Achalasia is characterized by incomplete relaxation of the lower esophageal sphincter and esophageal aperistalsis. The efficacy of peroral endoscopic myotomy (POEM) is similar to that of the Heller myotomy, with an apparently greater prevalence of gastroesophageal reflux disease. Our aim was to determine the presence of GERD in a post-POEM cohort of Mexican patients with achalasia and follow-up of at least 12 months.
Materials and methodsA retrospective cohort study was conducted on post-POEM patients with a minimum of 12 months of follow-up, within the time frame of 2012 to 2017. Pregnant patients were excluded. Serial endoscopy, pH study, and GERDQ application were performed. Univariate and bivariate data analyses were carried out and statistical significance was set at a P<0.05.
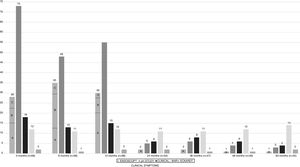
ResultsSixty-eight patients had post-POEM follow-up for 12 months. Of those patients, follow-up continued to 24 months for 58, 36 months for 47, 48 months for 39, and 60 months for 25. Mean patient age was 47.8±14.3 years, 57.3% of the patients were women, 77.9% were treatment-naïve, and 54.4% had type II achalasia. The pH study, endoscopy, and questionnaire were positive in 73, 28, and 18% at 3 months; 48, 35, and 13% at 6 months, and 55, 30, and 15% at 12 months, respectively. Once the proton pump inhibitor was begun, the percentages decreased to 5, 2, and 6% at 24 months; 6, 2, and 8% at 36 months; 4,1, and 6% at 48 months; and 3, 1, and 4% at 60 months, respectively. There was no relation between the efficacy of POEM and the presence or intensity of GERD. There were no secondary complications due to gastroesophageal reflux.
ConclusionsThe post-POEM prevalence of GERD was 50% in the short term (12 months), with no evidence of complications at the medium term or long term (60 months). Gastroesophageal reflux was adequately controlled through proton pump inhibitors administration in over 95% of the cases.
La acalasia se caracteriza por una relajación incompleta del esfínter esofágico inferior y aperistalsis esofágica. La miotomía endoscópica por la boca (POEM) brinda una eficacia similar y aparentemente mayor prevalencia de la enfermedad de reflujo gastroesofágico (ERGE) que la miotomía de Heller. Nuestro objetivo fue determinar la presencia de la ERGE en una cohorte de pacientes mexicanos pos-POEM con acalasia y un seguimiento mínimo de 12 meses.
Material y métodosSe trata de un estudio de cohorte retrospectivo en el que se incluyó a pacientes pos-POEM con un mínimo de 12 meses de seguimiento entre 2012 y 2017; se excluyó a pacientes embarazadas. Se realizaron endoscopia, pHmetría y cuestionario GERDQ de forma seriada. Los datos se analizaron de forma univariada y bivariada considerando una p<0.05 como estadísticamente significativa.
ResultadosEl seguimiento se completó en 68 pacientes (12 meses); 58 (24 meses); 47 (36 meses); 39 (48 meses) y 25 pacientes (60 meses) pos-POEM; con una edad de 47.8±14.3años; con un 57.3% de mujeres, 77.9% vírgenes para el método y un 54.4% con acalasia de tipo II. La phmetría, endoscopia y cuestionario fueron positivos en 73, 28% y 18% (3meses); en 48, 35 y 13% (6meses) y en 55, 30 y 15% (12 meses) y, una vez iniciado el inhibidor de bomba de protones, los valores disminuyeron a 5, 2 y 6% (24 meses); a 6, 2 y 8% (36 meses); a 4, 1 y 6% (48 meses) y a 3, 1 y 4% (60 meses), respectivamente. No hubo relación entre la eficacia de la POEM y la presencia o intensidad de la ERGE, ni complicaciones secundarias a su presencia.
