Graft-versus-host disease (GvHD) is a complication of hematopoietic cell transplantation, and the small bowel is one of the main targets in the gastrointestinal tract. Capsule endoscopy is a safe procedure and can be useful in the diagnosis of GvHD. The aim of the present study was to compare the diagnostic yield of capsule endoscopy with the histopathologic findings in GvHD.
Materials and methodsA retrospective diagnostic test study included all the patients with suspected GvHD that underwent gastroscopy and colonoscopy, with histopathologic evaluation of the biopsies taken, and capsule endoscopy, within the time frame of July 2015 and July 2019. Capsule endoscopy findings were compared with the histopathologic diagnosis, considered the gold standard.
ResultsTwenty-one patients with GvHD (7 [33%] women; 37 ± 11.9 years of age) were included, 20 (95%) of whom had acute GvHD. The median gastric transit time of the capsule was 55 minutes (20-113) and the median small bowel transit time was 261 minutes (238-434). The entire small bowel was visualized through capsule endoscopy in 17 cases (80.95%). The histopathologic findings and capsule endoscopy findings resulted in the diagnosis of GvHD in 17 and 16 cases, respectively. There was agreement between the histopathologic and capsule endoscopy findings in 18 cases (15 positive and 3 negative). Sensitivity, specificity, positive predictive value, negative predictive value, and diagnostic yield of capsule endoscopy were 88%, 75%, 94%, 60%, and 85%, respectively.
ConclusionsCapsule endoscopy is a safe tool for the diagnosis of GvHD, with high sensitivity and positive predictive value, as well as moderate agreement with histopathologic findings.
La enfermedad injerto contra huésped (EICH) es una complicación del trasplante de células hematopoyéticas. El intestino delgado (ID) es una área afectada del TD. La cápsula endoscópica (CE) es un procedimiento seguro y puede ser útil en el diagnóstico de EICH. El objetivo del trabajo es comparar el rendimiento diagnóstico de la CE con los hallazgos histopatológicos en EICH.
Material y MétodosEstudio de prueba diagnóstica retrospectivo que incluyó a todos los pacientes con sospecha EICH con estudio histopatológico de biopsias por gastroscopia y colonoscopia y CE, entre julio 2015 y julio 2019. Los hallazgos de CE fueron comparados con el diagnóstico histopatológico como prueba de oro.
ResultadosSe incluyeron a 21 pacientes con EICH [7 (33%) mujeres; 37 (± 11.9) años]. 20 (95%) tenían EICH agudo. La mediana del tiempo de tránsito gástrico fue de 55 minutos (20-113) y la del tiempo de tránsito del ID de 261 minutos (238-434). La visualización completa del ID por CE se observó en 17 casos (80.95%). Los hallazgos histopatológicos y de CE diagnosticaron EICH en 17 y 16 casos, respectivamente. El acuerdo entre hallazgos histopatológicos y de CE se identificó en 18 casos (15 positivos y 3 negativos). La sensibilidad, especificidad, valor predictivo positivo (VPP), valor predictivo negativo y rendimiento diagnóstico de la CE fue de 88%, 75%, 94%, 60% y 85%, respectivamente.
ConclusionesLa CE es una herramienta segura para el diagnóstico de EICH con alta sensibilidad y VPP, y concordancia moderada con los hallazgos histopatológicos.
