Currently there is no ideal diagnostic/therapeutic approach for patients with suspected choledocholithiasis. The primary aim of our study was to evaluate the performance of the criteria for predicting choledocholithiasis proposed by the American Society for Gastrointestinal Endoscopy (ASGE) in 2019.
Materials and methodsA retrospective study was conducted that included 352 patients seen at a secondary care public healthcare institution in Monterrey, Nuevo León, that treats an open population and does not have endoscopic ultrasound or magnetic resonance cholangiopancreatography at its disposal.
ResultsThe most frequent predictor presented by the patients was abnormal liver function tests (90.63%), and with their use alone, sensitivity was higher than that of all the predictors analyzed (91.41%). In addition, the finding of common bile duct stones on ultrasound imaging was the only predictor independently associated with the confirmatory diagnosis of choledocholithiasis. Regarding the general performance of the 2019 criteria, the high-risk category had 68.75% sensitivity, 52.08% specificity, a positive predictive value of 79.28%, a negative predictive value of 38.46%, diagnostic accuracy of 64.20%, and a confirmatory diagnosis of choledocholithiasis in 79.28% of the patients of that risk category.
ConclusionsThe study corroborated that the presence of choledocholithiasis could be predicted using the choledocholithiasis predictors and risk categories proposed by the ASGE, with acceptable accuracy, in accordance with the standards suggested by those same guidelines.
Actualmente no existe un enfoque óptimo, diagnóstico/terapéutico, para los pacientes con sospecha de coledocolitiasis. El objetivo principal del estudio fue evaluar el rendimiento de los criterios propuestos por la Sociedad Americana de Endoscopía Gastrointestinal (ASGE, por sus siglas en inglés) en el año 2019 para la predicción de coledocolitiasis.
Material y métodosCohorte retrospectiva de 352 pacientes de una institución pública de segundo nivel que atiende a población abierta en Monterrey, Nuevo León; la cual no cuenta con ultrasonido endoscópico o colangiorresonancia magnética.
ResultadosSe evidenció que el predictor más frecuentemente presentado por los pacientes fue la alteración en las PFH (90.63%). Por sí solo, su sensibilidad fue la mayor entre todos los predictores analizados en este estudio (91.41%). Por otro lado, el hallazgo de litiasis en el colédoco por ultrasonido fue el único predictor que se asoció de forma independiente con el diagnóstico confirmatorio de coledocolitiasis. En cuanto al rendimiento general de los criterios del año 2019, la categoría de riesgo alto tuvo una sensibilidad del 68.75% y una especificidad del 52.08%; un valor predictivo positivo del 79.28% y un valor predictivo negativo del 38.46%; y una exactitud diagnóstica del 64.20%; se corroboró el diagnóstico de coledocolitiasis en el 79.28% de los pacientes de esta categoría de riesgo.
ConclusionesSe logró corroborar que los predictores de coledocolitiasis y las categorías de riesgo propuestas por la ASGE, permiten predecir la presencia de coledocolitiasis con aceptable precisión, acorde con los estándares sugeridos por la misma guía.
Choledocholithiasis is the most common cause of bile duct obstruction and presents in 10-20% of patients with cholecystolithiasis, 7-14% of patients that underwent cholecystectomy, and 18-33% of patients with acute biliary pancreatitis.1 Despite the fact that the disease can be asymptomatic, it is associated with higher morbidity and mortality rates due to the development of other diseases, such as acute biliary pancreatitis or acute ascending cholangitis.2
The diagnosis of choledocholithiasis is based on the combination of clinical signs and symptoms, alterations in liver function tests (LFTs), and radiologic findings. Those indicators have varying degrees of diagnostic accuracy, and none of them, on their own, is a completely reliable method for identifying bile duct stones.2 Bile duct stone extraction, whether through endoscopic retrograde cholangiopancreatography (ERCP) or surgery (conventional or laparoscopic bile duct exploration [BDE]) is considered the gold standard for its diagnosis.3 However, ERCP is not an innocuous procedure and there is a risk for complications related to its performance, such as post-ERCP pancreatitis in up to 15% of patients, post-sphincterotomy bleeding in 1-2%, perforations, and anesthesia-related adverse events.4 Thus, ERCP should be carried out exclusively for therapeutic purposes.
