Chronic pancreatitis (CP) is characterized by chronic inflammation, fibrosis, and irreversible scarring that results in the loss of both exocrine (acinar) and endocrine (islet cells) pancreatic tissue1.
Etiology can be toxic-metabolic (alcohol, tobacco, medications, etc.), idiopathic, genetic, autoimmune, obstructive, or due to episodes of recurrent acute pancreatitis2.
CP causes healthy parenchyma to be substituted with fibrous connective tissue, resulting in increased density, atrophy, calcification, pseudocysts, and irregularities in the main pancreatic duct (MPD) and its branches. Complications of CP are stricture of the MPD and/or bile ducts, pseudocysts, pancreatolithiasis, duodenal stricture, malnutrition, vascular complications, and recurrent pain3.
Stones in the MPD cause an increase in the pressure of the parenchyma, as well as ischemia and chronic abdominal pain4.
Endoscopic management focuses on resolving MPD obstruction through dilation or stent placement, in the case of MPD stricture, or through the removal of stones5.
Surgical options include drainage, resection, resection with extended drainage, pancreatic denervation alone, or islet autotransplantation. The choice of the procedure depends on the morphologic changes of the pancreas (dilation of the MPD, stricture, lithiasis)6.
Studies conclude that surgical treatment is more efficacious and longer lasting than endoscopic treatment7–9. At present, the ideal time for surgical intervention is not known. Nealon et al. suggest that early surgical decompression of the MPD delays the progressive destruction of the pancreas8.
The modified Puestow procedure consists of a side-to-side longitudinal pancreaticojejunostomy of at least 10 cm, with no resection of the pancreatic tail or the pancreas. It is indicated in patients with MPD dilation > 7 mm, a “chain of lakes”, and no inflammatory mass in the pancreatic head. Pain relief resulting from that surgery has been shown to be around 60–70%10.
Case 1A 47-year-old man had a past medical history of chronic alcoholism and type 2 diabetes mellitus, both of 10-year progression. He presented with a high risk for choledocholithiasis. Endoscopic retrograde cholangiopancreatography (ERCP) was performed, revealing common bile duct stricture, and an endostent was placed. Later, the patient presented with pain, and an endoscopic ultrasound (EUS) study was carried out that identified a dilated MPD (10 mm), with multiple intraductal stones, calcifications in the pancreatic parenchyma, atrophy of the pancreatic head and tail, and dilation of the intrahepatic and extrahepatic bile ducts. Laparoendoscopic modified Puestow procedure plus cholecystectomy was performed. Oral diet was started the same day and the patient was released from the hospital 48 h after the procedure, with no complications.
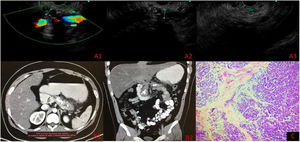
Case 2A 22-year-old man had a past medical history of numerous hospital admissions due to severe acute pancreatitis of biliary origin, from 2017 to the present date (eight hospital admissions). EUS identified signs of CP, MPD dilation, and intraparenchymal calcifications in the head, body, and tail of the pancreas and inside the MPD (Fig. 1A1–A3). Contrast-enhanced abdominal computed tomography scan revealed CP with multiple calcifications (Fig. 1B1–B2). The laparoendoscopic modified Puestow procedure with pancreatic biopsy was performed on September 2, 2021, confirming CP, with extensive fibrosis, associated with chronic inflammation (Fig. 1C). Oral diet was started the same day, in the afternoon, and the patient was released from the hospital 48 h after the procedure, with no complications.
A) Endoscopic ultrasound with main pancreatic duct measurement. A1) Neck 7 mm. A2) Body 10 mm. A3) Tail 3 mm (intraductal calcifications in body and tail). B1-B2) Contrast-enhanced abdominal computed tomography scan. C) Histopathology: chronic pancreatitis with extensive fibrosis associated with chronic inflammation.
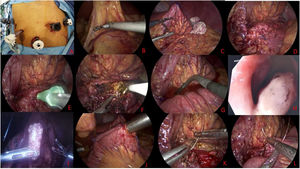
For the approach, a 12 mm supraumbilical camera port was placed; two 12 mm trocars were placed in the left and right midline of the clavicle; and two 5 mm trocars were placed in the anterior axillary line of both flanks (Fig. 2A). The gastrocolic ligament was cut with a Harmonic Ace® scalpel (Ethicon Endo-Surgery Inc.) (Fig. 2B), the omentum was accessed by cutting the short vessels, and the posterior gastric surface was fixed to the parietal peritoneum with a polypropylene GEA extracorporeal knot, to enable exposure (Fig. 2C). The atrophic and hardened pancreas was observed (Fig. 2D) and the main pancreatic duct was punctured, releasing pancreatic fluid (Fig. 2E). A 7 cm long pancreatotomy was made from the neck to the tail and the pancreatic duct was deroofed with a monopolar hook (Fig. 2F). Pancreatoscopy (Fig. 2G) revealed intraductal stones (Fig. 2H) that were then removed. Irrigation with physiologic solution was carried out through a 5 Fr catheter (Fig. 2I). Repeat pancreatoscopy corroborated the absence of ductal stones. A Roux-en-Y 60 cm biliary loop and 50 cm feeding loop were made utilizing an Endo-GIA™ stapler (Covidien, Minnesota, USA) (60 mm staples) (Fig. 2J). The jejunal isoperistaltic loop was lifted in front of the colon (antecolic) and a manual side-to-side pancreaticojejunostomy was performed. Continuous two-layer suturing was carried out with 2-0 polypropylene and reinforced with 2-0 barbed suture at the posterior surface (Fig. 2K) and with continuous 2-0 barbed suture at the anterior surface (Fig. 2L). Jackson Pratt drains were then placed at the posterior and anterior surfaces of the stomach.
A) Trocar placement. B) Opening of the gastrocolic ligament. C) Stomach fixed to the perineum to expose the pancreas. D) Atrophic pancreas. E) Main pancreatic duct puncture. F) Opening of the main pancreatic duct. G) Pancreatoscopy. H) Stones in the main pancreatic duct. I) Stone after its extraction. J) Roux-en-Y formation. K) Posterior wall pancreatojejunoanastomosis. L) Anterior wall pancreatojejunoanastomosis.
A written statement of informed consent was obtained from the patients and responsible relatives, with two witnesses, before the surgical procedure was performed. Given that the present article is a case report and not a research study, authorization from the ethics committee of the Hospital General Dr. Manuel Gea González was not requested. The authors declare that this article contains no personal information of any type that could identify the patients.
Please cite this article as: Brito-Carmona RD, Cuendis-Velázquez A, Carrión-Astudillo CM, Bozada-Gutiérrez KE, García-Manzano RA. Procedimiento de Puestow modificado laparoendoscópico. Reporte de dos casos. Rev Gastroenterol Méx. 2022;87:501–503.