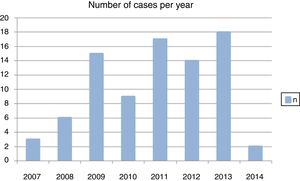
ResultsA total of 100 cases of GC were detected, and 84 that met the inclusion criteria were included. Sixteen cases were rejected because they had no histologic confirmation, or the clinical history was not complete. Incidence was 2.14 for every 100 oncology patients released from the hospital. Within the time frame of 2007-2014, a variation of new cases per year was observed (fig. 1).
Sociodemographic characteristicsOf all the cases, 41 were men and 43 were women (a 1:1.04 ratio). Mean age was 57.3 years, with a range from 25 to 87 years. Mean age was 58.7 years in men and 55.9 years in women.
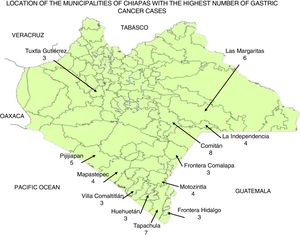
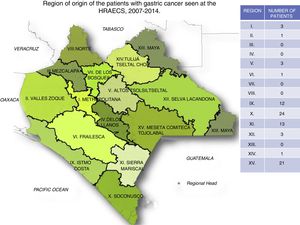
Figure 214 shows the municipalities where the patients with GC were from and are those that stand out from a total of 38. Figure 314 shows the socioeconomic zones where the patients with GC were from. Of the 84 cases, 2 were not from the State of Chiapas.
Table 1 describes the sociodemographic characteristics of the patients.
Sociodemographic characteristics of the patients with GC seen at the HRAECS within the time frame of 2007-2014.
| Variables | n | % |
|---|---|---|
| Sex | ||
| Women | 43 | 51.19 |
| Men | 41 | 48.81 |
| Educational level | ||
| Illiterate | 17 | 20.24 |
| Primary school completed or not completed | 48 | 57.14 |
| Secondary school completed or not completed | 9 | 10.71 |
| High school | 8 | 9.52 |
| University | 2 | 2.38 |
| Occupation | ||
| Housewife | 40 | 47.62 |
| Farmer | 28 | 33.33 |
| Businessperson | 2 | 2.38 |
| Retired | 1 | 1.19 |
| Employed | 4 | 4.76 |
| Unemployed | 9 | 10.71 |
| Religion | ||
| Adventist | 2 | 2.38 |
| Catholic | 63 | 75 |
| Christian | 18 | 21.42 |
| Jehova's Witness | 1 | 1.2 |
| Civil status | ||
| Married | 49 | 58.33 |
| Divorced | 2 | 2.38 |
| Single | 13 | 15.48 |
| Common law union | 11 | 13.1 |
| Widowed | 9 | 10.71 |
| Social Security | ||
| ISSTECH | 1 | 1.19 |
| IMSS | 1 | 1.19 |
| Seguro Popular | 68 | 80.95 |
| None | 14 | 16.66 |
A total of 35.71% of the patients stated they had been alcoholics and 22.61% declared they were smokers.
Clinical characteristicsA total of 25.28% of the patients had a relative that had presented with cancer and 8.04% had relatives with GC. Patient blood type was O, A, and B in 73.91, 18.84, and 7.25%, respectively. The parameters of hemoglobin, glucose, and body mass index (BMI) were compared between the men and women (Table 2).
Parameters of hemoglobin, glucose, and BMI in male and female patients with gastric cancer seen at the HRAECS from 2007-2014.
| Parameter | Men | Women | ||
|---|---|---|---|---|
| Mean | Standard deviation | Mean | Standard deviation | |
| Hemoglobin (g/dl) | 10.81 | 3.30 | 10.99 | 2.2 |
| Glucose (mg/dl) | 103 | 18.05 | 107 | 44.74 |
| BMI (kg/m2) | 22.98 | 3.95 | 24.67 | 4.31 |
Of all the patients, 5 had a qualitative ELISA test for HP and one was positive. Five cases had a histopathologic diagnosis related to HP.
Carcinoma was diagnosed in 90.16% of the patients, whereas the rest had different diagnoses. In relation to the Lauren classification, 13.09% of the patients had diffuse GC and 28.57% had intestinal GC. The classification was not performed on the remaining patients. At the end of follow-up, 18 patients had died and 61.11% of the patients that died had a diagnosis of carcinoma. Of those 18 patients, 38.8% were housewives, 33.3% were farmers, 16.6% were unemployed, 5.5% were carpenters, and 5.5% were mechanics. A total of 22.2% of the patients that died had experienced chronic exposure to smoke.
The patients received different types of treatment, but it was registered in only 59 patients. Table 3 shows the treatments and the number of patients that had them.
Treatment received by patients seen at the HRAECS from 2007-2014.
| Treatment | n | % |
|---|---|---|
| None | 1 | 1.69 |
| Radiotherapy exclusively | 1 | 1.69 |
| Chemotherapy exclusively | 21 | 35.59 |
| Surgery exclusively | 15 | 25.42 |
| Surgery and chemotherapy | 17 | 28.81 |
| Chemotherapy and radiotherapy | 2 | 3.39 |
| Chemotherapy, radiotherapy, and surgery | 2 | 3.39 |
A high glucose level was found to have no relation to a less favorable diagnosis of the disease.