When there is doubt regarding the diagnosis of choledocholithiasis, endoscopic ultrasound (EUS) and magnetic resonance cholangiopancreatography (MRCP) are highly accurate alternatives, with a low rate of associated risks.5–6 In a systematic review in which diagnostic accuracy with respect to choledocholithiasis was evaluated, 95% sensitivity and 97% specificity were described for EUS and 93% sensitivity and 96% specificity for MRCP, with no significant difference between the two methods.7
Currently, there is no ideal diagnostic/therapeutic approach for patients with suspected choledocholithiasis. A variety of predictive models of choledocholithiasis based on algorithms and diagnostic criteria can be found in the literature, but they are characterized by not providing therapeutic recommendations according to the calculated risk and by not having studies that have evaluated their external validity in populations outside of those in which they were initially developed.8–10
In 2010, The American Society for Gastrointestinal Endoscopy (ASGE) published clinical guidelines defining clinical predictors and risk categories for choledocholithiasis.11 The guidelines were revised and updated and published in 2019 (Table 1). According to the updated guidelines, the “high risk” category is for patients that have a more than 50% probability of presenting with choledocholithiasis and they should directly undergo ERCP. The “intermediate risk” category predicts a 10-50% probability of presenting with choledocholithiasis and those patients should undergo less invasive studies, such as EUS, MRCP, and intraoperative cholangiography (IOC), to evaluate the need for additional therapeutic action. The absence of risk predictors indicates “low risk” or a probability of choledocholithiasis below 10% and those patients can undergo cholecystectomy (conventional or laparoscopic), with no additional evaluations. Due to a lack of correlation, biliary pancreatitis, as a predictive criterion, was removed from the updated guidelines.12
ASGE strategy for assigning risk of choledocholithiasis and management of patients with symptomatic choledocholithiasis, based on clinical predictors.12
| Probability | Choledocholithiasis predictors | Recommended strategy |
|---|---|---|
| High | Common bile duct stone on US/CAT | ERCP |
| or | ||
| Symptoms of ascending acute cholangitis | ||
| or | ||
| Total bilirubin >4 mg/dl and dilated common bile duct on US/CAT | ||
| Intermediate | Altered LFTs | EUS, MRCP, IOC or intraoperative US |
| or | ||
| Age > 55 years | ||
| or | ||
| Dilated common bile duct on US/CAT | ||
| Low | No predictors present | Cholecystectomy with/without IOC or intraoperative US |
ASGE: American Society for Gastrointestinal Endoscopy; CAT: computed axial tomography; ERCP: endoscopic retrograde cholangiopancreatography; EUS: endoscopic ultrasound; IOC: intraoperative cholangiography; MRCP: magnetic resonance cholangiopancreatography; US: ultrasound.
The primary aim of our study was to evaluate the performance of the updated ASGE criteria for predicting choledocholithiasis at a secondary care public health institution in Monterrey, Nuevo León, Mexico, that treats an open population. The hospital does not have the use of EUS or MRCP at its disposal and the patients with suspected choledocholithiasis are treated in a non-standardized manner through cholecystectomy + IOC + BDE; ERCP + cholecystectomy; or cholecystectomy + IOC + intraoperative ERCP, depending on the availability of materials and equipment, surgical time, the decision of the staff surgeons, and the characteristics and general status of the patient. In that context, we sought to validate an efficient diagnostic algorithm for the treatment of choledocholithiasis that can be applied at institutions similar to ours, reducing the performance of tests and/or procedures that are costly and not exempt from complications. Our secondary aims were:
- 1
To evaluate the association of the high-risk and intermediate-risk 2019 ASGE predictors with the presence of choledocholithiasis.
- 2
To compare the performance of the 2010 ASGE criteria with their 2019 updated version.
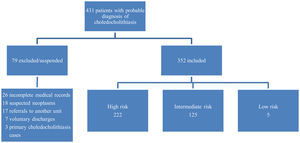
The present study was a retrospective, cross-over, observational, cross-sectional, analytic, and descriptive study. A review of non-probabilistic convenience sampling was carried out. The lists of patients hospitalized within the time frame of January 2016 and September 2019 were analyzed (diagnosis upon admission and discharge) to obtain the medical record number and specific information corresponding to all patients with a suspected diagnosis of choledocholithiasis and/or a diagnosis confirmed by ERCP or BDE (Fig. 1).