ConclusionesLa prevalencia de la ERGE pos-POEM es de hasta el 50% a corto plazo (12 meses), pero sin evidencia de complicaciones a mediano y largo plazo (60 meses) y puede ser controlada adecuadamente con inhibidores de la bomba de protones en más del 95% de los casos.
Achalasia is a primary motor disorder of the esophagus, characterized by incomplete relaxation of the lower esophageal sphincter and esophageal aperistalsis, which results in delayed emptying of the esophagus. It clinically manifests as progressive dysphagia, chest pain, regurgitation, and involuntary weight loss.1–3High-resolution manometry (HRM) enables the definitive diagnosis of the disease and classifies it into 3 subtypes: with no pressurization (type I), with panesophageal pressurization (type II), and with spasm (type III). Said classification has been a great help in “directing” the most adequate type of treatment for the patient.3–5Laparoscopic Heller myotomy (LHM) with partial fundoplication is considered the gold standard in the treatment of the disease. Peroral endoscopic myotomy (POEM) is a novel treatment that also enables improved esophageal emptying through the disruption of the muscle fibers of the body of the esophagus, involving the lower esophageal sphincter and the adjacent gastric muscle layer.6,7 LHM combined with partial fundoplication has shown adequate safety and efficacy in patients at the short term, medium term, and long term.8–12 POEM has shown similar results to LHM at the short term, medium term, and long term,13–15 unlike other endoscopic treatments that only offer temporary improvement. One such treatment is the use of botulinum toxin. That biologic substance has an initial response rate of approximately 90%, but the effect wears off and repeat treatments are required. At present, treatment with that toxin is reserved for patients that are not candidates for surgery.16,17 Another treatment is esophageal dilation, which although effective in advanced-age patients, has a high perforation rate (5-9%).18
POEM has an initial clinical response rate of 80-96% and is maintained at up to 88% in the medium term at 3 years.19,20 It has the advantage of being less invasive than LHM, with similar efficacy.21,22 In addition, it is superior to LHM in patients with subtype III achalasia and in patients above 65 years of age.23 Nevertheless, different authors have reported an increased incidence of reflux after the procedure, higher than that with LHM at the short term and medium term. Said reflux has been documented between 45 and 55%, determined through different methods, such as endoscopy and 24-hour pH study. However, there does not appear to be a direct relation between the clinical and endoscopic findings in those patients, nor is its real medium-term and long-term behavior and impact known.7,24,25 Therefore, our primary aim was to determine the prevalence of gastroesophageal reflux disease (GERD) in a cohort of Mexican patients with achalasia treated with the POEM technique, and our secondary aim was to determine its medium-term and long-term behavior at a minimum of 12 months of follow-up.
Materials and methodsA retrospective cohort study was conducted on a group of postoperative patients that underwent POEM within the time frame of November 2012 to December 2017 at the Department of Digestive Endoscopy of the Hospital de Especialidades Centro Médico Nacional Siglo XXI.
Inclusion and exclusion criteriaThe patients included in the study were above 18 years of age and persons of either sex. They had a diagnosis of esophageal achalasia confirmed by HRM (ManoScan ESOsystem; Given Imaging, Covidien; Dublin, Ireland) and underwent the POEM procedure, after which they were objectively evaluated for the presence of GERD at a minimum of 12 postoperative months. The patients excluded from the study were those that did not complete the GERD evaluation, did not undergo POEM, were pregnant women, were lost to follow-up, or had incomplete clinical records.
Before the performance of POEM, the demographic, clinical (Eckardt score), endoscopic, and manometric characteristics of the patients were documented.
Documentation of gastroesophageal reflux diseaseThree evaluations were carried out for the follow-up and evaluation of GERD: a validated clinical questionnaire (GERDQ), upper gastrointestinal endoscopy, and esophageal 24-hour pH study. Reflux was defined as positive with any of the following criteria: esophageal acid exposure above 6% determined through pH study,26 any degree of erosive esophagitis determined through upper gastrointestinal endoscopy (the Los Angeles classification), or a GERDQ score equal to or above 8 points. Those evaluations were carried out periodically after the POEM at 3, 6, 12, 24, 36, 48, and 60 months. In addition, the efficacy of the procedure was evaluated at those same time intervals through HRM and the Eckardt score.
