Intestinal intussusception (II) is defined as that which presents when the proximal intestinal segment is introduced over the distal segment, obliterating its lumen. It is one of the main causes of bowel obstruction in children but is rare in adults.1 Only 5% of adults with obstruction present with II.2 An important difference between children and adults is an identifiable cause of the II, given that it is idiopathic in the majority of pediatric cases, whereas etiology is identified in up to 90% of cases in adults. An incidence of 2 cases/100,000 inhabitants has been reported in adults,3 mainly affecting the small bowel and colon in up to 90% of cases; it rarely affects the stomach.4
A 53-year-old woman had a past medical history of papillary thyroid cancer (2019), treated surgically. She received radiotherapy with 100 Gy of iodine. Afterwards, she presented with secondary hypothyroidism and currently receives supplementation. She stated that she did not consume alcohol significantly and did not smoke. Her family history was unremarkable.
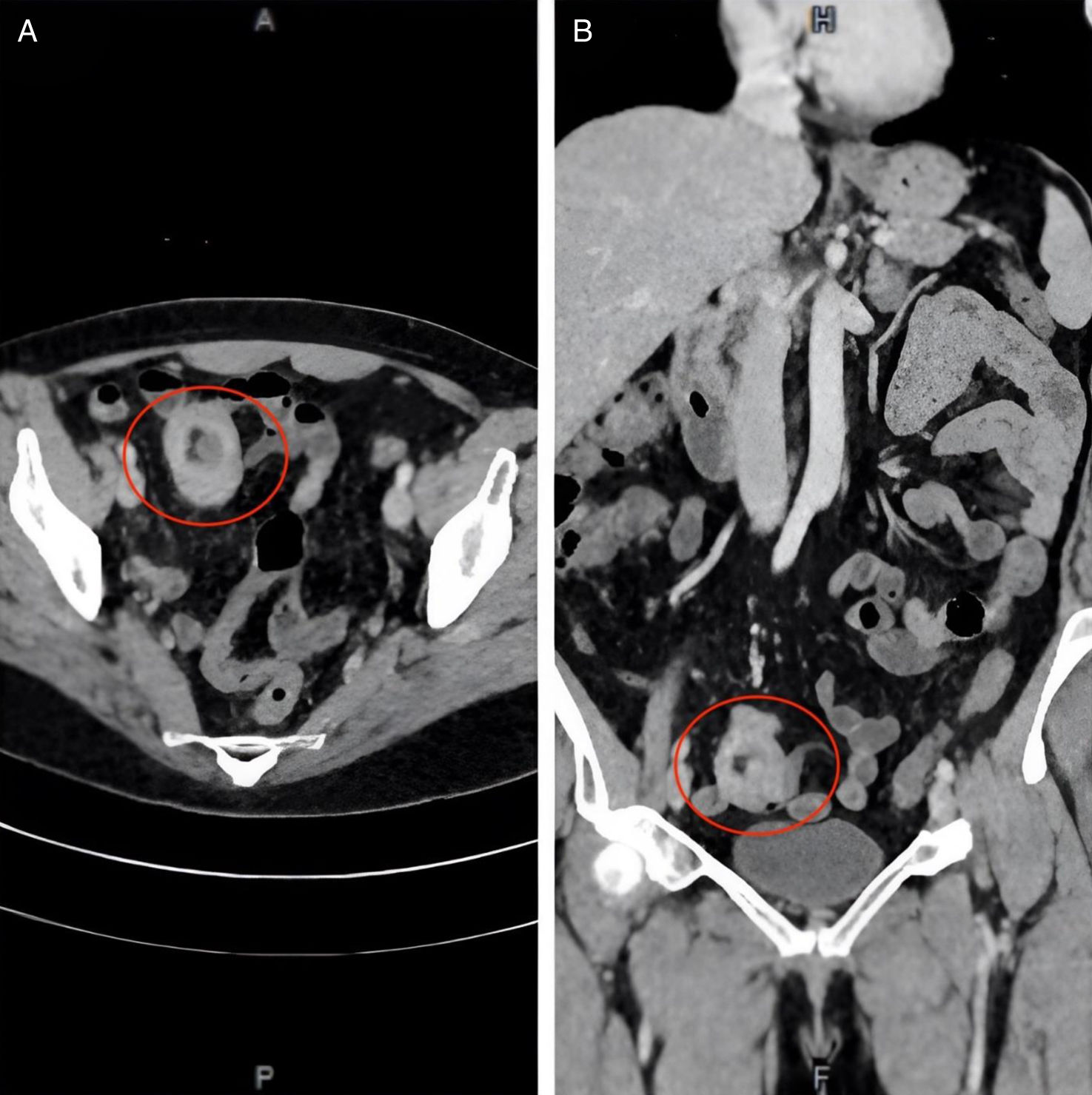
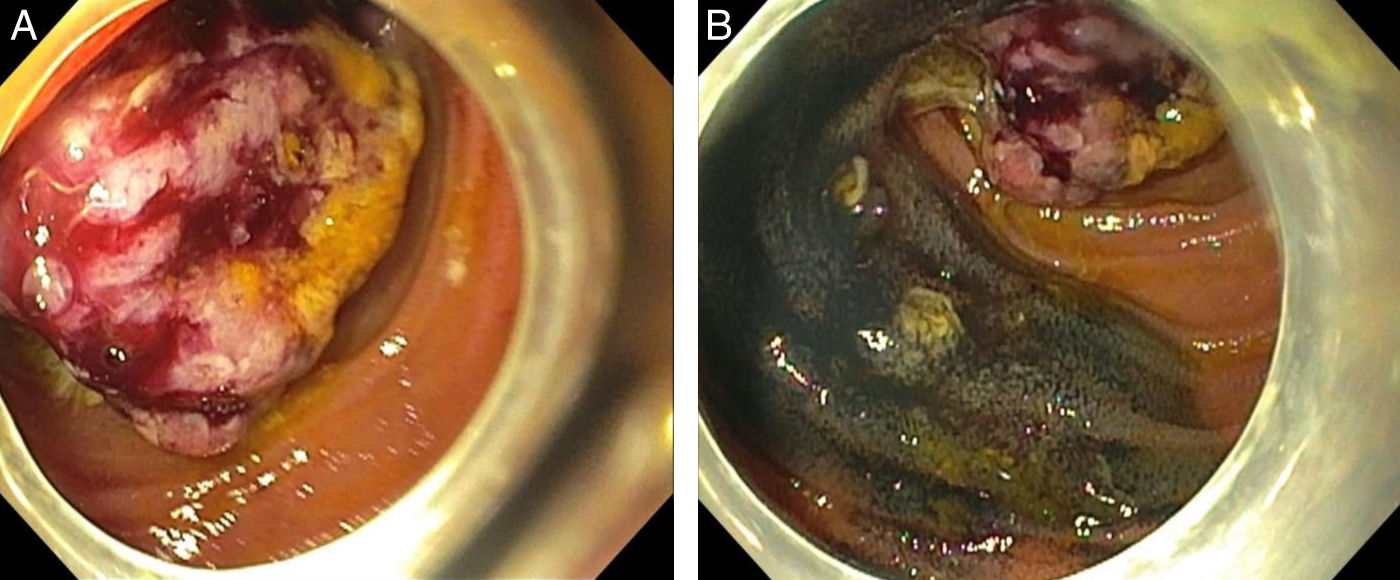
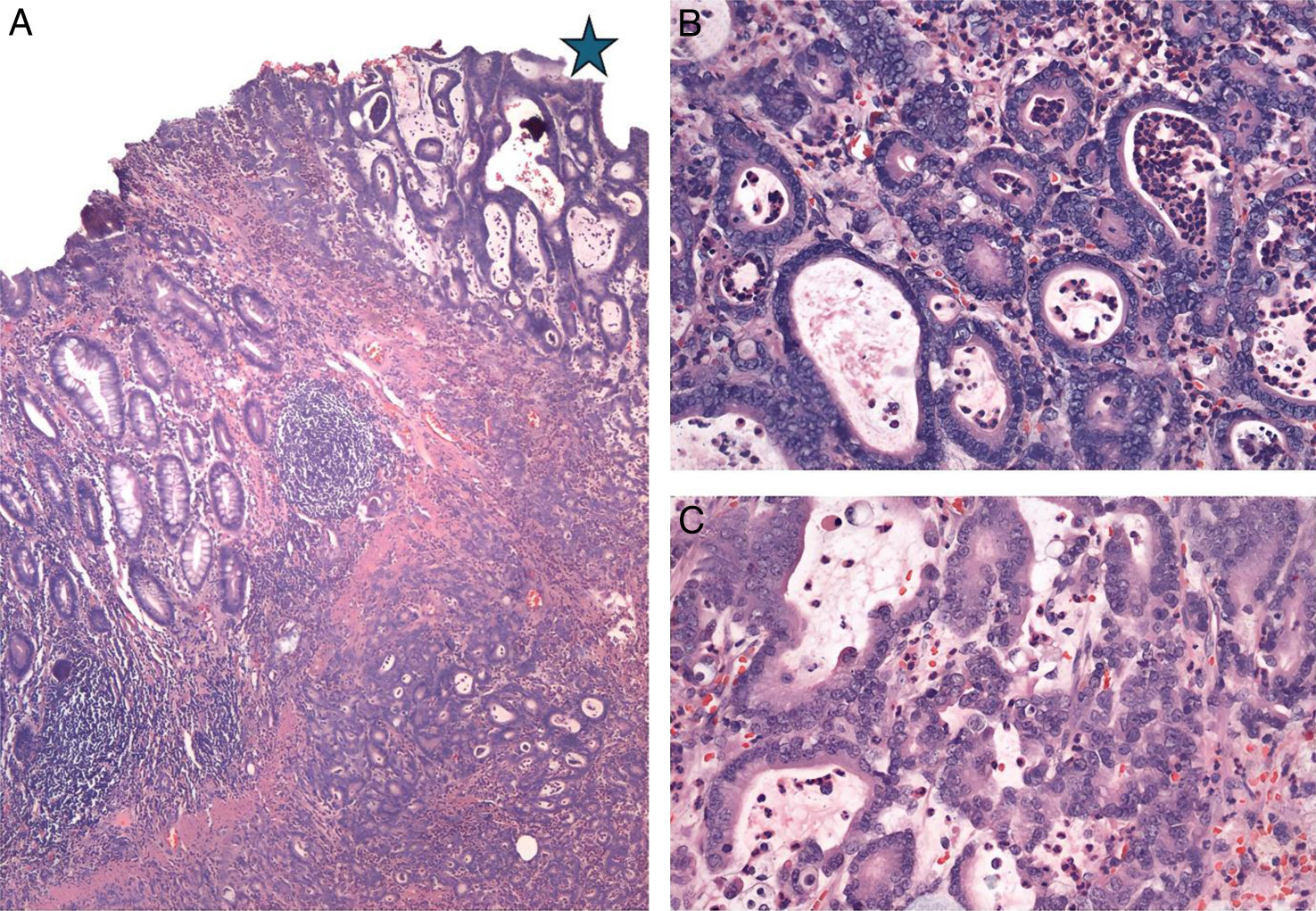
Upon her arrival at the emergency service, the patient was stable, with vital signs within normal parameters. She stated having nonradiating abdominal pain of moderate intensity in the right iliac fossa, nausea, vomiting of gastric content, and hematochezia. She received symptomatic treatment with no clinical improvement. Physical examination revealed an unaltered abdomen. In her laboratory tests, hypochromic microcytic anemia stood out and the rest were within normal parameters. Abdominal computed tomography with intravenous contrast identified bowel occlusion, with intussusception at the level of the terminal ileum and a polyp in its interior (Fig. 1A [axial view] and B [coronal view]). As part of the approach, retrograde single-balloon enteroscopy was performed, revealing an indurated, friable, fibrin-covered