Primary pancreatic lymphoma (PPL) is a rare entity. It accounts for approximately 0.5% of pancreatic neoplasias and less than 2% of lymphomas.1 PPL presents more commonly in males and the head of the pancreas is the most frequently affected region.2 The most common histologic type is non-Hodgkin lymphoma. PPL clinical manifestations and radiologic findings must be differentiated from other pancreatic processes, given that its outcome, treatment, and survival differ from those of the rest.3
We present herein a case of PPL diagnosed and treated at our hospital center.
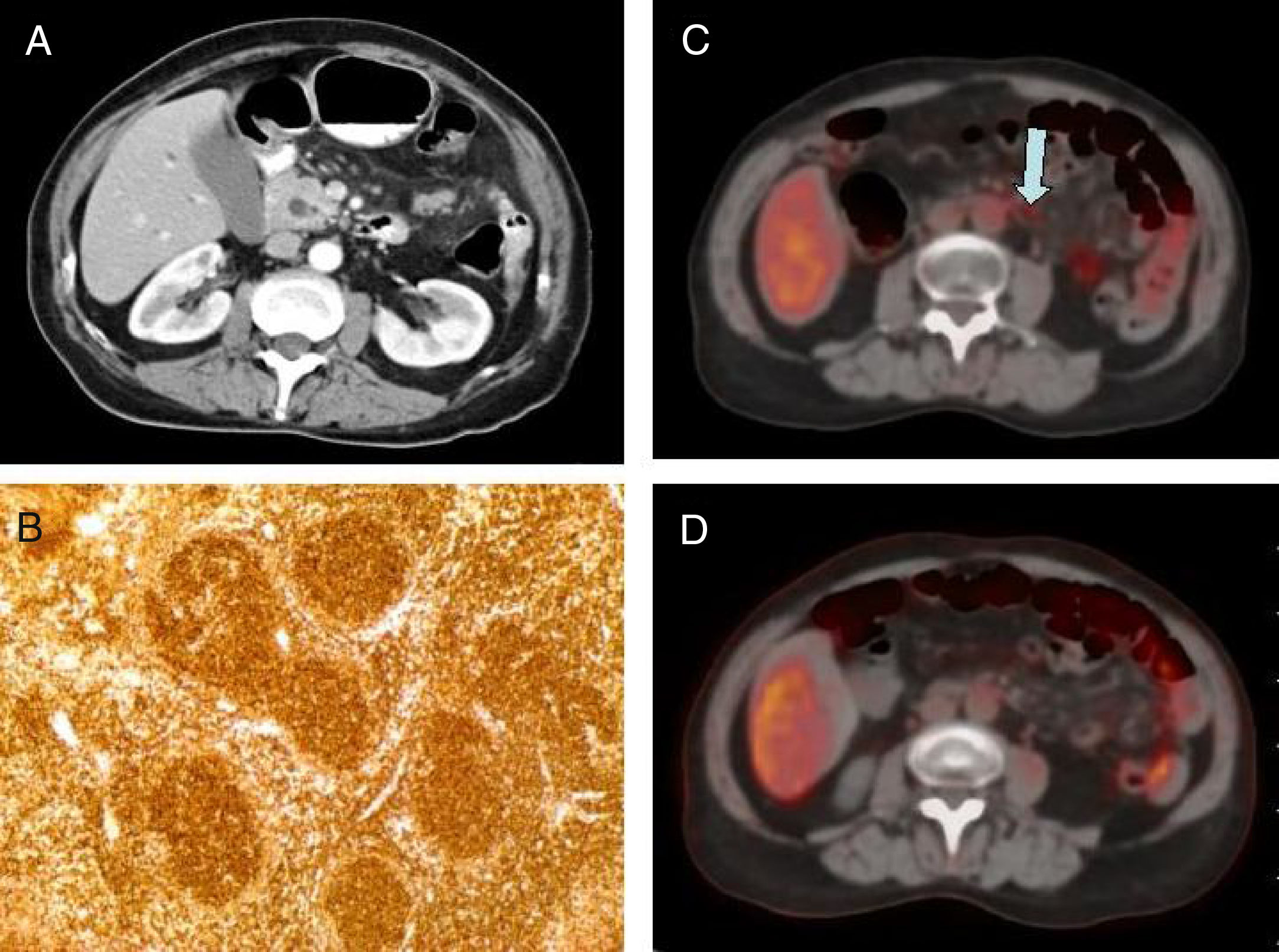
A 53-year-old woman with an unremarkable past history sought medical attention for epigastric pain, malaise, and a 3-kg weight loss within the last month. Physical examination revealed mucocutaneous jaundice and abdominal pain in the epigastrium. Laboratory test results reported total bilirubin 6.03mg/dl, GOT 318 IU/l, and GPT 524 IU/l. An abdominal ultrasound study showed extrahepatic bile duct dilation, with progressive distal narrowing, and a 4 x 3 x 2-cm hypodense mass at the head of the pancreas. A computed tomography scan identified intrahepatic and extrahepatic bile duct dilation, a choledochus with a 17-mm diameter, normal caliber of the duct of Wirsung, and pathologic-appearing adenopathies in the area of the celiac trunk and the mesenteric root (fig. 1A). Endoscopic retrograde cholangiography revealed bulging of the duodenal papilla, suggestive of an ampullary tumor or distal cholangiocarcinoma. A 10-Fr plastic biliary stent was placed, and biopsies were taken of the papilla that were consistent with a nodular lymphoid infiltrate. Given the diagnostic doubt with the complementary studies, the lack of availability of echoendoscopy at our hospital center, and the absence of peripheral lymph node involvement, we decided upon surgical examination to perform lymph node biopsy in the area of the common hepatic artery. The histologic diagnosis was follicular lymphoma (fig. 1B). Extension studies were completed with bone marrow biopsy and flow cytometry, ruling out involvement at other levels. The definitive diagnosis of PPL was made and treatment was begun with chemotherapy (a total of 6 cycles of R-CHOP) and external radiotherapy (a total of 36Gy were administered). The patient presented with clinical and radiologic improvement and jaundice was resolved. The biliary stent was removed at 120 days via endoscopy. At follow-up, after 24 months, a PET-CT scan identified pathologic adenopathy at the mesenteric root (fig. 1C), and bimonthly treatment with rituximab was begun. Later imaging studies revealed complete metabolic response to treatment (fig. 1D). At 48 months from diagnosis, the patient is asymptomatic with no active lymphoproliferative disease.
