Syphilis is a systemic disease caused by the spirochete, Treponema pallidum. Its prevalence is 5 million new cases diagnosed annually and the majority of cases, estimated at 75%, are men that have unprotected anal sex with men.1 Syphilis and human immunodeficiency virus (HIV) coinfection is very common, and its prevalence varies from 45% to 79%.2
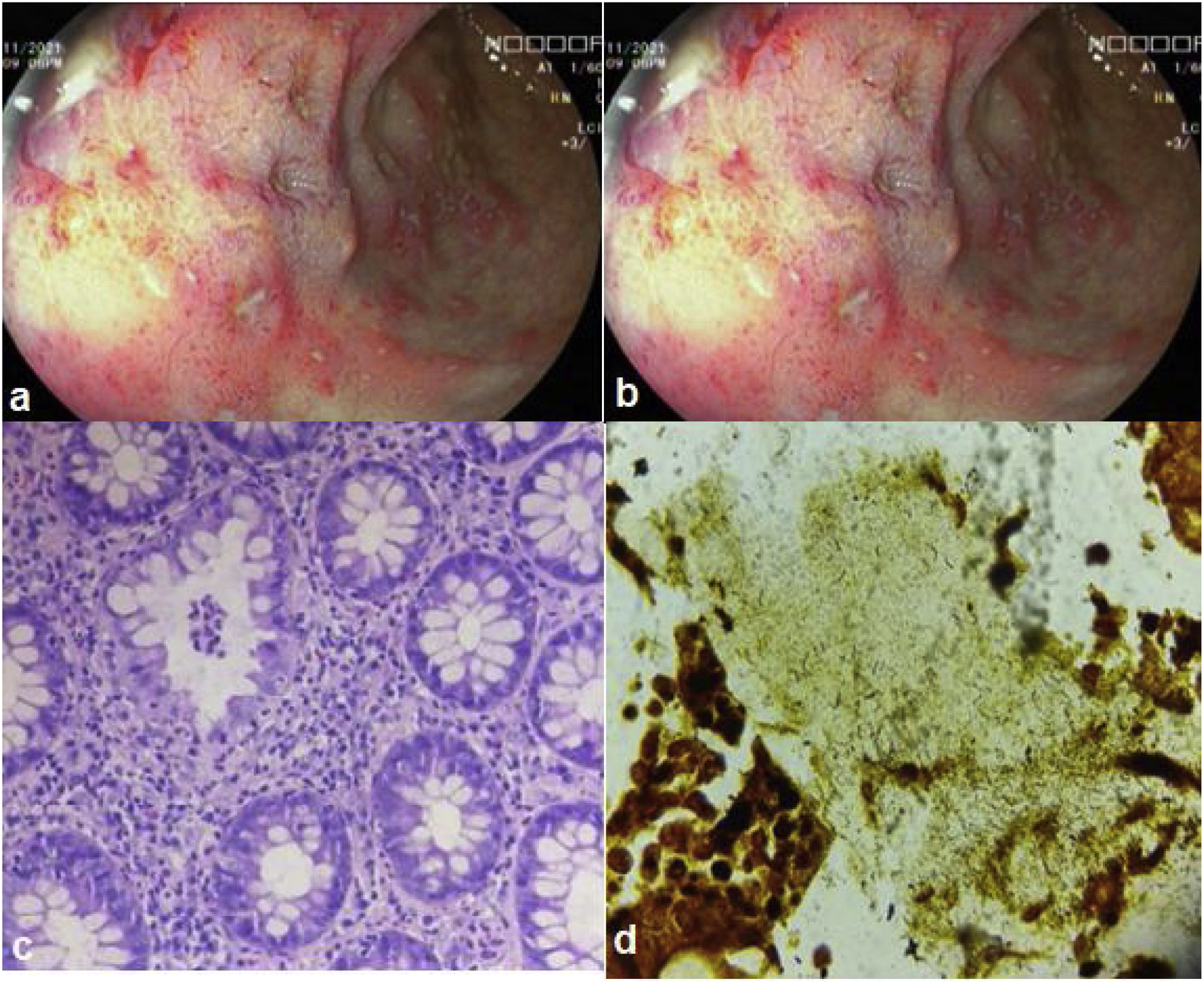
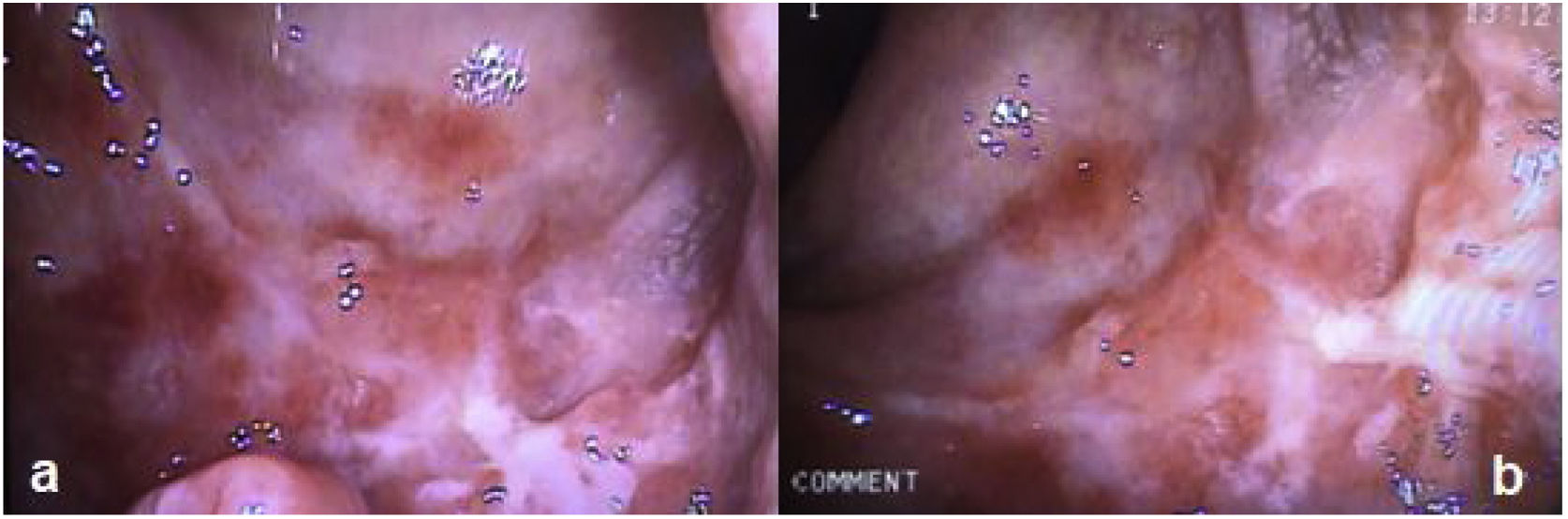
A 35-year-old man was diagnosed with HIV 3 years earlier and is undergoing treatment with a combination of tenofovir 300 mg + lamivudine 300 mg + efavirenz 400 mg, one tablet daily. The patient had a history of unprotected anal sex with men and sought medical attention due to straining, tenesmus, and rectal bleeding of two-week progression. Physical examination revealed multiple deep anal fissures. Laboratory work-up reported hemoglobin 15.2 g/dl, leukocytes 6,670 mm,3 HIV viral load 22.4 copies/mL, and CD4+ (T-helper) lymphocytes 765 cells/µl. Serum FTA-ABS was positive, RPR was reactive (RPR titer 1/4), and serum VDRL was reactive (VDRL titer 1/4). Chlamydia trachomatis IgG antibodies were reported at 348.5 RU/mL and IgM antibodies at 14.6 U/mL (positive >14). Proctoscopy revealed multiple erosions and rectal ulcers with raised edges and clean bases (Fig. 1a and b). Histology reported lymphoplasmacytic inflammatory infiltrate in the lamina propria, associated with cryptitis and cryptic microabscesses (Fig. 1c). Warthin-Starry staining identified multiple spirochetes (Fig. 1d). A single dose of intramuscular benzathine penicillin G (2.4 million units) was administered. At the control follow-up at three weeks, the patient was asymptomatic, and proctoscopy revealed the ulcer healing process (Fig. 2).