exophytic lesion with mucous and vascular pattern loss that involved more than 80% of the lumen (Fig. 2A and B). Biopsies were taken and the adjacent area was marked with India ink. The histopathologic report was received later and was consistent with primary adenocarcinoma of the ileum (Fig. 3A [asterisk], B, and C). Extension studies were performed that documented enhancement only at that level. As part of the treatment, laparoscopy with intestinal resection, guided by the previously marked India ink tattoo, was performed. An extracorporeal mechanical side-to-side anastomosis was carried out, reporting a 2 × 2 cm tumor, with no invasion into adjacent structures, and malignancy-free margins. The patient was evaluated by the oncology service and later discharged with no eventualities. She is currently asymptomatic, and her progression is good. Follow-up will be carried out at the oncology service.
Pathology: Moderately differentiated small bowel adenocarcinoma. (A) Slide showing intestinal mucosa inflammation (left) and the transition to adenocarcinoma (right/asterisk). Hematoxylin and eosin staining ×200. (B and C) Neoplastic glands of adenocarcinoma, with altered architecture, cytologic atypia, and accentuated acute and chronic inflammation. Hematoxylin and eosin staining ×400.
Small bowel adenocarcinoma accounts for 30–40% of primary cancers of the small bowel. It has a poor prognosis, compared with other tumor subtypes, with a 10% survival rate for stage IV disease. Approximately 50% of small bowel adenocarcinomas are in the duodenum, 30% in the jejunum, and 15% in the ileum. The disease is usually associated with advanced age, inflammatory bowel disease (IBD), and celiac disease, as well as hereditary syndromes, such as Peutz-Jeghers syndrome, familial adenomatous polyposis, or Lynch syndrome.5 In the ileum, incidence has been reported from 7 to 17% of all tumors, representing 0.06% of new cancer cases in the United States, most presenting with