A) Intravenous contrast-enhanced abdominal CT scan (5-mm axial slice) showing the thickening of the head of the pancreas and dilation of the choledochus. B) Histopathologic study of peripancreatic adenopathy and positive bcl-2, consistent with follicular lymphoma. C) PET/CT (axial view): adenopathy in the hyperenhanced mesenteric root (arrow). D) Control PET/CT after treatment with rituximab (axial view): disappearance of metabolic activity in the adenopathy of the mesenteric root.
Classically, PPL is diagnosed when the following criteria are met: the presence of a mass that predominantly affects the pancreas with peripancreatic lymph node involvement, normal hemogram, and the absence of palpable adenopathies, of mediastinal involvement, and of hepatosplenic metastases.3 The most common clinical manifestations are abdominal pain, weight loss, jaundice, acute pancreatitis, small bowel obstruction, and diarrhea.2
Ultrasound, CT, and NMR are outstanding imaging techniques for aiding in differentiating PPL from adenocarcinoma. Radiologically, PPL is a voluminous tumor, located at the head of the pancreas, with no significant dilation of the duct of Wirsung, and with adenopathies adjacent to the renal veins.4 Generally, PPL is larger than adenocarcinoma, and unlike those tumors, it grows around blood vessels without infiltrating them. The definitive diagnosis is made through histologic study, and endoscopic ultrasound-guided fine needle aspiration (FNA) biopsy is considered the diagnostic method of choice.3 However, because the tissue samples obtained with the conventional aspiration needles are often insufficient for making an accurate diagnosis, FNA has a reduced diagnostic yield for PPLs. Therefore, ProCore® or Shark Tip needles are recommended, given that a larger quantity of tissue can be biopsied, conserving the tissular architecture. When results are inconclusive, surgical biopsy is an alternative that enables an even larger quantity of tissue to be obtained.
Chemotherapy and/or radiotherapy is the treatment of choice for PPL. Cure rates of up to 30% have been reported, with no need for pancreatic resection.3 Rituximab has also been described as an acceptable therapeutic option in cases of non-Hodgkin lymphoma.5
Thus, it is emphasized that PPL should be included in the differential diagnosis any time a pancreatic mass is identified, given that PPL outcome and treatment are very different from those of other such entities.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Financial disclosureNo specific grants were received from public sector agencies, the business sector, or non-profit organizations in relation to this study.
Conflict of interestThe authors declare that there is no conflict of interest.
Please cite this article as: Rodríguez-Infante A, Fernández-Martínez D, Iglesias-García E, García-Flórez LJ. Linfoma pancreático primario como causa de ictericia obstructiva. Revista de Gastroenterología de México. 2019;84:114–115.