Portal hypertension occurs when pressure in the portal vein is elevated, or when the hepatic venous pressure gradient (HVPG) exceeds 6 mmHg, becoming clinically significant at >10 mmHg.1 This condition can lead to variceal bleeding and ascites, among other complications. In non-cirrhotic cases, the cause of portal hypertension depends on the affected location (pre-hepatic, intrahepatic, or post-hepatic). Arterioportal fistulas (APFs) are abnormal connections between the splanchnic artery and portal vein, commonly due to trauma (28%),2 causing pre-sinusoidal portal hypertension. While often asymptomatic, some APFs cause severe portal hypertension, requiring rapid diagnosis and treatment to prevent complications. The case presented herein discusses portal hypertension due to a spontaneous splenic arteriovenous fistula (SAVF) and its management via invasive angiography.
A 62-year-old woman with no history of liver or pancreatic disease, alcohol abuse, trauma, or surgeries presented with three months of abdominal bloating and mild pain. Laboratory tests showed a normal platelet count (220,000/μl) and normal albumin (4.8 g/dl), bilirubin, and transaminase levels. Initial ultrasound revealed moderate ascites and splenomegaly, with no obvious liver abnormalities, as well as portal vein patency and increased flow velocity. Upper endoscopy identified large esophageal varices, which were ligated. The patient started treatment with carvedilol and furosemide for ascites and portal hypertension.
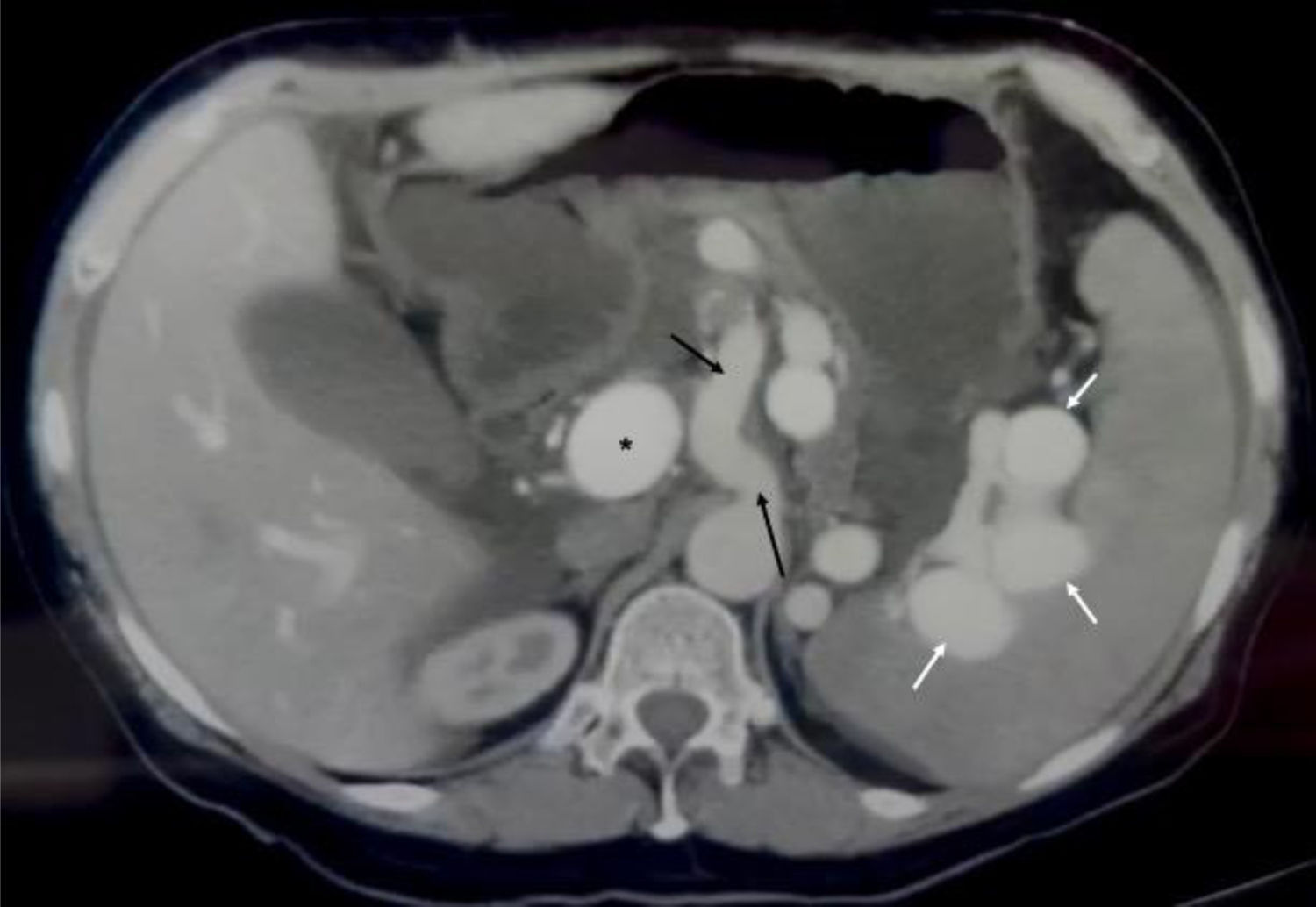
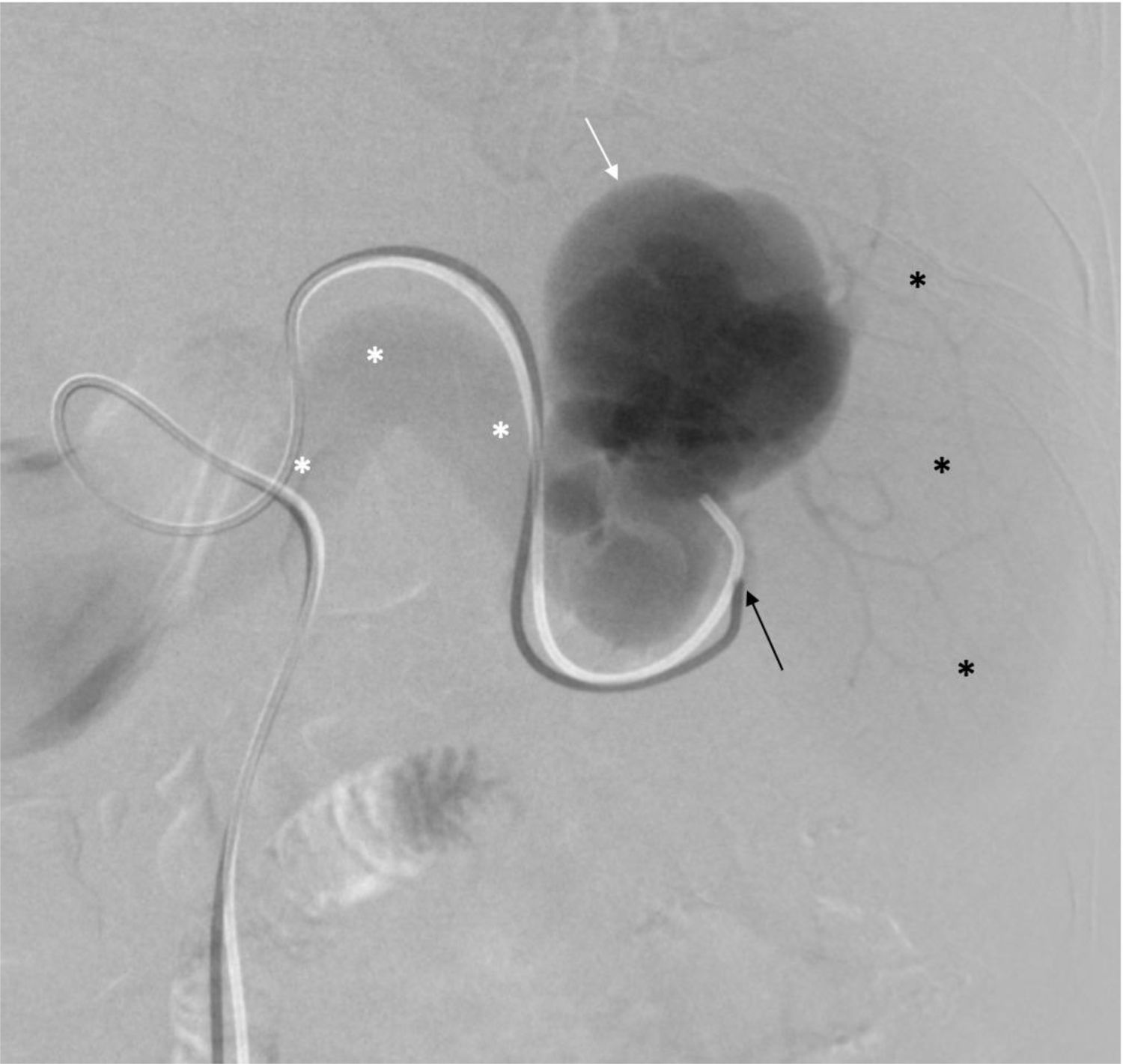
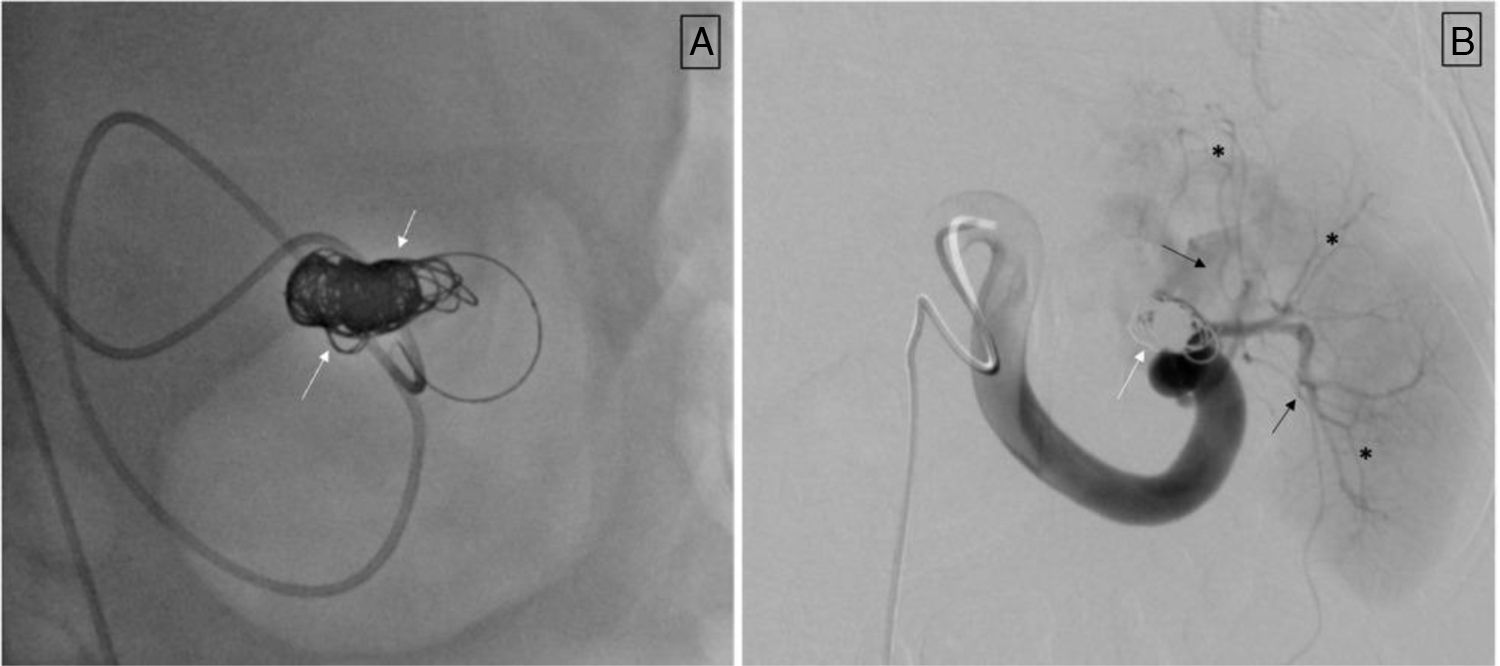
An abdominal and pelvic contrast-enhanced computed tomography scan showed arterialization of the portal vasculature with normal liver parenchyma, moderate ascites, and splenomegaly, ruling out other causes of portal hypertension and ascites (Fig. 1). Further imaging revealed communication between the splenic artery and vein. Angiography confirmed a SAVF, which was treated with coil embolization via the femoral artery approach with a 6 F sheath; the splenic artery was cannulated with a 5 F Cobra C2 catheter. Digital subtraction angiography (DSA) revealed an aneurysmal dilation of the splenic vein, without opacification of the splenic parenchyma (Fig. 2). The fistula was successfully embolized using coils placed via a microcatheter (Fig. 3). Post-procedure, the patient’s ascites and esophageal varices improved, and one year later, she does not need beta-blockers or diuretics and shows no signs of clinically significant portal hypertension.