Syphilis is a systemic disease that can sometimes affect the gastrointestinal tract. The present case describes a young man with HIV that practiced unprotected sex with men. Physical examination revealed multiple anal fissures, leading to the diagnostic suspicion of an infectious disease.3–4 Clinical manifestations include anal pain, tenesmus, fecal urgency, purulent secretion, and rectal bleeding.5 The diagnosis of syphilis requires non-treponemal and treponemal antibody tests. Warthin-Starry staining can identify spirochetes. Nevertheless, we suggest the PCR test in rectal biopsies, which has 70–95% sensitivity and 92–98% specificity.6Chlamydia trachomatis infection, herpes simplex virus, and cytomegalovirus should be taken into account in the differential diagnosis in immunocompromised patients that practice unprotected sex, otherwise, neoplastic disease or inflammatory bowel disease should be considered.7,8 Local complications can include stricture, obstruction, and perforation of the rectum.9
In conclusion, rectal syphilis is rare and tends to present with ulcers and symptoms of proctitis. Opportune diagnosis is important, given that treatment is easy to carry out and offers a good prognosis, if administered in the early phase, thus preventing complications, such as neurosyphilis or severe damage to the heart.
Ethical considerationsThe authors declare that no experiments on humans were carried out for this research. Database protocols of the authors’ work center were followed, preserving patient anonymity. This study meets the current bioethical research norms, (thus informed consent was not requested), was approved by the Ethics Committee of theHospital Belén de Trujillo.
Financial disclosureNo financial support was received in relation to this study/article.
Conflict of interestThe authors declare that there is no conflict of interest.
Please cite this article as: Alcántara-Figueroa CE, Calderón-Cabrera DC, Estela-Vásquez EF, Coronado-Rivera EF, Calderón-De la Cruz CA. Sífilis rectal: reporte de un caso. Rev Gastroenterol Méx. 2023;88:186–188.