Chronic pancreatitis is a progressive fibroinflammatory disease that, in addition to causing exocrine pancreatic insufficiency and endocrine alterations, is painful in the majority of cases.
Current symptomatic chronic pancreatitis management is scaled. It begins with lifestyle changes and analgesics and can end in the need for surgery. Endoscopic treatment is a less invasive option than surgery and is considered first-line therapy, together with extracorporeal shock wave lithotripsy (ESWL), when there is main pancreatic duct obstruction at the level of the head or body of the pancreas due to a stone.1,2
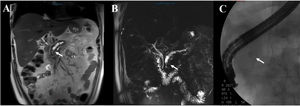
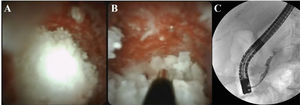
A 58-year-old man presented with chronic pancreatitis, experiencing persistent abdominal pain and recurring symptoms of acute pancreatitis for several years. He had a surgical history of laparoscopic cholecystectomy and no personal history of significant alcohol consumption. In his most recent episode of acute pancreatitis, a stone that appeared to be located in the intrapancreatic common bile duct was reported on an abdominal computed tomography scan. The patient was referred to our hospital to undergo endoscopic retrograde cholangiopancreatography (ERCP). The approach was complemented with magnetic resonance cholangiography, revealing that the stone was actually located in the main pancreatic duct at the level of the head of the pancreas, with pancreatic duct dilation (Fig. 1A and B). The decision was made to extract the pancreatic stone through conventional ERCP. After cannulating the pancreatic duct, a 0.035” guidewire was advanced until coming up against a 7 mm radio-opaque stone that did not allow further advancement, preventing the completion of the procedure as it had been planned (Fig. 1C). Sphincterotomy was carried out and a temporary 5 Fr pancreatic plastic stent was placed. As a second intervention, at a different time, ERCP was performed, together with a single operator pancreatoscopy (SpyGlass™ DS System). To facilitate the insertion of the device, sphincteroplasty with hydraulic balloon dilation, 8 mm in diameter and 3 cm in length, was carried out, enabling its advancement into the main pancreatic duct. Once the probe (Autolith™Touch Biliary EHL System) was 1 mm from the stone, electrohydraulic lithotripsy was performed (at a 50-watt energy configuration and 10/sec frequency), until the stone was fragmented into very small pieces that were then removed from the pancreatic duct with a 9 mm/12 mm extraction balloon (Fig. 2, complementary video: shortened ERCP and pancreatoscopy procedure). A prophylactic 5 Fr × 7 cm pancreatic plastic stent was placed, thus completing the procedure. No complications associated with the intervention were reported and at his latest consultation, five months after the procedure, the patient stated he had no recurrence of pain.
(A and B) Magnetic resonance cholangiography showing main pancreatic duct dilation up to 8 mm, with a serpiginous tract and sudden caliber reduction at the level of the head of the pancreas, associated with an intraluminal hypointense image (arrow). (C) Fluoroscopy showing a radio-opaque stone in the topography of the head of the pancreas (arrow).
Endoscopic treatment for managing main pancreatic duct obstruction is effective in adequately evaluated patients. Stones smaller than 5 mm or radiolucent stones located in the head or body of the pancreas can be managed through conventional ERCP, utilizing a balloon or basket. For radio-opaque stones larger than 5 mm, management with ESWL is suggested, but its high cost and low availability are limitations.1 Pancreatoscopy-guided lithotripsy (PGL) is another endoscopic treatment option in such cases. Pancreatoscopy enables direct stone visualization, facilitating more precise fragmentation and confirming the complete cleaning of the pancreatic duct; concomitant strictures can also be evaluated. The combination of ERCP and pancreatoscopy tends to be more successful that ERCP alone.3,4 The pancreatoscope has a very small diameter and can be inserted through the working channel of the duodenoscope. Likewise, the pancreatoscope has its own working channel, through which special accessories can be introduced, such as the lithotripsy probe. Both laser PGL and electrohydraulic PGL are performed at a distance of 0.5 mm from the stone and do not make contact with it. Prophylactic antibiotic use is recommended in all cases.5,6
PGL is considered by many to be second-line endoscopic treatment because it is a much more complex procedure than ESWL, and information on the modality is still scarce. In a systematic review, the stone fragmentation success rate was 85.77%, achieving complete fragmentation in 62.05% of cases. The severe adverse effect rate was reported at 4.84%. No significant differences were found in the comparison of electrohydraulic lithotripsy and laser lithotripsy, with respect to fragmentation success and adverse effects.7
In a recent study that evaluated electrohydraulic PGL as first-line treatment for such cases, stone resolution was 70.6%. Impossibility of achieving adequate access to the pancreatic duct was one of the main limitations for completing the procedures. Taking into account only the cases in which adequate access to the pancreatic duct was achieved, the technical success rate was 92.3%. There was also a significant decrease in the pain scale scores. Pancreatitis presented in 28% of the cases, all of which were mild.8
In conclusion, PGL is a treatment option to consider in selected cases of chronic pancreatitis, when symptom control through medical management is insufficient.
Ethical considerationsThe authors declare that they followed the bioethics protocols of their work center regarding the publication of patient data. Given the type of publication, no evaluation by an ethics committee was required. The authors declare that this article contains no personal information of the patient and that he gave his informed consent for this publication.
Financial disclosureNo financial support was received in relation to this article.
Author contributionsDrafting of the manuscript: PVH, FRV; data collection: PVH, IFA; video editing: FRV; manuscript review: FRV, ROA, JFML.
Conflict of interestThe authors declare that there is no conflict of interest.
Please cite this article as: Valdez-Hernández P, Romero-Vallejo F, Molina-López JF, Olavide-Aguilar R, Fonseca-Rodríguez I. Litotripsia electrohidráulica guiada por pancreatoscopia para el manejo de obstrucción del conducto pancreático principal por lito. Rev Gastroenterol Méx. 2023;88:179–181.