We aimed to investigate changes in initial platelet indices in patients arriving at the emergency department with acute cholecystitis.
Material and methodsA retrospective case-control study was conducted at a tertiary care teaching hospital. Demographics, comorbidities, laboratory data, length of hospital stay, and mortality data for the acute cholecystitis group were retrospectively obtained from the hospital digital database. Platelet count, mean platelet volume, plateletcrit, platelet distribution width, and platelet mass index were collected.
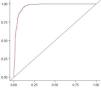
ResultsA total of 553 patients with acute cholecystitis were the study cases, and 541 hospital employees were the study controls. According to the results of the multivariate analysis of the platelet indices studied, only mean platelet volume and platelet distribution width showed significant differences between the two groups (adjusted odds ratio: 2, 95% confidence interval: 1.4−2.7, p < 0.001 and adjusted odds ratio: 5.88, 95% confidence interval: 2.44−14.4, p < 0.001, respectively). The multivariate regression model created had an area under the curve of 0.969 in the prediction of acute cholecystitis (accuracy: 0.917, sensitivity: 89%, and specificity: 94.5%).
ConclusionThe study results indicate that the initial mean platelet volume and platelet distribution width were independent predictors of acute cholecystitis.
Nuestro objetivo fue investigar los cambios en los índices plaquetarios iniciales en pacientes que llegaron a la sala de urgencias con colecistitis aguda.
Material y métodosSe realizó un estudio de casos y controles en un hospital universitario de tercer nivel. De manera retrospectiva, se obtuvo la siguiente información: demografía, comorbilidades, datos de laboratorio, duración de estancia hospitalaria y datos de mortalidad para el grupo de colecistitis aguda. Dicha información fue obtenida de la base de datos digital del hospital. Se obtuvo también el conteo plaquetario, el volumen medio plaquetario, el plaquetocrito, el ancho de distribución plaquetario y el índice de masa plaquetaria.
ResultadosLos casos de estudio fueron 553 pacientes con colecistitis aguda y los controles fueron 541 empleados del hospital. De acuerdo con los resultados del análisis multivariado de los índices plaquetarios estudiados, solo el volumen medio plaquetario y el ancho de distribución plaquetaria mostraron diferencias significativas entre los dos grupos (razón de momios ajustada: 2, intervalo de confianza de 95%: 1.4−2.7, p < 0.001, y razón de momios ajustada: 5.88, intervalo de confianza de 95%: 2.44−14.4, p < 0.001, respectivamente). El modelo de regresión multivariada creó un área bajo la curva de 0.969 en la predicción de colecistitis aguda (precisión: 0.917, sensibilidad: 89% y especificidad: 94.5%).
ConclusiónLos resultados del estudio indican que el volumen plaquetario inicial y el ancho de la distribución plaquetaria fueron predictores independientes de colecistitis aguda.
Gallbladder diseases constitute an important health problem, affecting approximately 20% of the general population in developed countries.1 Acute cholecystitis refers to a syndrome of right upper quadrant pain, fever, and leukocytosis associated with gallbladder inflammation. Acute cholecystitis is the most common complication of gallstone disease and typically develops in patients with a history of symptomatic gallstones. Less often, acute cholecystitis can develop without gallstones, accounting for approximately 5–10% of cases.2 Acute cholecystitis is associated with mortality, morbidity, and recurrent hospitalization, as well as difficult cholecystectomy.3 The diagnosis of acute cholecystitis is made by comprehensively evaluating the patient’s history, physical examination, laboratory findings, and imaging results. There is no single parameter that can be used to make or exclude a diagnosis of acute cholecystitis.4
Platelets are the basic element of coagulation reactions and take part in the aggregation, adhesion, secretion, and induction of procoagulant activity. They play a key role in the assembly of coagulation complexes and thrombin formation in primary hemostasis.5 In addition, thrombocytopenia and coagulation disorders occur in severe sepsis. Changes in platelet count and function in sepsis range from mild changes in platelet count to disseminated intravascular coagulopathy.6 Based on those data, we speculated that platelet count and other platelet parameters might be affected in patients with acute cholecystitis admitted to the emergency department. In this study, we aimed to investigate changes in initial platelet indices in patients with acute cholecystitis.
