Esophageal melanosis is a rare condition characterized by melanocytic proliferation in the squamous epithelium of the esophagus and melanin accumulation in the mucosa.1 Its etiology and natural course remain uncertain, although some authors suggest a link with chronic inflammation from gastroesophageal reflux disease, which may cause mucosal damage and reactive melanocytic hyperplasia.2 Often identified during endoscopic screening, with an incidence of 0.7-2.1% in upper endoscopies, esophageal melanosis has been proposed as a premalignant condition.3,4 This article reports a case of esophageal melanocytosis.
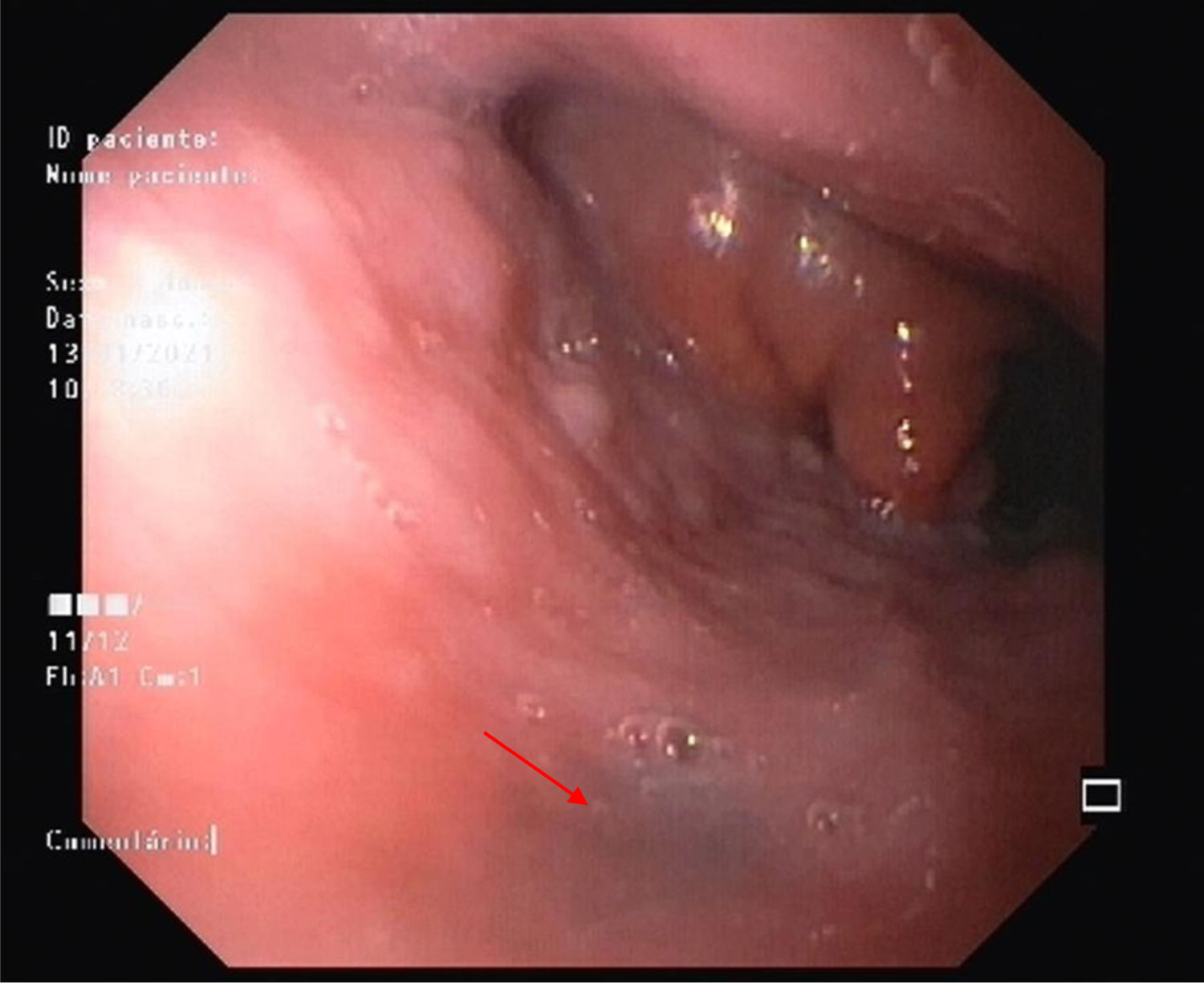
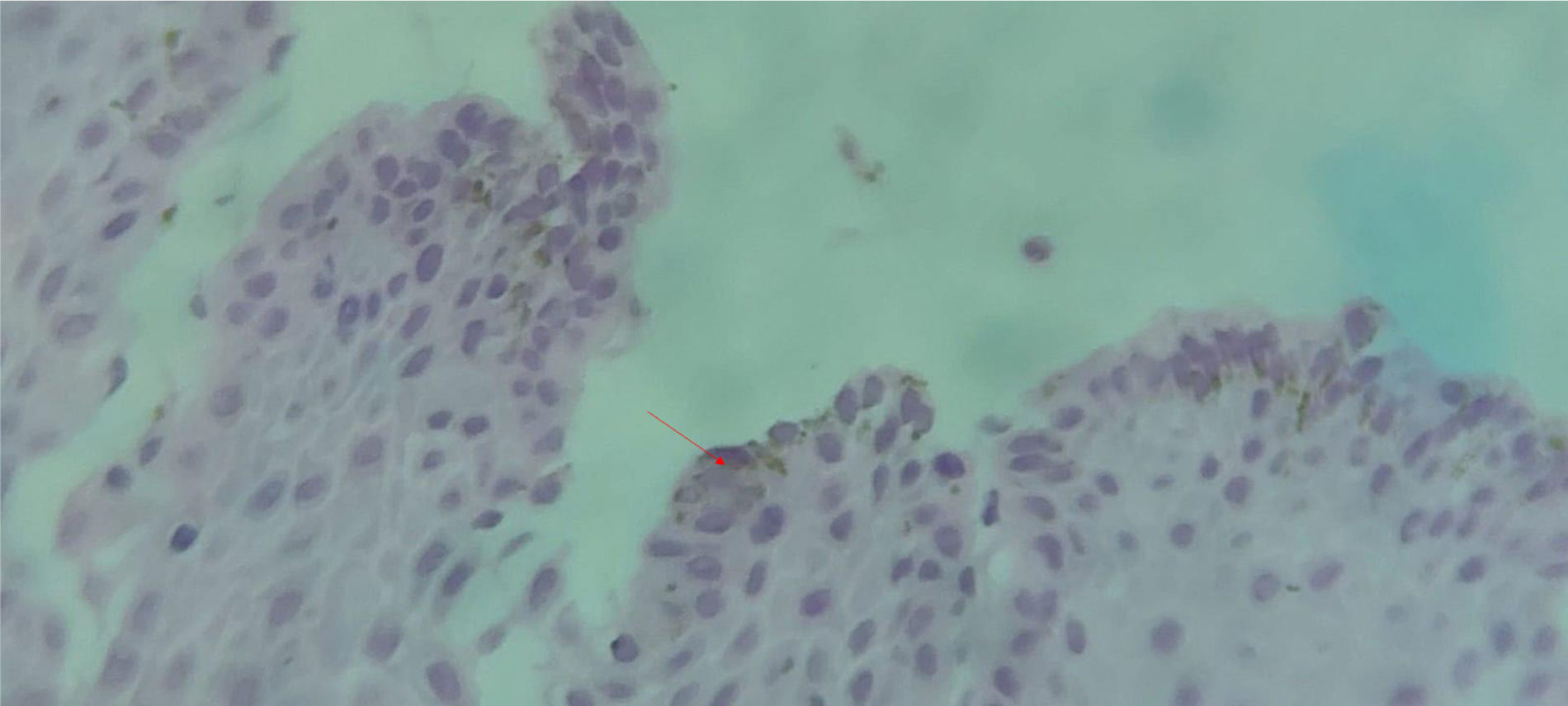
A 67-year-old woman was referred to a gastroenterology consultation after a sessile polyp was found in the gastric antrum during investigation for iron-deficiency anemia. She reported no significant symptoms, such as dyspnea, fatigue, anorexia, weight loss, or gastrointestinal/gynecological bleeding. Her medical history was unremarkable. Examination revealed pale mucous membranes, hemoglobin of 10.2g/dl, and ferritin of 9μg/l. Upper endoscopy showed a black macula, 7-8mm in size, at 32cm into the esophagus (Fig. 1). Biopsies confirmed esophageal melanocytosis, with negative Perls stain (Fig. 2). There were no signs of hyperpigmentation on the skin, eyes, mouth, or genital mucosa. Given the condition’s potential premalignant nature, a follow-up endoscopy was performed one year later and revealed no abnormalities.
Endoscopically, esophageal melanosis appears as a circular, linear, or oval brownish lesion with a smooth surface and irregular borders, usually in the middle or lower esophagus. Histologically, it shows melanocytic proliferation in the squamous epithelium and melanin deposition.1,2
Its origin is unclear, but theories suggest either abnormal melanocyte migration during embryogenesis or keratinocytic hyperplasia from chronic irritation (e.g., alcohol, tobacco, gastric reflux).3 Differential diagnoses include melanocytic nevi and malignant melanoma.4