Included in the study were patients of either sex and any age that had a history of biliary colic, or clinical symptoms consistent with it, plus any of the following aspects:
- •
Jaundice at hospital admission or having a history of the condition
- •
Abnormal LFTs
- •
Radiologic evidence (US or computed axial tomography [CAT]) of extrahepatic and/or
- •
intrahepatic bile duct dilation (common bile duct > 6 mm)
- •
Radiologic evidence (US or CAT) of bile duct stones
- •
Intraoperative identification of extrahepatic bile duct dilation
- •
Outflow of stones from the cystic duct or common bile duct, intraoperatively or during ERCP
The criteria for exclusion or suspension from the study were:
- •
Acute biliary pancreatitis at admission
- •
Incomplete medical records
- •
Previous cholecystectomy
- •
Preoperative suspicion of hepatobiliary neoplasia
- •
Voluntary patient discharge
- •
Referral to another hospital to complete treatment
With the information obtained from the digital and physical medical records, the following variables were entered into a database:
- •
Age: age of the patients in years at hospital admission
- •
Sex: biologic sex of the patients
- •
Risk for choledocholithiasis: the estimated risk for choledocholithiasis in patients with symptomatic cholecystolithiasis based on clinical predictors of the ASGE, classifying them into low risk, intermediate risk, and high risk (Table 1)
- •
Total bilirubin (TB): total bilirubin value in the LFTs of the patients at admission
- •
Abnormal LFTs: alteration in any of the LFT values of the patients at admission
- •
Dilated common bile duct: common bile duct diameter measured on US at admission, considering common bile duct dilation to measure more than 6 mm
- •
Choledocholithiasis on US: bile duct stones observed on US
- •
Choledocholithiasis: confirmation of bile duct stones through ERCP or intraoperatively (IOC + BDE)
- •
Cholangitis: clinical diagnosis of cholangitis, according to the Tokyo guidelines
- •
Number of predictors: number of ASGE clinical predictors for high risk or intermediate risk of choledocholithiasis
The statistical analysis of the information was carried out using the SPSS® version 21 program. A normality analysis of the numerical or interval variables was carried out through the Kolmogorov-Smirnov test. The Student’s t test for independent samples was employed when distribution was normal, and the non-parametric equivalent (Mann-Whitney U), when it was not. The ordinal variables were compared using the Mann-Whitney U test, and the dichotomous nominal variables, using the chi-square test for homogeneity. The nominal and ordinal variables were expressed through absolute frequencies and relative frequencies and the interval variables through measures of central tendency and dispersion. A multivariate logistic regression analysis was carried out to calculate the odds ratio between each predictor and the presence of choledocholithiasis. Sensitivity, specificity, negative predictive value (NPV), positive predictive value (PPV), and diagnostic accuracy (DA) were evaluated for the high-risk category. Likewise, the sensitivity, specificity, NPV, PPV, and DA were assessed for each predictor of the high-risk and intermediate-risk categories. For all the analyses, statistical significance was set at a p < 0.05.
Ethical considerationsGiven that the present study has a retrospective and observational design, there was no potential harm or risk involved. No changes were made in the diagnostic and/or therapeutic criteria, upon including the study criteria. The data were collected as mentioned above. Likewise, patients were codified to protect their identity. The analysis is considered a non-risk study, in accordance with the General Health Law regarding Healthcare Research Material, Article 17. Statements of informed consent were signed by the patients upon their hospitalization per hospital regulations.
ResultsIn the hospital records from the period of January 2016 to September 2019, a total of 431 probable cases of choledocholithiasis, according to the ASGE criteria, were found. Of those cases, 79 were excluded: 26 incomplete medical records, 18 suspected neoplasms, 17 referrals to another hospital unit, 7 voluntary discharges, and 3 cases of primary choledocholithiasis (cholecystectomy already performed), leaving a total of 352 cases that were adequate for conducting the study (Fig. 1).
The patient sample was made up of 311 women (88.4%) and 41 men (11.6%), and the mean patient age was 35.56 years (SD: 16.25). Choledocholithiasis was confirmed through ERCP and/or intraoperatively in 256 patients (72.73%). Table 2 describes the study patient characteristics.
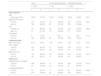
Demographic characteristics of the study patients.
| Total | No choledocholithiasis | Choledocholithiasis | p | ||||
|---|---|---|---|---|---|---|---|
| n = 352 | n = 96 | n = 256 | |||||
| n | % | n | % | n | % | ||
| Clinical picture | |||||||
| Age | |||||||
| Mean age (±SD) | 35.56 | (16.25) | 33.68 | (14.46) | 36.20 | (16.85) | 0.231 |
| Age above 55 years | |||||||
| Yes (%) | 46 | (13.07) | 13 | (28.26) | 33 | (71.74) | 0.872 |
| No (%) | 306 | (86.93) | 83 | (27.12) | 223 | (72.88) | |
| Sex | |||||||
| Women (%) | 311 | (88.40) | 86 | (27.65) | 225 | (72.35) | 0.659 |
| Men (%) | 41 | (11.60) | 10 | (24.39) | 31 | (75.61) | |
| Cholangitis | |||||||
| Yes (%) | 5 | (1.42) | 1 | (20) | 4 | (80) | 0.713 |
| No (%) | 347 | (98.58) | 95 | (27.38) | 252 | (72.62) | |
| Laboratory tests | |||||||
| Mean TB (±SD) | 5.72 | (4.54) | 4.76 | (3.75) | 6.07 | (4.76) | 0.016 |
| TB > 4 mg/dl | |||||||
| Yes (%) | 214 | (60.79) | 51 | (23.83) | 163 | (76.17) | 0.071 |
| No (%) | 138 | (39.21) | 45 | (32.61) | 93 | (67.39) | |
| Abnormal LFTs | |||||||
| Yes (%) | 319 | (90.63) | 85 | (26.65) | 234 | (73.35) | 0.412 |
| No (%) | 33 | (9.37) | 11 | (33.33) | 22 | (66.67) | |
| Ultrasound | |||||||
| Dilated common bile duct | |||||||
| Yes (%) | 299 | (84.94) | 74 | (24.75) | 225 | (75.25) | 0.012 |
| No (%) | 53 | (15.06) | 22 | (41.51) | 31 | (58.49) | |
| Choledocholithiasis | |||||||
| Yes (%) | 75 | (21.31) | 11 | (14.67) | 64 | (85.33) | 0.006 |
| No (%) | 277 | (78.69) | 85 | (30.69) | 192 | (69.31) | |
LFTs: liver function tests; SD: standard deviation; TB: total bilirubin.