Material and methodsStudy designThe present analysis was designed as a retrospective case-control study. The healthcare center where the study was conducted was a tertiary care teaching hospital, with more than 500,000 annual emergency presentations. In our study, the data of patients with acute cholecystitis that were assigned the I81.0 ICD code between August 15, 2017, and August 15, 2021, were collected from the hospital digital database.
Study samplePatients with acute cholecystitis confirmed through clinical, laboratory, and radiologic (ultrasound or computed tomography) findings were included in the study as the case group, and hospital employees were recruited for the control group. In 2020, a total of 1,856 medical and non-medical personnel were working at our hospital. Every year, examinations for occupational diseases are routinely performed, and during that time, all hospital personnel are tested for hemogram and hepatitis markers. The blood test results of asymptomatic healthcare workers were used as the control group data. To minimize bias, a control individual of the same age was selected for each patient in the case group.
Data collectionDemographics, comorbidities, laboratory data, length of hospital stay, and mortality data for the acute cholecystitis group were obtained from the hospital digital database. The comorbidities of hypothyroidism, hyperthyroidism, hypertension, malignancy, diabetes mellitus, hyperlipidemia, chronic obstructive pulmonary disease, asthma, Alzheimer’s disease, coronary artery disease, heart failure, and chronic kidney disease were recorded. Of the laboratory parameters, white blood cell count, neutrophil count, lymphocyte count, eosinophil count, hemoglobin, hematocrit, red cell distribution width, platelet count, mean platelet volume, plateletcrit, platelet distribution width, platelet mass index, C-reactive protein, blood urea nitrogen, creatinine, aspartate transaminase, and alanine transaminase values were recorded. The platelet mass index was calculated by multiplying the mean platelet volume by the platelet count.
Statistical analysisThe Jamovi program (Version 1.6.21.0; The Jamovi Project, 2020; R Core Team, 2019) was used for the statistical analyses. The Shapiro–Wilk test was conducted to assess normality. Categorical data were presented as percentages and continuous data as interquartile range and median values. In the univariate analysis of data, the chi-square and Mann-Whitney U tests were applied, where necessary, for comparing the groups. The multivariate analysis was performed with parameters that had p values greater than 0.05 in the univariate analysis. The results of the multivariate analysis were presented using the adjusted odds ratio (AOR), 95% confidence interval (CI), and p values. The clinically significant predictors of acute cholecystitis were determined using a multivariate logistic regression model. The receiver operating characteristic (ROC) analysis was performed to reveal the accuracy of the model, and the results were presented as the area under the curve (AUC), sensitivity, specificity, and accuracy values. An AUC value of more than 0.7 was used for statistical significance.7 The Spearman’s correlation test was used to evaluate the correlation between platelet indices and C-reactive protein. A p value of less than 0.5 was used for statistical significance.
Ethical considerationsApproval for the current study was obtained from the local ethics committee. Due to the retrospective design of the study and the use of nonpersonal data, informed consent was not requested from the case and control groups, a fact known by the ethics committee.
ResultsAfter applying the exclusion criteria, 553 patients with acute cholecystitis were included as the case group and 541 hospital employees with complete hemogram parameters as the control group. There were 271 women in the case group, and the median patient age was 58 (25th and 75th quartiles: 44−71) years. The control group was made up of 378 women, and the median patient age was 42 (25th and 75th quartiles: 38–46) years. There was a significant difference between the cases and controls in terms of age (Mann–Whitney U test, p < 0.001) and sex (chi-square test, p < 0.001). Descriptive data and some biochemical parameters of the case group are shown in Table 1. According to the results of the univariate analysis, there was a statistically significant difference between the groups, with respect to the mean platelet volume, plateletcrit, platelet distribution width, and platelet mass index (Mann-Whitney U test; p < 0.001, p = 0.002, p < 0.001, and p = 0.001, respectively). According to the results of the multivariate analysis, of the platelet indices evaluated, only the mean platelet volume and platelet distribution width showed significant differences between the two groups (AOR: 2, 95% CI: 1.4−2.7, p < 0.001 and AOR: 5.88, 95% CI: 2.44−14.4, p < 0.001, respectively). Table 2 describes the results of the univariate and multivariate analyses of the remaining parameters. The multivariate regression model created had an AUC value of 0.969 in the prediction of acute cholecystitis (accuracy: 0.917, sensitivity: 89%, specificity: 94.5%) (Fig. 1). No statistically significant correlation was observed between platelet indices and C-reactive protein. P values for platelet count, mean platelet volume, plateletcrit, platelet distribution width, and platelet mass index were 0.125, 0.719, 0.276, 0.720, and 0.255, respectively (Spearman’s correlation test).