Peroral endoscopic myotomy procedurePOEM was carried out utilizing a conventional gastroscope (diameter of 9.8mm, working channel of 2.8mm). A cap was attached to the tip of the gastroscope, along with an electrosurgical unit (ERBE, Tübingen, Germany). The procedure was performed with a type I Hybrid knife (ERBE, Tübingen, Germany) and carbon dioxide insufflation. The previously described POEM technique utilized by our group consists of 5 steps:27
Examination and injection: Diagnostic endoscopy was performed, locating the level of the esophageal gastric junction (EGJ). An anterior approach was utilized in treatment-naïve patients and a posterior approach in patients with a history of previous surgery. A 9% sodium chloride solution, with 0.5% methylene blue, was then injected with a type 1 Hybrid knife. Depending on the achalasia subtype, the injection was placed 10cm from the EGJ for subtypes I and II and at 15cm above the EGJ for subtype III.
Incision: A longitudinal incision between 10 and 15mm was made, which served as the entrance site to the submucosal tunnel, parallel to the major axis of the esophagus.
Tunnel: A submucosal tunnel was created by means of the injection of methylene blue combined with bi-distilled water, extending up to 2-3cm under the EGJ.
Myotomy: The myotomy was begun two centimeters under the incision, performing myotomy of the esophagus, the lower esophageal sphincter, up to 2cm from the intragastric portion below the EGJ.
Closure: Hemostatic or Ovesco clips were used for incision closure. In the cases in which closure with clips was not possible, 1ml of undiluted cyanoacrylate was applied.28
Statistical analysisSample size was calculated, based on the minimum expected frequency of 50% of post-POEM GERD, with a 95% confidence interval, obtaining a formula-based minimum total of 65 patients. Procedure and patient characteristics were documented and expressed according to the type of variable. The quantitative variables were expressed as mean with standard deviation (SD) or median with maximum and minimum values (max-min), depending on their distribution. The qualitative variables were expressed as proportions. A bivariate analysis was carried out, comparing the treatment-naïve patients with the treatment-experienced patients, utilizing the Student's t test, the Mann-Whitney U test, and the Fisher's exact test. A multivariate analysis was carried out to evaluate the factors related to GERD. Statistical significance was set at a p <0.05 and the SPSS version 21.0 program (Chicago, IL, USA) was used.
Ethical considerationsThe present protocol, identified as R-2017-348-42, was approved by the ethics committee of our hospital. It was carried out following the specific norms for that type of study on humans, as well as in accordance with the regulations of the General Health Law for Health Research, the Declaration of Helsinki, and according to the institutional norms and guidelines for scientific research.
ResultsA total of 113 patients were initially included in the study within the time frame of November 2012 to December 2017. Thirty-two of those patients were excluded because they did not meet the inclusion criteria: 18 had a diagnosis other than achalasia, 13 had incomplete case records, one patient died due to a cause unrelated to the procedure, and 13 patients could not complete the pH-study follow-up. The final total of 68 patients were included in the analysis and were operated on by two endoscopists (OVHM [47] and OMSP [21]), with follow-up of a minimum of 12 months. Post-POEM follow-up extended to 24 months for 54 of those patients, to 36 months for 47 patients, to 48 months for 39 patients, and to 60 months for 25 patients.
Mean patient age was 47.8±14.3 years. The predominant sex was female, with 39 women (57.3%). The pre-procedure HRM parameters were: a median integrated relaxation pressure (IRP) of 24.3mmHg (min-max 15.5-53.6) and a baseline lower esophageal sphincter pressure of 28.2mmHg (min-max16-54). According to the Chicago classification, 10 patients (14.7%) had type I achalasia, 37 (54.4%) had type II, and 6 (8.9%) had type III. Fifteen patients (22%) had previously undergone treatment for achalasia (14 LHM and 1 redo POEM). Median time between symptom onset and final diagnosis of the disease was 24 months (min-max 9-140) (Table 1).