The demographic profile of the two groups was homogeneous for sex and age distribution. There were statistically significant differences in patient distribution according to the ASGE risk for choledocholithiasis, TB value at admission, and US evidence of common bile duct stones and a dilated common bile duct. However, that was not reflected in the percentage result of patients with stones confirmed during the surgical procedure of each group. The study included 222 cases with high risk, 125 with intermediate risk, and 5 with low risk.
At hospital admission, the ASGE choledocholithiasis predictors more frequently observed in the study patients were: alteration in the LFTs (90.63%), common bile duct dilation above 6 mm on US (84.94%), and the combination of a TB value above 4 mg/dl and a dilated common bile duct on US (54.55%) (Table 3).
Frequency of choledocholithiasis predictors.
| Predictors | Total (n = 352) | |
|---|---|---|
| n | % | |
| High risk | ||
| Common bile duct stone on US | 75 | 21.31 |
| Clinical ascending cholangitis | 5 | 1.42 |
| Total bilirubin > 4 mg/dl + dilated common bile duct > 6 mm | 192 | 54.55 |
| Intermediate risk | ||
| Abnormal LFTs | 319 | 90.63 |
| Age > 55 years | 46 | 13.07 |
| Dilated common bile duct on US (> 6 mm with gallbladder in situ) | 299 | 84.94 |
| Low risk | ||
| No predictors present | 5 | 1.42 |
LFTs: liver function tests; US: ultrasound.
Regarding the diagnostic capacity of the risk predictors on their own (Table 4):
- •
Common bile duct stones were seen on US in 75 patients, and the diagnosis was confirmed in 64 of them (85.33%), resulting in 25% sensitivity, 88.54% specificity, and 42.33% DA.
- •
Five patients presented with clinical ascending cholangitis, and the diagnosis of choledocholithiasis was confirmed in 4 of them (80%), accumulating a sensitivity of only 1.56%, specificity of 98.96%, and DA of 28.12%.
- •
A total of 192 patients presented with the combination of TB above 4 mg/dl and common bile duct dilation above 6 mm, and 152 of them (79.17%) had choledocholithiasis. That predictor had 59.38% sensitivity, 58.33% specificity, and 59.09% DA.
- •
LFTs were abnormal in 319 patients, and choledocholithiasis was confirmed in 234 of them (73.35%). That predictor was the most sensitive, at 91.41%, with 11.46% specificity and 69.6% DA.
- •
Forty-six patients were above 55 years of age at admission and 33 of them had a final diagnosis of choledocholithiasis (71.74%). The sensitivity of that predictor was low (12.89%), its specificity was high (86.46%), and its DA was 32.95%.
- •
Lastly, imaging studies showed a dilated common bile duct in 299 patients and 255 of them had choledocholithiasis (75.25%). For the imaging study on its own, sensitivity for identifying a dilated common bile duct was 87.89%, specificity was 22.92%, and DA was 70.17%.
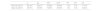
Predictor capacity to diagnose choledocholithiasis.
| S | Sp | PPV | NPV | DA | |
|---|---|---|---|---|---|
| High risk | |||||
| Common bile duct stone on US | 25.00% | 88.54% | 85.33% | 30.69% | 42.33% |
| Clinical ascending cholangitis | 1.56% | 98.96% | 80.00% | 27.38% | 28.12% |
| Total bilirubin > 4 mg/dl + dilated common bile duct > 6 mm | 59.38% | 58.33% | 79.17% | 35.00% | 59.09% |
| Intermediate risk | |||||
| Abnormal LFTs | 91.41% | 11.46% | 73.35% | 33.33% | 69.60% |
| Age > 55 years | 12.89% | 86.46% | 71.74% | 27.12% | 32.95% |
| Dilated common bile duct on US (> 6 mm with gallbladder in situ) | 87.89% | 22.92% | 75.25% | 41.51% | 70.17% |
DA: diagnostic accuracy; LFTs: liver function tests; NPV: negative predictive value; PPV: positive predictive value; S: sensitivity; Sp: specificity; US: Ultrasound.