Descriptive data and biochemical parameters of the patients with acute cholecystitis.
| Parameter | n/%, median/25th–75th quartiles |
|---|---|
| Demographics | |
| Age | 58 (44−71) |
| Male | 282 (51%) |
| Female | 271 (49%) |
| Comorbidities | |
| Diabetes mellitus | 126 (22.8%) |
| Hypertension | 236 (42.7%) |
| Malignancy (active) | 23 (4.2%) |
| Hypothyroidism | 10 (1.8%) |
| Hyperthyroidism | 2 (0.4%) |
| Alzheimer’s disease | 10 (1.8%) |
| Chronic obstructive pulmonary disease | 37 (6.7%) |
| Coronary artery disease | 109 (19.7%) |
| Asthma | 44 (8%) |
| Heart failure | 39 (7.1%) |
| Chronic kidney disease | 16 (2.9%) |
| Laboratory parameters | |
| Albumin | 40 (36−43) |
| Aspartate transaminase | 30 (20−63) |
| Alanine transaminase | 27 (16−69) |
| C-reactive protein | 60 (10.2−155.2) |
| Blood urea nitrogen | 30.4 (23.5−40.2) |
| Creatinine | 0.84 (0.72−1.02) |
| Total bilirubin | 1.03 (0.6−1.75) |
| Direct bilirubin | 0.36 (0.2−0.74) |
| Indirect bilirubin | 0.6 (0.37−0.98) |
| Hospital stay (days) | 4 (3−6) |
| Mortality (30-day) | 12 (2.2%) |
Hematologic parameters of the enrolled population and comparison of the acute cholecystitis group and control group.
| Laboratory parameters | Case group | Control group | Univariate analysis | Multivariate analysis | |
|---|---|---|---|---|---|
| p values | Adjusted odds ratio (95% confidence interval) | p values | |||
| White blood cell count | 12.9 (10−16.9) | 6.87 (5.83−8.07 | <0.001 | 0.73 (0.55−0.97) | 0.032 |
| Neutrophil count | 10.3 (7.32−14.2) | 3.97 (3.25−4.89) | <0.001 | 0.49 (0.36−0.66) | <0.001 |
| Lymphocyte count | 1.56 (1.07−2.18) | 2.14 (1.82−2.64) | <0.001 | 1.2 (0.97−1.7) | 0.078 |
| Eosinophil count | 0.06 (0.01−0.14) | 0.15 (0.09−0.24) | <0.001 | 15 (2−109.7) | 0.007 |
| Basophil count | 0.03 (0.02−0.05) | 0.03 (0.02−0.049 | 0.002 | 15.3 (0.06−38.6) | 0.112 |
| Red blood cell count | 4.62 (4.27−5.02) | 4.6 (4.32−4.96) | 0.749 | ||
| Hemoglobin | 13.3 (12.1−14.6) | 13.4 (12.4−14.6) | 0.113 | ||
| Hematocrit | 40 (36.8−43.8) | 40.6 (38.1−44) | 0.003 | 1.1 (1.07−1.2) | <0.001 |
| Mean corpuscular volume | 87.2 (83.9−90.4) | 89.1 (85.7−91.9) | <0.001 | 1.07 (0.97−1.19) | 0.155 |
| Mean corpuscular hemoglobin | 29 (27.6−30.1) | 29.4 (28.1−30.4) | 0.009 | 0.8 (0.6−1.069 | 0.129 |
| Red cell distribution width | 14 (13.2−15.4) | 13.2 (12.8−13.9) | <0.001 | 0.7 (0.5−0.9) | 0.011 |
| Platelet count | 256 (213−318) | 258 (220−293) | 0.535 | ||
| Mean platelet volume | 9.3 (8.2−10.2) | 9.7 (9.1−10.4) | <0.001 | 2 (1.4−2.7) | <0.001 |
| Plateletcrit | 0.24 (0.18−0.3) | 0.25 (0.22−0.28) | 0.002 | 0.99 (0.9−1) | 0.831 |
| Platelet distribution width | 16.3 (16−17) | 16.1 (15.8−16-3) | <0.001 | 5.88 (2.44−14.4) | <0.001 |
| Platelet mass index | 2363 (1832−2985) | 2485 (2171−2842) | 0.001 | 0.99 (0.9−1) | 0.916 |
In the current study, we investigated changes in platelet indices in patients with acute cholecystitis. For this purpose, we used data from 553 patients with acute cholecystitis and 541 healthy hospital employees. Our results showed that mean platelet volume and platelet distribution width were independent predictors of acute cholecystitis. Another important result was that our multivariate regression model predicted acute cholecystitis with high accuracy (0.917).
