The SB3 capsule endoscopy system has better image resolution and the capacity to increase the number of images from 2 to 6 frames per second. Small bowel bleeding is the most common indication. The aim To determine if the advances in capsule endoscopy technology increase diagnostic yield in cases of small bowel bleeding, according to the Saurin classification.
Material and methodsA retrospective, observational, analytic, cross-sectional study included 100 SB2 capsule endoscopies and 100 SB3 capsule endoscopies in patients that presented with small bowel bleeding. The findings obtained with both systems were evaluated. The lesions identified by the two capsules were categorized using the Saurin classification. The relation between the lesions identified with the SB3 and those found with the SB2 was identified through a logistic regression analysis.
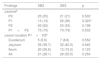
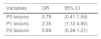
ResultsIn the SB2 capsule endoscopy group, 60% were women, patient age was 59 years (42.2, 73), and intestinal transit time was 271min (182, 353). In the SB3 group, 57% were women, patient age was 60 years (42.5, 73), and intestinal transit time was 277min (182, 352). There were no significant differences in the identification of P0 and P2 lesions between the two systems. The SB3 capsule endoscope identified more P1 lesions (p=0.020, OR: 2.35, 95% CI:1.12-4.90). There was no significant difference in relation to location of the lesions in the small bowel.
ConclusionsA greater number of P1 lesions were detected through the technologic advances made in SB3 capsule endoscopy, but the diagnostic yield for P2 lesions was not modified.
La cápsula endoscópica (CE) SB3 tiene una mejor resolución de imágenes y capacidad para incrementar de 2 a 6 imágenes obtenidas por segundo. La hemorragia de intestino delgado (HID) es la indicación más común. El objetivo fue determinar si los avances tecnológicos de la CE incrementan el rendimiento diagnóstico en HID de acuerdo a la clasificación de Saurin.
Material y métodosEstudio transversal, observacional, retrospectivo y analítico que incluye 100 SB2 y 100 SB3 en pacientes con HID. Se valoraron los hallazgos obtenidos por ambas CE. Se utilizó la clasificación de Saurin para englobar las lesiones identificadas en las CE. Se realizó una regresión logística para identificar la relación de las lesiones detectadas con la CE SB3 en comparación con la SB2.
ResultadosEn el grupo de CE SB2 el 60% eran mujeres, edad de 59 años (42.2, 73) y un tiempo de tránsito intestinal de 271minutos (182, 353). En el grupo de SB3, el 57% eran mujeres, edad de 60 años (42.5, 73) y el tiempo de tránsito intestinal de 277 minutos (182, 352). No se encontraron diferencias significativas para la identificación de lesiones P0 y P2 con ambas CE. La CE SB3 identificó más lesiones P1 (p=0.020) y una razón de momios de 2.35 (IC 95%; 1.12-4.90). No hubo diferencia significativa por la localización de las lesiones en el intestino delgado.
ConclusionesLos avances tecnológicos permiten a la CE SB3 detectar mayor número de lesiones P1, sin modificar en el rendimiento diagnóstico de las P2.
First-generation capsule endoscopy (CE) was described in 2000,1 after which each generation has been improved through technologic advances. Compared with the first-generation system, or SB, the second-generation system, known as the PillCam SB2, provided a larger field of vision, autonomic light control, and a new lens that resulted in better visualization of the mucosa.2 A new version of the second-generation system, called SB2-ex, extended battery duration by 4hours, for a total battery life of 12hours.3 The latest version of CE is the PillCam SB3, which offers a 30% improvement in image resolution, compared with its predecessor.4 It also has the capacity to increase the number of photographic frames from 2 to 6 per second in relation to the speed at which the capsule endoscope moves in the small bowel.
The numerous indications for CE in the study of the small bowel include small bowel bleeding (SBB), Crohn's disease, polyposis, diarrhea, the search for tumors,5 and more recently, graft-versus-host disease of the gastrointestinal tract.6 Nevertheless, SBB continues to be the most common indication for CE.7 The aim of the present study was to identify whether the technological advances of the PillCam SB3 modified the diagnostic yield of CE in patients with SBB, compared with the PillCam SB2.