In the multivariate logistic regression analysis of the predictors, only the finding of bile duct stones on US was independently associated with the confirmatory diagnosis of choledocholithiasis (Table 5).
Association with choledocholithiasis: multivariate analysis.
| Variables | OR | p | 95% CI |
|---|---|---|---|
| High risk | |||
| Common bile duct stone on US | 2.49 | 0.011 | 1.23-5.02 |
| Clinical ascending cholangitis | 2.49 | 0.515 | 0.21-21.69 |
| Total bilirubin > 4 mg/dl + dilated common bile duct > 6 mm | 3.16 | 0.074 | 0.90-11.13 |
| Intermediate risk | |||
| Abnormal LFTs | 1.05 | 0.917 | 0.45-2.43 |
| Age > 55 years | 0.84 | 0.633 | 0.40-1.75 |
| Dilated common bile duct on US (> 6 mm with gallbladder in situ) | 1.13 | 0.773 | 0.48-2.66 |
CI: confidence interval; LFTs: liver function tests; OR: odds ratio; US: ultrasound.
A total of 172 patients were classified as high risk, for presenting with at least one predictor (77.48%), 50 for presenting with 2 predictors (22.52%), and no patient in that category presented with 3 predictors. Seventy-one patients were classified as intermediate risk for presenting with only one predictor (48.80%), 58 presented with 2 predictors (46.40%), and 6 patients presented with 3 predictors (4.80%). The difference between the number of predictors in the patients of each risk category was not statistically significant (Table 6).
Presence of choledocholithiasis according to risk category.
| Total | No choledocholithiasis | Choledocholithiasis | p | ||||
|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | ||
| High risk (%) | 222 | (63.07) | 46 | (20.72) | 176 | (79.28) | 0.000 |
| One (%) | 172 | (77.48) | 40 | (23.26) | 132 | (76.74) | 0.085 |
| Two (%) | 50 | (22.52) | 6 | (12) | 44 | (88) | |
| Three (%) | 0 | (0) | 0 | (0) | 0 | (0) | |
| Intermediate risk (%) | 125 | (35.51) | 50 | (40) | 75 | (60) | 0.000 |
| One (%) | 61 | (48.80) | 26 | (42.62) | 35 | (57.38) | 0.448 |
| Two (%) | 58 | (46.40) | 22 | (37.93) | 36 | (62.07) | |
| Three (%) | 6 | (4.80) | 2 | (33.33) | 4 | (66.67) | |
In accordance with the ASGE criteria, 222 (63.07%) and 125 (35.51%) patients had a high risk and an intermediate risk for choledocholithiasis, respectively. In the high-risk category, choledocholithiasis was confirmed in 176 patients (79.28%), and intermediate risk in 75 patients (60%) (Table 6).
Regarding diagnostic yield, the high-risk category had 68.75% sensitivity, 52.08% specificity, a PPV of 79.28%, an NPV of 38.46%, and DA of 64.20% (Table 7).
Risk category capacity to diagnose choledocholithiasis.
| S | Sp | PPV | NPV | PP | NP | DA | |
|---|---|---|---|---|---|---|---|
| High risk (2010) | 86.72% | 30.21% | 76.82% | 46.03% | 1.24 | 0.44 | 71.31% |
| High risk (2019) | 68.75% | 52.08% | 79.28% | 38.46% | 1.43 | 0.60 | 64.20% |
DA: diagnostic accuracy; NP: negative probability; NPV: negative predictive value; PP: positive probability; PPV: positive predictive value; S: sensitivity; Sp: specificity; US: Ultrasound.
Utilizing the 2010 criteria, choledocholithiasis was confirmed in 222 patients (76.82%) in the high-risk category and 29 patients (50%) in the intermediate-risk category (Table 8). In accordance with the 2010 ASGE guidelines, the diagnostic yield for the high-risk category had 86.72% sensitivity, 30.21% specificity, a PPV of 76.82%, an NPV of 46.03%, and 71.31% DA (Table 7).
2010 vs. 2019 risk category comparison.
| Total | No choledocholithiasis | Choledocholithiasis | ||||
|---|---|---|---|---|---|---|
| n | % | n | % | n | % | |
| ASGE 2010 | ||||||
| High risk (%) | 289 | (82.10) | 67 | (23.18) | 222 | (76.82) |
| Intermediate risk (%) | 58 | (16.48) | 29 | (50) | 29 | (50) |
| ASGE 2019 | ||||||
| High risk (%) | 222 | (63.07) | 46 | (20.72) | 176 | (79.28) |
| Intermediate risk (%) | 125 | (35.51) | 50 | (40) | 75 | (60) |
ASGE: American Society for Gastrointestinal Endoscopy.