SurvivalThe Kaplan-Meier method was utilized to carry out the survival analysis in the patients that presented with GC15 and it took into account the information of the patients that died, as well as the censored patients. Survival at one, 2, 3, and 4 years was determined. The log-rank test was used in the stratified analysis16 to evaluate the differences between the survival curves. Overall survival in the 84 patients was 67%, showing a one-year survival of 72% and a two to four-year survival of 62%, with a mean survival rate of 38.8% (95% CI: 34.7-42.9). The survival curve differences were not statistically significant (p=0.66) (fig. 4).
DiscussionIn Mexico, GC is a public health problem. Within the time frame of 2007 to 2014 a total of 84 cases of GC were registered. A study carried out at the Hospital Juárez de México reported 234 cases of GC over a 4-year period (2006-2010).17 The highest incidence worldwide was reported in Japan: 77.9 per 100,000 in men and 33.3 in women.2 Incidence in Mexico is 3.3 per 100,00011 and in Chiapas is 6.4 per 100,000.3 In the present study, incidence was 2.14 for every 100 oncology patients released from the HRAECS. In Chiapas, malignant tumors are reported as the second cause of death, with a rate of 52 per 100,000 inhabitants.18
Stomach cancer mostly affects advanced-age persons, with a reported age between 65 and 69 years at the time of diagnosis.17,19 In Mexico, the reported age is from 50 years and in the present study, which included patients 25 years of age with the diagnosis, the mean age was 57 years.
For the year 2008, reports indicate that the frequency of GC had a man:woman ratio of 1.2:1.20 We found a minimal difference, with a man:woman ratio of 1:1.04. Likewise, persons with blood type A have been described as having a greater risk for presenting with GC.3,11 Of the patients in our study, 73.91% had blood type O.
Weight loss and anorexia syndrome have been described as symptoms of patients with GC.4,6 We observed body mass indices of our patients within normal parameters, but there were also patients that had considerable weight loss: in women the lowest weight was 32kg, and in men 33.5kg. The mean hemoglobin value in men was 10.81g/dl, and in women it was 10.99g/dl, far below normal values.
A family history of cancer, and specifically of GC, have been described as risk factors for presenting with GC.1,5,7,21 In our study those percentages were 25.28 and 8.04%, respectively.
The main risk factors associated with GC are HP infection, heavy smoking, and to a lesser degree, alcohol consumption.1,4,21,22 In our results, 35.71% of the patients stated they had been alcoholics and 22.61% said they were smokers. Likewise, we found 10 patients that had related HP infection: 5 were determined through qualitative ELISA testing and 5 through histopathology studies.
Using the study by Roesch-Dietlen et al. as a reference, there was an increase in GC cases in 2009.7 In the present study we also observed an increase, but the most notable one was in 2013.
Ninety-five percent of all gastric neoplasias are adenocarcinomas.1,7,19,21 In a study conducted in Mexico City that compared 4 hospitals, 95.73% of the tumors were adenocarcinomas.22 Of all our cases, 90.16% were classified as adenocarcinomas.
The main treatment for GC is surgical.4 In our study, the majority of the patients were treated exclusively with chemotherapy, whereas surgery was the treatment that was the second in frequency.
Survival is very low in patients with GC5. In a study conducted in Chiclayo, Peru, the authors found survival rates of 31.5% and 53% at 5 years of follow-up,23 whereas our patients at the HRAECS had a survival rate of 62% at 4 years of follow-up.
Our study results did not show a big difference between men and women in relation to GC presentation. Some of the patients with GC were very young, but the age of the majority of patients was similar to that reported in Mexican populations. Regarding risk factors, we could not conclude that there was a relation between HP and GC, given that HP testing was not part of the laboratory studies performed on all the patients. However, we did find that exposure to smoke was a factor present in our patients. GC is an aggressive neoplasia that mostly affects the advanced-age population, but it also affects young persons. A younger age at the time of diagnosis has been reported in Mexico, compared with other countries. There are many risk factors for developing GC, and alcohol consumption and smoking are the most outstanding non-pathologic factors. Another important factor is a family history of GC or any other neoplasia. In general, GC is diagnosed at advanced stages, conferring a poor outcome on the patient and underlining the importance of creating prevention, early detection, and disease control strategies.
ConclusionsAn epidemiologic analysis was carried out in relation to the cases of GC seen at the HRAECS, in the State of Chiapas.
GC is an aggressive neoplasia that mostly affects the advanced-age population, but it can also present in young persons.
In the present analysis, we found that the consumption of alcohol and tobacco played an important role in the development of GC, as did a family history of any type of cancer.
In general, GC is diagnosed at advanced disease stages, resulting in poor patient prognosis. Therefore, developing a plan for the prevention, early detection, and control of the disease in the State of Chiapas is a reasonable endeavor.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Financial disclosureThe authors received financial support from the E022IV010 budget program “Fomentar la investigación en Salud” from the Health Department's Centro Regional de Alta Especialidad de Chiapas.
Conflict of interestThe authors declare that there is no conflict of interest.
Please cite this article as: Canseco-Ávila LM, Zamudio-Castellanos FY, Sánchez-González RA, Trujillo-Vizuet MG, Domínguez-Arrevillaga S, López-López CA. Epidemiología de cáncer gástrico en el tercer nivel de atención en salud en Chiapas. Revista de Gastroenterología de México. 2019;84:310–316.