Cirrhosis of the liver is a major cause of death worldwide, with a recent increase in cases secondary to metabolic dysfunction-associated steatotic liver disease and alcohol use. Liver transplantation is currently the only definitive treatment but requires immunosuppression for preventing graft rejection.
Calcineurin inhibitors are the cornerstone of immunosuppression in transplanted patients. However, their use conditions metabolic and renal complications, such as metabolic syndrome, post-transplant diabetes, and chronic kidney disease. Minimizing or discontinuing immunosuppression has been shown to reduce those adverse effects in selected patients, especially those with potential immunotolerance. Predictors of immunotolerance and cardiovascular complications in transplanted patients have been identified in recent studies. Thus, there is a need for developing individualized strategies for balancing metabolic risk and graft rejection prevention.
La cirrosis hepática representa una causa importante de mortalidad a nivel mundial, con un aumento reciente en los casos secundarios a la enfermedad hepática esteatósica asociada a disfunción metabólica y el consumo de alcohol. Actualmente, el trasplante hepático es el único tratamiento definitivo, pero amerita el uso de inmunosupresión para prevenir el rechazo.
Los inhibidores de calcineurina son la piedra angular de la inmunosupresión en pacientes trasplantados. No obstante, su uso condiciona complicaciones metabólicas y renales, como el síndrome metabólico, la diabetes postrasplante y la enfermedad renal crónica. La minimización o suspensión de la IS ha mostrado reducir estos efectos adversos en pacientes seleccionados, especialmente en aquellos con potencial inmunotolerancia. En estudios recientes, se han identificado predictores de inmunotolerancia y complicaciones cardiovasculares en pacientes trasplantados. Por tanto, existe la necesidad de desarrollar estrategias individualizadas para equilibrar el riesgo metabólico con la prevención del rechazo.
Liver cirrhosis (LC) is a worldwide public health problem, with an annual mortality rate of more than two million persons. In recent years, the etiology of this disease has evolved due to the growing pandemic of overweight and obesity. In Mexico, the current primary causes of cirrhosis are metabolic dysfunction-associated steatotic liver disease (MASLD), which is predominant in advanced age persons, and excessive alcohol use in young patients. On the other hand, the prevalence of hepatitis C virus has decreased significantly, thanks to high cure rates and universal access to direct-acting antivirals (DAAs).1–3
Liver transplantation (LT) is the curative treatment for decompensated LC or in selected cases of hepatocellular carcinoma, but its access is limited due to a scarcity of donors.2,4 Advances in surgical techniques and current immunosuppression (IS) strategies have improved overall survival in transplanted patients, reaching rates of 93%, 80.2%, and 64.3% at 1, 5, and 10 years, respectively.3 Nevertheless, those results depend on factors, such as etiology, age of the recipient, and the presence of comorbidities.
Within IS strategies, calcineurin inhibitors (CIs) are the cornerstone for preventing short and long-term graft rejection. Tacrolimus is the most widely used CI, and its administration is associated with greater patient and graft survival, in addition to having a positive impact on quality of life.5 However, the prolonged use of CIs leads to important challenges, particularly in the development or worsening of metabolic syndrome, among other complications.
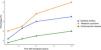
MASLD is closely associated with other metabolic disorders, such as diabetes mellitus, high blood pressure, obesity, and dyslipidemia, resulting in a greater risk of cardiovascular and renal complications, among others. This is aggravated by the use of IS agents, and the development of chronic kidney disease (CKD) is one of the biggest concerns. It is defined as a glomerular filtration rate < 60 ml/min for more than 3 months, which affects more than 14% of patients with LT, after 5 years. Those patients may require dialysis, or even a kidney transplant, after LT.6 In addition, metabolic syndrome occurs in more than 20% of patients after the first year of treatment, whereas new onset diabetes after transplantation (NODAT) affects more than 20% of patients after 2 years of follow-up. Those alterations contribute to an increase in the incidence of cardiovascular disease, surpassing 15% at 3 years, post-transplantation, and is one of the main causes of death in the transplanted population5 (Fig. 1).
In recent studies, noninvasive predictors of cardiovascular complications have been identified in the LT population. For example, a controlled attenuation parameter (CAP) > 270 dB/m determined during elastography was associated with a higher risk of myocardial infarction in patients with LT who also presented with diabetes.7 This underlines the need for individualized adjustments in the IS strategies for balancing metabolic and cardiovascular risks and graft rejection prevention. A study by Angelico et al.8 showed that the reduction in the CI dose to less than 25% of the maintenance dose, or its complete withdrawal, significantly decreased the prevalence of metabolic syndrome in transplanted patients: 8.3% in the reduced dose group versus 47.8% in the group with no changes. In addition, up to 50% of patients with previous metabolic alterations experienced improvement after reducing IS drug dose.8 In other words, the patients with a minimization or withdrawal of IS agents had a significant decrease in the associated metabolic complications.
Therefore, considering the implementation of a reduced IS regimen or its complete withdrawal has been proposed for patients at high risk of metabolic complications, particularly patients in whom a degree of immunotolerance is suspected. In a multicenter, controlled clinical trial on a highly selected transplanted population, IS drug withdrawal was achieved in 41% of the participants, suggesting that the combination of clinical parameters could be useful for identifying adequate candidates for those strategies.9 On the other hand, in another multicenter study, predictors associated with operational immunotolerance were identified. The most relevant were advanced age and prolonged time since transplantation, whereas serum biomarkers did not show such a significant role. However, even though there are numerous studies in this area, prospective analyses with larger samples are needed.10
In conclusion, as long as IS continues to be the cornerstone of treatment after LT, its management should be carefully adapted in patients at a higher risk of metabolic or cardiovascular complications. Considering IS minimization strategies and immunotolerance in selected patients is vital for optimizing quality of life and long-term results.
Financial disclosureNo financial support was received in relation to this article.
Ethical considerationsThere is no personal patient data or intervention information in the present article. It is considered low-risk and requires no review or approval by the local ethics committee. Likewise, the authors declare that it contains no personal information that could identify patients and needs no informed consent.
The authors declare that there is no conflict of interest.