The present study is the first in Mexico to evaluate the performance of the updated ASGE guidelines for assigning the risk of choledocholithiasis. Only one other retrospective study that evaluated and validated the clinical usefulness of the new criteria at a tertiary care referral hospital in Hyderabad, India, was found.13
After analyzing the performance of each of the updated guidelines’ predictors, our study patients most frequently presented with abnormal LFTs (90.63%). The sensitivity of that predictor on its own was the highest of all the predictors assessed (91.41%), but its specificity was the lowest (11.46%); its DA was 69.60%. Those findings are consistent with the results of Jagtap et al.13 (Table 9). LFT alteration was one of the biggest changes in criteria between the two publications. In the 2010 guidelines, a TB value between 1.8 and 4 mg/dl was a “very strong” criterion and an alteration in the LFTs other than bilirubin was considered a “moderate” criterion.11 In the updated publication, only a TB value above 4 mg/dl is considered high risk and LFT alteration as intermediate risk.12 By broadening that criterion, in relation to any abnormality in any of the LFT parameters, it would be expected for sensitivity to be higher and specificity to be lower, but in our study that item had the second highest DA, just behind US identification of common bile duct dilation. On the other hand, Al-Jiffry et al. and Prachayakul et al. reported that the only biochemical marker that was useful as a choledocholithiasis predictor was alkaline phosphatase.14,15
Comparison of the diagnostic capacity of each predictor.
| Stone on US | Cholangitis | TB >4 mg/dl +dilated common bile duct >6 mm | Abnormal LFTs | Age > 55 years | Dilated common bile duct >6 mm | |
|---|---|---|---|---|---|---|
| Sensitivity (%) | ||||||
| Ovalle | 25 | 1.5 | 59 | 91 | 13 | 88 |
| Adams et al. 23 | 22 | 17 | ||||
| He et al. 19 | 44 | 1 | 19 | 77 | 60 | 75 |
| Jagtap et al. 13 | 62 | 23 | 43 | 90 | 37 | 70 |
| Magalhaes et al. 22 | 56 | 18 | 90 | 79 | 84 | |
| Rubin et al. 21 | 13 | 7 | 98 | 18 | 58 | |
| Suarez et al. 20 | 14 | 20 | ||||
| Specificity (%) | ||||||
| Ovalle | 89 | 99 | 58 | 12 | 86 | 23 |
| Adams et al. 23 | 94 | 93 | ||||
| He et al. 19 | 97 | 99 | 96 | 50 | 54 | 63 |
| Jagtap et al. 13 | 99 | 99 | 97 | 39 | 69 | 69 |
| Magalhaes et al. 22 | 90 | 97 | 21 | 38 | 49 | |
| Rubin et al. 21 | 98 | 98 | 7 | 86 | 61 | |
| Suarez et al. 20 | 97 | 94 | ||||
| Positive predictive value (%) | ||||||
| Ovalle | 85 | 80 | 79 | 73 | 72 | 75 |
| Adams et al. 23 | 71 | 59 | ||||
| He et al. 19 | 91 | 56 | 78 | 50 | 46 | 57 |
| Jagtap et al. 13 | 98 | 89 | 72 | 35 | 30 | 44 |
| Magalhaes et al. 22 | 92 | 92 | 70 | 72 | 77 | |
| Rubin et al. 21 | 88 | 83 | 57 | 63 | 66 | |
| Suarez et al. 20 | 77 | 70 | ||||
| Negative predictive value (%) | ||||||
| Ovalle | 31 | 27 | 35 | 33 | 27 | 42 |
| Adams et al. 23 | 62 | 58 | ||||
| He et al. 19 | 73 | 61 | 58 | 77 | 67 | 79 |
| Jagtap et al. 13 | 88 | 78 | 90 | 92 | 75 | 86 |
| Magalhaes et al. 22 | 50 | 37 | 51 | 48 | 60 | |
| Rubin et al. 21 | 47 | 45 | 68 | 45 | 53 | |
| Suarez et al. 20 | 62 | 63 | ||||
LFTs: liver function tests; TB: total bilirubin; US: ultrasound.