Platelets are involved in immunity and have proinflammatory and prothrombotic properties. They perform their functions in hemostasis by interacting with endothelial cells. In addition, they interact with structural cells, such as lymphocytes, dendritic cells, and fibroblasts, and play a role in the regulation of the inflammatory response. Inflammatory cytokines affect the bone marrow, causing changes in platelet synthesis and maturation. Both as a cause and a result, inflammatory and infectious processes lead to changes in platelet number and structure.8,9
Mean platelet volume is an objective parameter in evaluating platelet size. Since the 1980s, impedance methods have been used in the automatic calculation of the complete blood count. Mean platelet volume is a well-known parameter that has been studied in many clinical scenarios in the literature, including sepsis, infection, and inflammation. First, Seker et al.10 investigated its role in acute and chronic cholecystitis and revealed the relation between low mean platelet volume values and cholecystitis. Later, studies conducted by Mahathi et al.11 and Sayit et al.12 presented similar results. The findings of our study were also in agreement with those found in the literature. Two explanations have been proposed as the cause of the decreased mean platelet volume in acute cholecystitis. The first is that IL-6, one of the inflammatory cytokines, causes a low mean platelet volume by acting on platelet production in bone marrow; the second is the theory of platelets being sequestered from the intestinal wall.10,11
Platelet distribution width is another platelet parameter determined during the automated analysis of hemogram profiles and is related to platelet morphology and proliferation kinetics. In the literature, platelet distribution width has been shown to increase in many cases in which the mean platelet volume decreases.13 A logical explanation for the increased platelet distribution width is changes in platelet morphology caused by inflammation.
The platelet mass index refers to the total platelet mass per unit volume. In the literature, it has been associated with platelet functions. Silahli14 showed that the platelet mass index was associated with an increased ventilation requirement in pediatric surgery cases. Chegondi et al.15 reported that the platelet mass index was associated with increased mortality in pediatric septic shock. In contrast, Algin and Özdemir16 found that said index was not associated with short-term mortality in adult COVID-19 cases. In our study, the platelet mass index was not affected in patients with acute cholecystitis. To the best of our knowledge, the present study is the first to investigate the relationship between acute cholecystitis and the platelet mass index.
There are several important limitations to our study. First, the retrospective design was a major obstacle. Second, balancing the groups was an important challenge, as in other case-control studies. Although the number of cases and controls was similar, demographic differences may have affected our results. Third, the relatively high number of cases with hypertension and coronary artery disease, many of whom could be taking acetylsalicylic acid, may be a confounding factor for our study, since acetylsalicylic acid has been reported to influence platelet indices.17
In conclusion, our study results indicated that the initial mean platelet volume and platelet distribution width were independent predictors of acute cholecystitis. Because they can be measured using inexpensive and easily accessible tests, decreased mean platelet volume and increased platelet distribution width values can assist clinicians in the evaluation of suspected acute cholecystitis cases.
Financial disclosureNo financial support was received in relation to the present study.
Conflict of interestThe authors declare that there is no conflict of interest.