Materials and methodsThe present study included the first 100 PillCam SB3 CEs carried out in patients with SBB8 at the Endoscopy Service of the Hospital de Especialidades del Centro Médico Nacional Siglo XXI and compared them with the last 100 PillCam SB2 CEs in patients with the same diagnosis. All the patients had undergone upper gastrointestinal endoscopy and colonoscopy that showed no signs of lesions explaining the bleeding. None of the patients had undergone a previous CE or enteroscopy. The CEs in which complete visualization of the small bowel was not achieved, as well as those that identified the cause of the bleeding in an area of the digestive tract other than the small bowel, were excluded.
The patients underwent bowel preparation one day prior to the examination with 4 liters of polyethylene glycol and fasted for 8hours before swallowing the capsule endoscope. The data recorders and belt of the CE system were removed 12hours after their placement, or sooner if the capsule was expelled. The Rapid 8 system was employed for the CE readings and all were reviewed by the same endoscopist, whose experience included the reading of more than 300 CEs, prior to those included in the present analysis.
Age, sex, bowel transit time, and the findings and their locations were documented. Utilizing the Saurin classification,9 the lesions identified in the CE readings were divided into: P0, or normal CE, which included lesions with no bleeding potential, such as diverticula with no signs of bleeding or nodules; P1, which were lesions with an uncertain bleeding potential, such as erosions or red spots; and P2, which included lesions with a high bleeding potential, such as ulcers, angioectasias, and tumors.
The statistical analysis was carried out using the SPSS version 22 program. The quantitative variables were freely distributed, and so the median was used as the measure of central tendency and interquartile ranges as the measure of dispersion. The Mann-Whitney U test was utilized to compare the quantitative variables in the 2 CE systems. The qualitative variables were expressed through frequencies and percentages and they were compared in the CE systems through the chi-square test, obtaining the odds ratio for the Saurin classification. Because the present analysis was a retrospective study that included only the evaluation of CE results, there was no need for it to be examined by the Review Committee of the Hospital de Especialidades del Centro Médico Nacional Siglo XXI. In addition, the present study followed the guidelines of the Declaration of Helsinki.
To determine the size of the study sample, we used the article by Monteiro et al.,10 in which they identified the major duodenal papilla in 42.7% of the patients with the PillCam SB3 system and in 24% with the PillCam SB2. The Fleiss formula was employed to compare 2 proportions, using the CDC EpiInfo version 3.2.1 program, producing a sample size of 99 patients per group. We decided to close each group at 100 patients in the present study.
ResultsTwo hundred CEs performed on the same number of patients with SBB were included in the study. One hundred were carried out with the PillCam SB2 and the other 100 with the PillCam SB3. Sixty percent of the PillCam SB2 CEs were performed on female patients, the median patient age was 59 years (42.2, 73), and the median bowel transit time was 271minutes (182, 353). The time between the last bleeding event and the placement of the SB2 capsule was 12 days (4,10). Fifty-seven percent of the PillCamSB3 CEs were carried out on women, the median patient age was 60 years (42.5, 73), and the median bowel transit time was 277min (182, 352). The time between the last bleeding event and the placement of the SB3 capsule was 13 days (5,18). There were no statistically significant differences in the population characteristics of the two groups (Table 1).