Common bile duct dilation above 6 mm, on its own, had the highest DA of all (70.17%), with 87.89% sensitivity and 22.92% specificity (Table 9). No statistically significant association was found between a dilated common bile duct on US and the presence of choledocholithiasis. However, the measurement of the dilation of the common bile duct should be interpreted according to the characteristics of the patient, such as age, body mass index, and previous cholecystectomy (those patients were excluded from our study).16 Common bile duct diameter measurement has been reported to vary in the short term, resulting in different measurements on successive tests, possibly secondary to physiologic or pathologic fluctuations in bile duct pressure.17 In addition, some authors report that the common bile duct diameter increases 1 mm every 10 years, from the age of 60 years, resulting in slight dilation in old age.18 For all those reasons, bile duct dilation is not a determining parameter in the diagnosis of choledocholithiasis, requiring other tests for corroborating suspicion.
By combining common bile duct dilation with a TB value above 4 mg/dl, the 2019 guideline-related specificity in our study increased to 52.08% and the PPV to 79.28%, findings consistent with those reported by He et al.19 Nevertheless, that change improved specificity at the expense of sensitivity, expanded the intermediate-risk category, and increased the need for performing EUS or MRCP.12 That criterion had a higher DA (59.09%) for choledocholithiasis than the other high-risk predictors. Its PPV was 79.17%, similar to values from other studies13,19,20 (Table 9). Because its PPV was the lowest in its risk category, perhaps it should be included for the probability stratification of patients in the intermediate-risk category, rather than in the high-risk one.13
Age above 55 years as an independent predictor had a specificity of 86.46% and a PPV of 71.74%, values much higher than those reported in other studies13,19,21,22 (Table 9). Jagtap et al. proposed that if said predictor were removed from the intermediate-risk category, the need for confirmatory diagnostic tests, such as EUS, MRCP, or IOC, would be reduced in 8.6% of the cases.13
The diagnosis of choledocholithiasis was confirmed in 80% of the patients that presented with acute ascending cholangitis, demonstrating its importance as a high-risk predictor, albeit no statistically significant association with the diagnosis of choledocholithiasis was found, which were findings similar to those described in the study by Adams et al.23 As an independent predictor, its sensitivity was the lowest of all (1.56%), but its specificity was the highest (98.96%) (Table 9). Those results could be due to the fact that only 5 patients presented with acute cholangitis in the present study (1.42%).
The multivariate logistic regression analysis of the predictors showed that the finding of common bile duct stones on US was the only risk predictor independently associated with choledocholithiasis, a finding consistent with those of Benites-Goñi et al.2 Likewise, it had 25% sensitivity and 88.54% specificity, similar to the results of Adams et al.23 (Table 9). US is frequently used when choledocholithiasis is suspected, but its DA is operator-related, with a varying sensitivity of 20-80%.24
According to the ASGE guidelines, a patient in the high-risk category has an over 50% probability of presenting with choledocholithiasis.12 In the present study, 79.28% of the high-risk patients had choledocholithiasis. Those results are consistent with the previous studies of Rubin et al., Magalhaes et al., and Sethi et al.21,22,25 Sensitivity for our high-risk group was 68.75%, a value similar to those found by Jagtap et al., He et al., and Rubin et al.,13,19,21 lower than the results of Magalhaes et al. and Sethi et al.,22,25 but higher than the findings by Adams et al. and Suarez et al., who described sensitivity around 50%.20,23 Specificity was 52.08%, reaching a value similar to that reported by Magalhaes et al. and Sethi et al., but lower than the results of the other authors13,19,20,22,23,25 (Table 10).
ASGE guideline performance comparison.
| Total | No choledocholithiasis | Choledocholithiasis | S | Sp | PPV | NPV | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | |||||||
| Ovalle | HR | 222 | 46 | 20.72 | 176 | 79.28 | 69 | 52 | 79 | 38 |
| (ASGE 2019) | IR | 125 | 50 | 40 | 75 | 60 | ||||
| Jagtap et al. 13 | HR | 230 | 24 | 10.43 | 206 | 89.57 | 74 | 96 | 89 | 91 |
| (ASGE 2019) | IR | 678 | 613 | 90.41 | 65 | 9.59 | ||||
| Adams et al. 23 | HR | 179 | 80 | 44.69 | 99 | 55.31 | 47 | 73 | 56 | 65 |
| (ASGE 2010) | Not HR | 319 | 208 | 65.20 | 111 | 34.80 | ||||
| He et al. 19 | HR | 1171 | 70 | 74 | 64 | 79 | ||||
| (ASGE 2010) | IR | 1252 | ||||||||
| Magalhaes et al. 22 | HR | 193 | 39 | 20.21 | 154 | 79.79 | 86 | 56 | 80 | 66 |
| (ASGE 2010) | IR | 73 | 48 | 65.75 | 25 | 34.25 | ||||
| Rubin et al. 21 | HR | 260 | 74 | 28.50 | 186 | 71.50 | 65 | 67 | 72 | 59 |
| (ASGE 2010) | IR | 250 | 148 | 59 | 102 | 41 | ||||
| Sethi et al. 25 | HR | 244 | 59 | 24.18 | 185 | 75.82 | 80 | 44 | 76 | 51 |
| (ASGE 2010) | IR | 92 | 47 | 51.08 | 45 | 48.91 | ||||
| Suarez et al. 20 | HR | 71 | 32 | 45.07 | 39 | 54.93 | 55 | 69 | 55 | 69 |
| (ASGE 2010) | Not HR | 102 | 70 | 68.63 | 32 | 31.37 | ||||
ASGE: American Society for Gastrointestinal Endoscopy; HR: high risk; IR: intermediate risk; NPV: negative predictive value; PPV: positive predictive value; S: sensitivity; Sp: specificity.