The splenic artery is selectively cannulated (black arrow), and DSA is conducted from the distal portion of the artery, identifying the arteriovenous fistula with a venous aneurysm (white arrow) and revealing immediate opacification of the splenic vein (white asterisks) without any blush of the splenic parenchymal (black asterisks).
A) Superselective catheterization is performed using a microcatheter, followed by embolization with microcoils (indicated by white arrows) until the fistula is occluded. B) Control angiography from the proximal portion of the splenic artery, showing no opacification of the previously described venous aneurysm; the coils are visible (white arrows), along with the parenchymal branches (black arrows), and adequate splenic parenchymal blush (black asterisks).
APFs are rare but can be life-threatening. Most APFs (65%) originate from the hepatic artery, followed by the splenic (11%) and superior mesenteric arteries (10%).3 Causes include trauma (28%), iatrogenic events (16%), congenital anomalies (15%), tumors (15%), and ruptured aneurysms (14%).3 SAVFs, a subset of APFs, are classified by etiology, size, location, and physiologic effects: type 1 (small, intrahepatic, often asymptomatic), type 2 (larger, intrahepatic or extrahepatic, typically post-trauma, such as the SAVFs), and type 3 (congenital, causing severe hypertension in children).4
SAVFs can induce secondary fibrosis of the portal branches and capillarization of the hepatic sinusoids, adding an intrahepatic component to the disease, leading to hyperdynamic circulation in the portal branches and increased mechanical pressure in the hepatic sinusoids.5 This stimulates portosystemic collaterals, raising portal pressure.
Few idiopathic SAVFs without splenic artery aneurysms have been reported.6 An incidence of 8.7% was noted in splenic arterial aneurysms larger than 5 cm, although no correlation was found between aneurysm size and SAVF development.7
SAVF symptoms include ascites (35%), esophageal varices (52%), splenomegaly (55%), upper abdominal pain (30%), and gastrointestinal bleeding (45%).3,8 Only 16% of cases are asymptomatic.8 There is a predominance of females (80%), especially multiparous women, with a mean patient age of 44 years.6,9
Color Doppler ultrasound is preferred for initial imaging, showing turbulent, pulsatile flow with increased velocity in the fistula, enabling rapid diagnosis.9 However, selective splenic arteriography remains the gold standard for SAVF due to its accuracy in identifying vascular anomalies and collateral circulation.10
In cases with splenic artery or venous aneurysm, traditional open or laparoscopic splenectomy generally offers a good prognosis.6 However, secondary adhesions make exposing the lesion around the splenic hilum challenging, and high splenic pressure increases portal collaterals, making splenectomy risky due to intraoperative bleeding.6
Endovascular therapy, as in the present case, is a minimally invasive, cost-effective alternative, in which diagnosis and treatment occur simultaneously, without splenectomy, reducing complications.3 This approach is especially recommended in patients with acute portal hypertension and no liver disease.10 While vascular tortuosity and turbulent flow can complicate guidewire placement, transcatheter coil embolization reduces abnormal blood flow and splenoportal pressure, aiding in variceal rupture control and gastrointestinal bleeding management.8 Protecting splenic artery branches before embolization is essential, especially when the lesion is near the splenic hilum.
Most patients with SAVFs have a favorable prognosis. About 8% experience portal or splenic vein thrombosis post-embolization or post-splenectomy, despite anticoagulation.3 Other complications include abscesses and segmental splenic infarction.6
Endovascular embolization has a low surgical risk and preserves the spleen, making it the preferred option for patients with SAVF, especially those with simultaneous splenic arterial aneurysms. Treatment should be tailored to the patient’s vascular characteristics.
In conclusion, SAVFs represent a rare but important cause of portal hypertension, with potentially life-threatening complications. Although Doppler ultrasound is often used for making the initial diagnosis, selective splenic arteriography is essential for precise localization and therapeutic planning, offering favorable outcomes with minimal complications.
FundingNo sponsorship of any kind was received to carry out this article.
Ethical considerationsThe authors of the manuscript ensure that patient anonymity was maintained at all times during the preparation of this case report. This work complies with the current regulations in bioethical research and was carried out according to the knowledge and experience of the team doctor. At no time were any actions taken with the sole purpose of obtaining the publication of this report. Therefore, obtaining authorization from the ethics committee of our institution was not required.
The authors declare that they have no conflict of interest that could affect the objectivity of the case.