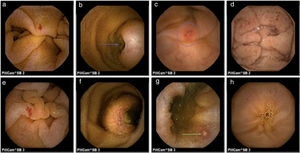
In relation to the findings, P0 lesions were found in 25 SB2 CEs and in 21 SB3 CEs (p=0.502). P1 lesions were identified in 13 SB2 CEs and in 26 SB3 CEs, resulting in a statistically significant difference between the two systems (p=0.020), with an odds ratio of 2.35 (95% CI: 1.12-4.90). P2 lesions were found in 62 SB2 CEs and 53 SB3 CEs, with no significant difference between the two CE systems (p=0.198) (Tables 2 and 3). There were no significant differences between the two systems upon dividing the P2 lesions into ulcer, angioectasia, or tumor subgroups (figs. 1a-h), nor in relation to lesion location in the small bowel when divided into the subgroups of duodenum (p=0.552), jejunum (p=0.645), ileum (p=0.123) or 2 or more regions of the small bowel (p=0.250).
Capsule endoscopy findings.
The technologic advances that have been made in CE are obvious to the endoscopist through the greater image resolution produced by the SB3 capsule, compared with that of the previous generations. However, that improvement is not reflected in the diagnostic yield of all lesion classifications. We observed an increase in the detection of P1 lesions, made up of erosions and red spots, but not in P2 lesions, which include ulcers, angioectasias, and tumors. Perhaps that was due to the fact that P1 lesions are smaller and require greater resolution for their detection than P2 lesions. Xavier et al.11 also compared SB3 CE with SB2 CE and observed no significant differences in the identification of ulcers, angioectasias, and tumors between the two systems. They found that SB3 CE identified more villous atrophy than the SB2 capsule (p=0.03). Those are also subtle changes in the mucosa that require better image definition.
The therapeutic impact of the P1 lesions is 23% versus 61% in the P2 lesions.12 P1 lesions, mainly erosions, can be identified in up to 20% of CEs.13 However, their bleeding potential is uncertain and even though the erosions are mainly related to the use of nonsteroidal anti-inflammatory drugs, they have also been observed in patients that do not use them.9
Another modification presented by the SB3 capsule is the increase in the number of images obtained. It has a velocity sensor that increases the frames per second from 2 to 6 when it detects that the capsule is moving more quickly. That could have an influence on the detection of more lesions in the duodenum and jejunum because the capsule endoscope moves at a greater speed in those regions than in the ileum.14 Monteiro et al., 11 observed a significant difference in the detection of the major duodenal papilla between the SB3 capsule and the SB2 capsule (42.7% vs. 24%, respectively, p=0.015). A slight increase in the detection of lesions in the duodenum and jejunum (7% vs. 5% and 32% vs. 29%, respectively) with the SB3 capsule was found in the present study, compared with the SB2, but it was not statistically significant.
The findings of the present study imply that the detection of lesions with a high bleeding potential was not modified, despite improvement in image resolution and the number of images obtained. However, there was a difference in the detection of lesions with uncertain bleeding potential, such as erosions and red spots. That could modify diagnosis and follow-up, not only in patients that present with intestinal bleeding, but also in those with other small bowel pathologies, such as chronic diarrhea, in which subtle changes in the mucosa can have clinical consequences.15 It is important to conduct prospective studies to identify the implications of that type of lesion on the small bowel. The main limitation of the present study was its retrospective design and the fact that it was conducted at a single hospital center.
ConclusionsThe technologic advances made in the SB3 CE system enabled the identification of a higher number of P1 lesions (erosions and red spots) but did not modify the diagnostic yield in the detection of P2 lesions (ulcers, angioectasias, and tumors), when compared with the SB2 system. Likewise, there was also an increase in the detection of lesions in the duodenum and jejunum, but the difference was not statistically significant. New prospective studies with a larger number of patients are needed to confirm whether the advances made in CE increase the diagnostic yield in patients with SBB.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Financial disclosureNo financial support was received in relation to this study/article.
Conflict of interestThe authors declare that there is no conflict of interest.
Please cite this article as: Blanco-Velasco G, Solórzano-Pineda OM, Mendoza-Segura C, Hernández-Mondragón O. Pillcam SB3 vs. Pillcam SB2: ¿pueden los avances tecnológicos de la cápsula endoscópica mejorar el rendimiento diagnóstico en pacientes con hemorragia de intestino delgado? Revista de Gastroenterología de México. 2019;84:467–471.