The diagnosis of choledocholithiasis was confirmed in 60% of the patients in the intermediate-risk category, which was higher than that expected in accordance with the ASGE guidelines and the previously described studies (5-50%)12,13,20–23,25 (Table 10).
Upon comparing the performance of the 2010 ASGE criteria with their updated 2019 version, with respect to the former, the diagnosis of choledocholithiasis was confirmed in 222 patients (76.82%) in the high-risk category, a slightly lower percentage than that found using the 2019 criteria (79.28%). On the other hand, in the intermediate-risk category, despite the fact that the diagnostic confirmation percentages were similar (50% with the 2010 criteria and 60% with the 2019 criteria), interestingly, fewer than half the total number of patients were classified in the intermediate-risk category with the former criteria prior to diagnostic confirmation (58 versus 125 patients, respectively) (Table 8). That difference in the number of patients classified in each category could have contributed to the apparently higher sensitivity (86.72%) and DA (71.31%) of the 2010 criteria versus the 2019 criteria (Table 7).
The application of the clinical guidelines of the ASGE enabled us to approach the patients by following a risk-benefit model. In the present study, patients in the choledocholithiasis high-risk category reached a DA in accordance with that proposed by the ASGE, which would entail the performance of ERCP, with no additional studies. However, there are still a significant number of high-risk patients that unnecessarily undergo ERCP because the sensitivity and specificity of the current predictors are still below the ideal values. Likewise, in the present study, the percentage of patients with choledocholithiasis that were in the intermediate-risk category was higher than the expected ASGE percentage, signifying that more than the expected number of bile duct stones would be found during IOC, by following those guidelines to the letter. Keeping in mind the significant adverse event rate associated with ERCP and the costs associated with the procedure and its complications, steering our efforts toward reducing the number of diagnostic ERCPs as much as possible is a reasonable endeavor. At any rate, redefining the cutoff point of a 50% probability of choledocholithiasis, for categorizing a patient as high-risk, seems logical.
Our study has certain limitations. First, to maximize the internal validity, the study was restricted to patients with no other abnormality or concomitant biliary disease that could alter the clinical evaluation. Thus, the findings correspond to those of a population with no previous liver or biliary disease and with no history of cholecystectomy. Second, the effect of serial LFTs on the diagnosis of choledocholithiasis was not studied. Nevertheless, two studies showed that the persistent elevation of TB > 4 mg/dl had 86-90% specificity for detecting choledocholithiasis, with very low PPVs (52-71%).21,23 In addition, He et al. showed that clinical decision-making in suspected choledocholithiasis may not be influenced by serial LFTs.19 The third limitation was the retrospective nature of the study. A better approximation of the NPV could be achieved by routinely applying IOC, which would increase the evaluation of the low-risk patients. However, the strength of the study lies in the prediction of choledocholithiasis in the high-risk patient group and in the comparison of the performance of the 2010 and 2019 ASGE criteria.
ConclusionsThe present study confirms that the ASGE choledocholithiasis predictors and risk categories enable the prediction of choledocholithiasis to be made with acceptable accuracy, in accordance with the standards suggested by those same guidelines. Even though our study verified that the updated ASGE criteria achieved higher specificity for detecting choledocholithiasis, an over-number of diagnostic ERCPs will still be performed, if only those criteria are followed. Therefore, our study should be viewed as an initial work for prospectively evaluating associations of choledocholithiasis predictive factors that have over 90% accuracy.
Financial disclosureNo specific grants were received from public sector agencies, the business sector, or non-profit organizations in relation to this study.
Conflict of interestThe authors declare that there is no conflict of interest.
Please cite this article as: Ovalle-Chao C, Guajardo-Nieto DA, Elizondo-Pereo RA. Rendimiento de los criterios predictivos de la Sociedad Americana de Endoscopía Gastrointestinal en el diagnóstico de coledocolitiasis en un hospital público de segundo nivel del Estado de Nuevo León, México. Revista de Gastroenterología de México. 2023;88:322–332.