General patient characteristics.
| Characteristic | n=68 |
|---|---|
| Age in years, mean (SD) | 47.8±14.3 |
| Sex, number (%) | Women 39 (57.3%)Men 29 (42.6%) |
| Time in months between symptom onset and diagnosis, median (min-max) | 24 (9-140) |
| Type of patient, number (%) | Treatment-naïve 53 (77.9%)Treatment-experienced 14 (20.5%)Redo POEM 1 (1.4%) |
| Pre-POEM Eckardt score, median (min-max) | 9 (1-12) |
| Post-POEM Eckardt score at 3 months; median (min-max) | 2 (0-4) |
| Pre-POEM IRP in mmHg, median (min-max) | 24.3 (15.5-53.6) |
| Post-POEM IRP in mmHg at 3 months, median (min-max) | 11.2 (0-24) |
| Achalasia subtype or motor disorder, number (%) | Type I 10 (14.7%)Type II 37 (54.4%)Type III 6 (8.8%)Previous post-myotomy changes: 15 (22.05%) |
IRP: integrated relaxation pressure; SD: standard deviation
Regarding the procedure characteristics, mean duration of POEM was 88.3±29.9min, 45/68 (66.1%) patients underwent the anterior approach, and 23/68 (33.9%) had the posterior approach. Total myotomy was performed on 58/68 (85.2%) patients and partial myotomy on 10/68 (14.8%). Closure was carried out with clips in 52/68 (76.4%) patients, with cyanoacrylate in 12/68 (17.7%), and with the Ovesco clip in 4/68 (5.9%). The most frequent adverse event was pneumoperitoneum and presented in 15/68 (22%) patients. Decompression puncture was required in only 5 patients. Table 2
GERD parameter comparison between treatment-naïve and treatment-experienced patients.
| Characteristic | Treatment-naïven=53 | Treatment-experiencedn=15 | p |
|---|---|---|---|
| Age in years, mean (SD) | 46.4±1 | 45.1±14.3 | *0.56 |
| Sex, number (%) | Women 30 (56.6%)Men 23 (43.4%) | Women 9 (60%)Men 6 (40%) | **0.71 |
| Positive pH study at 3 months, number (%) | 38 (71.6%) | 11 (73.3%) | **0.08 |
| Positive endoscopy at 3 months, number (%) | 15 (28.3%) | 4 (26.6%) | **0.24 |
| Positive GERDQ at 3 months, number (%) | 10 (18.8%) | 3 (20%) | **0.22 |
| Positive pH study at 6 months, number (%) | 25 (47.1%) | 7 (46.6%) | **0.14 |
| Positive endoscopy at 6 months, number (%) | 19 (35.8%) | 5 (33.3%) | **0.63 |
| Positive GERDQ at 6 months, number (%) | 7 (13.2%) | 2 (13.3%) | **0.92 |
| Post-POEM Eckhardt score at 6 months, median (min-max) | 1 (1-3) | 2 (1-3) | ***0.75 |
| Post-POEM IRP in mmHg at 6 months, median (min-max) | 12.2 (4-18) | 11.5 (3-17) | ***0.48 |
The pre-procedure median Eckardt score was 9 points (min-max 1-12), with a median IRP of 24.3mmHg (min-max 15.5-53.6). At 3 months after POEM, there was a significant reduction in both parameters, with a median Eckardt score of 2 (min-max 0-4) and a median IRP of 11.2mmHg (min-max 0-24), which lasted up to the interval at 6 months. At the follow-up at 12 months, the median Eckardt score was 11.5 (min-max 0-3) and the median IRP was 12.0mmHg (min-max 0-23) and lasted up to 5 years. Recurrence presented in 1/25 (4%) patients and that patient's IRP was above 15mmHg. The rest of the group had a higher median IRP, with respect to the measurements of the previous years, reaching values of 14.1mmHg (min-max 2-24). However, that increase in the IRP did not correlate with the Eckardt score, which remained at a median of 2 points (min-max 0-3) at 5 years. Thus, the general efficacy of POEM over time was maintained in 96% (24/25) of the patients evaluated up to 5 years after the procedure.