metastasis. Prognosis is poor. If the disease is localized, five-year survival varies from 30 to 79% and if metastatic, from 3 to 19%.6 Clinical presentation is highly nonspecific, ranging from nausea (16%) and abdominal pain (43%) to gastrointestinal bleeding (7%). Given that symptoms are vague, diagnosis is usually delayed and may take up to eight months after starting the approach. Diagnosis is generally made through imaging studies (computed tomography, magnetic resonance imaging) and complemented with endoscopic studies for taking biopsies or with surgery. Treatment should be multidisciplinary and include oncology consultation but the cornerstone of treatment for localized disease is surgery.7 In the case presented herein, we found a tumor in its early clinical stage. The diagnostic approach was carried out with endoscopy and the diagnostic/therapeutic approach with minimally invasive surgery that will most likely be curative, improving patient prognosis, given that the survival rate is nearly 80% for localized disease.
Ethical considerationsInformed consent was required for participation in the present written research. All individuals who enter the hospital as patients sign a privacy notice that authorizes the use of their personal data for research purposes and the consent for surgery also includes a section for using data for research. This work meets the current bioethical research regulations and the norms of the Research and Ethics Committee for Studies on Humans (CEIEH) of the Hospital Médica Sur, but as a case report, its submission was not necessary. The authors declare this article contains no personal information that could identify patients.
Financial disclosureNo type of financing was involved in this publication given that the only resources utilized were those provided by the hospital, such as the clinical record.
There were no financial or personal relations associated with the publication of this article that could lead to a conflict of interest.