Endoscopic features distinguish esophageal melanosis from malignant melanoma, which appears polypoid. Histologically, melanosis lacks spindle cells or cytological atypia. Some authors suggest it may be a precursor to dysplasia, melanoma, or esophageal carcinoma, emphasizing the need for clinical and endoscopic surveillance for early neoplasia detection.3
Another consideration in the differential diagnosis is esophageal necrosis, typically ischemic in origin, which presents as circumferential black coloration with friable hemorrhagic tissue and a sharp transition at the gastroesophageal junction.4 Ingestion of corrosive agents can cause esophageal mucosal sloughing and dark discoloration, mimicking melanosis. Benign conditions, such as pseudo-melanocytosis, which involves pseudo-melanin deposition from lysosomal degradation or carbon dust, should be considered before diagnosing esophageal melanosis.2–4
Finally, we emphasize the importance of careful, meticulous, and detailed observation of the entire gastrointestinal tract visible during upper digestive endoscopy, which allows for the diagnosis of rare lesions, such as esophageal melanosis.
Financial disclosureNo specific grants were received from public sector agencies, the business sector or non-profit organizations in relation to this article.
Ethical considerationsThe authors declare that this case report contains no personal information that can identify the patient, and so informed consent was not required. Nevertheless, informed consent was obtained for the publication of the present work. In addition, this case report meets the current bioethics research regulations and did not require authorization by the institutional ethics committee because it did not affect the patient’s health.
Author contributionsAll authors have read the manuscript and agree with the version to be published.