Post-peroral endoscopic myotomy gastroesophageal reflux diseaseAll the patients per protocol were treated with the standard dose of a proton pump inhibitor (PPI) for 30 days after POEM. They had no treatment for 8 weeks until their first evaluation at 3 months. If the patient presented with endoscopic data of esophagitis, treatment with a PPI was begun for 8 weeks. At the following evaluation at 6 months, the patient once again underwent pH study, endoscopy, and answered the GERDQ. If any degree of esophagitis presented, treatment with a PPI was newly started for a period of 8 weeks. At 12 months, if the patient had a positive pH study or any sign of esophagitis, single-dose PPI treatment was begun and continued indefinitely.
Three monthsAt 3 months post-POEM, the results of the GERD evaluation showed that 73% of the patients had a positive pH study, 18% had positive clinical reflux, and 28% had esophagitis (85% had grade A or B). The pH study was positive, as was to be expected, in all the cases of esophagitis, but there was no correlation with the clinical GERDQ. There was also no correlation between the post-POEM IRP and the post-POEM Eckardt score. Thus, in cases of esophagitis, treatment was a PPI for 8 weeks.
Six monthsAt 6 months, the pH study was positive in 48% of the patients, 35% had some grade of esophagitis (A:12.5%, B: 20%, and C: 2.5%), and 13% had clinical reflux. There was also no correlation between the 3 parameters, but 100% of the patients that presented with esophagitis in the previous evaluation had esophageal damage in the evaluation at 6 months. The number of patients with abnormal acid exposure was reduced by 25%. There was no relation between the symptomatology or documentation of GERD and clinical efficacy. Again, treatment with a PPI was prescribed for 8 weeks in patients with some grade of esophagitis.
Twelve monthsAt 12 months, 55% of the patients had a positive pH study, 30% had some grade of esophagitis (the majority had grade A [20%]), and 15% had a positive result for GERD on the questionnaire. In general, 7% more patients presented with a positive pH study and 5% fewer patients had some grade of esophagitis, compared with the measurements at 6 months. But just as in the previous evaluations, there was no relation between the clinical, endoscopic, or pH study evaluations, nor with post-procedure efficacy. Treatment with a single-dose PPI for an indefinite period was prescribed for patients that presented with a positive pH study or had some grade of esophagitis.
The remaining evaluationsThe evaluations carried out at 24, 36, 48, and 60 months showed a considerable decrease in the percentage of abnormal esophageal acid exposure, with 5, 6, 4, and 3% through pH study and 2, 2, 1, and 1% through endoscopy, respectively. Only grade A esophagitis was observed at endoscopy in all the cases. Nevertheless, the clinical evaluation was overestimated, with positive questionnaire results in 6, 8, 6, and 4% in the corresponding assessments. Finally, the multivariate analysis showed no association with GERD, according to the different factors included: clinical success, manometric success, type of myotomy (partial vs. total), approach (anterior vs. posterior), or weight gain (p=0.42). None of the patients presented with any other type of complication secondary to GERD (Barrett's esophagus, esophageal stricture, or esophageal adenocarcinoma) at the post-POEM follow-up at 60 months (fig. 1).
Treatment-naïve vs treatment-experiencedA bivariate analysis of the treatment-naïve patients (n=53) vs. the treatment-experienced patients (n=15) included in the follow-up at 12 months was carried out. There were no statistically significant differences in the reflux parameters evaluated in the two groups in relation to the results of endoscopy, pH study, or clinical symptoms in the evaluation at 12 months, nor were there any during the later evaluations (up to 60 months), post-POEM. There were also no differences with respect to the Eckardt score or the IRP values after the proc
DiscussionIn the present study, we could confirm that the prevalence of GERD, defined as abnormal esophageal acid exposure, was high at the short term and medium term in a Mexican population after treatment with POEM (73% at 3 months, 48% at 6 months, and 55% at 12 months). Those values are similar to figures reported by other centers.20,25,29 However, we were able to determine a long-term follow-up of 60 months in 36.7% (25/68) of the total cohort. We found that at 12 months of treatment, there were no big changes from the measurements at 3 and 6 months. In our opinion, indefinite PPI administration was the most adequate, controlling reflux in 95% of the cases, with only 3 to 6% with abnormal acid exposure and under 50% of cases with some grade of esophagitis. Thus, even though the real initial prevalence of GERD after the procedure was high, it could be adequately controlled in nearly all the cases. Those results concur with the data reported in other centers, albeit with a shorter average follow-up period (3 years).19–21,23,29,30
The treatment goal in achalasia is to improve esophageal emptying and consequently prevent the complications secondary to the disease. Surgical treatment with LHM is a good alternative for those patients. Said procedure initially included only direct myotomy of the lower esophageal sphincter, 6cm from the esophageal portion and 2-3cm from the gastric portion. Despite its adequate efficacy (> 90%), the documented prevalence of reflux was also high (60%), making it necessary to add an antireflux procedure. According to different studies, the incidence of reflux was reduced to 15-35%,17,21,24 figures that are lower than those reported after POEM. However, those figures have been questioned due to a lack of objectivity in the studies conducted on patients that underwent LHM, resulting from poor systematization and follow-up, as well as heterogeneity in the definitions of GERD used by the different authors (and with no pH study, endoscopy, or validated clinical questionnaire).29,30 Be that as it may, the results are recognized as lower than those currently reported for POEM, specifically because the peroral procedure does not have an associated antireflux maneuver, leaving the patient at risk. It offers figures similar to those obtained through LHM without partial fundoplication.1,8
POEM is a revolutionary technique in “surgical” therapeutic endoscopy, not only because it is a true “surgery” performed by an endoscopic team, and therefore the first success of the natural orifice transluminal endoscopic surgery (NOTES) concept, but also because of its efficacy and safety demonstrated in the short term, medium term, and long term, at different hospital centers.19–21,23,25 In the present study, POEM was confirmed as a safe and effective technique in the short term, medium term, and especially in the long term, given that 96% of the patients continued to present with clinical and manometric improvement up to 60 months after the procedure. Twenty-two percent of the patients had the minor adverse event of pneumoperitoneum, and only 5 of those patients required abdominal decompression via puncture.
The true risk factors for post-POEM reflux are not currently known, which is why we used the multivariate analysis for that assessment. We included the reported factors that could determine its presence, such as the type of myotomy, approach and extension, post-POEM Eckardt score, post-POEM IRP, and weight gain. Those variables showed no association with the presence of GERD in patients with achalasia treated with the POEM method we employed. Similar data were found at other hospital centers.3,20,25,29
PPIs appear to be the cornerstone of treatment in patients with post-POEM GERD. In our cohort, 73% had a positive pH study at the evaluation at 3 months, and of those patients, under 50% presented with some type of tissue damage confirmed at endoscopy. However, after administering treatment with a PPI in the patients with damage observed at endoscopy, said lesions persisted in the two following evaluations, despite having received adequate doses in relation to time and quantity for their resolution. In addition, of the “new” cases of reflux at the evaluations at 6 and 12 months, identified through endoscopy, all the patients had a positive pH study in the previous evaluations, suggesting that practically all patients with a positive pH study would present with some grade of esophagitis at some point of their evaluation, which is why we considered the indefinite treatment with PPIs to be the best alternative in those cases. In addition, GERD was controlled with that measure and less than 5% of the cases continued to have a positive pH study or present with esophageal damage. Said persistence was possibly due to poor treatment adherence, a dietary transgression (once patients begin to feel better, they tend to eat all types of food), or inadequate PPI doses prescribed to those patients, but in all the cases evaluated, there was only mild esophageal mucosal damage (grade A esophagitis). No severe complications, such as esophageal stricture, Barrett's esophagus, or esophageal adenocarcinoma were observed. Different authors have expressed concern about those serious complications in the medium-term or long-term evaluation of those patients.1,3,5,14,21,29,30
Regarding the clinical evaluation of reflux, the role of the different questionnaires that determine the severity of typical symptoms has been evaluated. They have been shown to have low sensitivity (20-25%), good specificity (87.5%), adequate PPV (83.3%), and deficient NPV (30.4%), signifying low diagnostic accuracy (41.3%). In other words, patients that complain of symptoms have a high probability of presenting with GERD, but the majority of patients with GERD in that specific population are asymptomatic and their signs do not correlate with evaluations through pH study (sensitivity: 90.4%, specificity: 100%, PPV: 100%, and NPV: 80%) or conventional endoscopy (diagnostic accuracy: 75.8%).1,3,25,29,30 Therefore, we recommend that all post-POEM patients be objectively evaluated through pH study or digestive endoscopy at least at 6 months after the procedure. If a case is positive at endoscopy, we suggest giving the corresponding treatment and then continuing with a PPI indefinitely. If the patient has a positive pH study, we recommend indefinite treatment with a PPI, given that those patients are at high risk for progressing at some point from a “non-erosive” stage to an “erosive” stage.
Among the weaknesses of the present study, the first is its retrospective nature, which does not allow the researcher to adequately assess the maneuver homogeneously. However, we attempted to exclude all cases that did not have an adequate evaluation of GERD at all the follow-up points. The second was the sample size. It was sufficient for obtaining statistical significance at the follow-up at 12 months, but not at the medium term or long term, at which points a larger sample would most likely be required to confirm the results. And third, was the comparison between treatment-naïve and treatment-experienced patients in relation to the presence or absence of reflux. It was considered preliminary data, given that it was not the primary aim of the study. Even though no difference was shown between the two groups regarding the presence of reflux after POEM, the two groups were distinct. In the treatment-experienced group, there was a subgroup of patients (LHM) that had undergone an antireflux procedure. Therefore, the comparison between treatment-naïve and treatment-experienced patients in relation to the presence of reflux after POEM could not be considered a real comparison. Nevertheless, it did show that the behavior of GERD at 12 months after treatment, in the treatment-experienced patients (n=15), did not appear to be different from that of the treatment-naïve patients after POEM. A specific evaluation of that group of patients would be recommendable to confirm those results.
Finally, we believe the findings of our study are of great value to the endoscopists and gastroenterologists that evaluate patients with achalasia that undergo POEM. In particular, the findings provide initial information on the medium-term and long-term behavior of reflux after a procedure that is gaining in popularity but is still too recent a creation to be considered the new “gold standard” in that pathology.
ConclusionGERD, defined as abnormal esophageal acid exposure in post-POEM patients, presented in more than 50% of the patients in the short term. However, there was no correlation with clinical or endoscopic findings, nor with major adverse events, and could be adequately controlled through PPI use in more than 95% of the patients in the short term, medium term, and long term.
Financial disclosureNo financial support was received in relation to this article.
Conflict of interestThe authors declare that there is no conflict of interest.
Please cite this article as: Hernández-Mondragón OV, Solórzano-Pineda OM, González-Martínez M, Blancas-Valencia JM. Enfermedad por reflujo gastroesofágico posterior a miotomía endoscópica a través de la boca: Resultados a corto, mediano y largo plazo. Revista de Gastroenterología de México. 2020;85:4–11.