Graft-versus-host disease (GvHD) is a frequent complication that presents in up to 20% of patients after an allogenic transplantation of hematopoietic cells, in which donor T cells attack the recipient’s healthy tissue.1 GvHD is divided into acute disease, if it presents within the first 100 post-transplantation days, or chronic disease, if it presents after the first 100 days.2 It can affect different organs, such as the skin, liver, and gastrointestinal tract, causing systemic deterioration, with high morbidity and mortality.3
GvHD that affects the gastrointestinal tract usually presents with secretory diarrhea, but can also produce vomiting, anorexia, and abdominal pain. The presence of bleeding is associated with poor outcome and results from ulceration of the mucosa.4 The mucosa is affected in patches, which is why it can go undetected by endoscopy, when normal mucosa is observed.5
Both upper endoscopy and colonoscopy are recommended tools in the study of gastrointestinal GvHD. Upper and lower gastrointestinal involvement are simultaneously affected in GvHD. The agreement rate between biopsies taken at the same time in the upper and lower digestive tract ranges from 59 to 83%.6
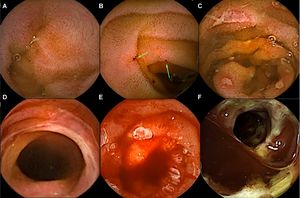
The small bowel (SB) is the area most affected by GvHD, given that it is the most extensive immune organ.7 GvHD can affect the SB in its entirety or by segments. The lesions generally identified in the SB are edema, erythema, erosions, ulcers, and bleeding.8 Capsule endoscopy (CE) is a noninvasive endoscopic tool that enables complete SB visualization. Different studies have demonstrated the utility of CE in the diagnosis of gastrointestinal GvHD.9 The aim of the present study was to evaluate the utility of CE as a diagnostic test in gastrointestinal GvHD.
Materials and methodsA retrospective diagnostic test study was conducted that included patients suspected of presenting with GvHD after bone marrow transplantation, who underwent gastroscopy and colonoscopy with biopsy and CE (Pillcam SB3, Given Imaging, Yokneam, Israel), with a period of less than one week between the two procedures, within the time frame of July 2015 and July 2019, at the Endoscopy Service of the Hospital de Especialidades del Centro Médico Nacional Siglo XXI, Instituto Mexicano del Seguro Social. Patients in whom cytomegalovirus or another opportunistic infection had not been ruled out prior to the CE were excluded from the study.
CEs were considered positive for GvHD when any of the following lesions were detected: erythema, erosions, ulcers, denudation of the mucosa, stricture, or bleeding. The CEs were compared with the histopathologic report of the biopsies of the stomach, duodenum, colon, and terminal ileum taken during the gastroscopy and colonoscopy procedures. All the CEs were read at a velocity of 10 images per second by an experienced endoscopist that had read more than 500 capsules.
Sample sizeSample size was calculated with the formula of a proportion with a 95% confidence interval and a power of 80%, based on the 12 bone marrow transplantations performed at the hospital annually and calculating that 20% of the patients would present with GvHD, resulting in a sample size of 11 patients per group. In relation to all patients that underwent the two diagnostic tests, the final sample size was 11 patients. Nevertheless, to increase the population, the decision was made to add all available patients to the study.
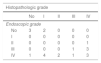
Statistical analysisThe distribution of the quantitative variables was evaluated using the Shapiro-Wilk test. The demographic characteristics of the patients were recorded, and the results were expressed in proportions for the qualitative variables. The quantitative variables with normal distribution were expressed with means as measures of central tendency and standard deviations as dispersion measures. For the variables considered distribution-free, the median and interquartile ranges (25-75) were utilized. A 2 × 2 table was performed to analyze the sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) of the CEs, comparing them with the gastroscopy and colonoscopy without biopsy and with the gold standard of histopathology. A sub-analysis was then performed in which agreement was analyzed utilizing the Cohen’s kappa coefficient between the Brand endoscopic classification for the CE findings and the Lerner histopathologic GvHD classification. The Brand classification was divided into grade 0 (normal), grade I (mild loss of vasculature and/or mild erythema), grade II (moderate diffuse erythema or nodularity), grade III (erosions or friability of the mucosa), and grade IV (desquamation, ulceration, and denudation of the mucosa)10 and the Lerner classification was divided into grade I (isolated apoptotic epithelial cells with no crypt loss), grade II (isolated crypt loss with no contiguous crypt loss), grade III (loss of 2 or more contiguous crypts), and grade IV (extensive crypt loss with denudation of the mucosa).11 The SPSS version 21.0 program was utilized.
Ethical considerationsAll the patients included in the study remained anonymous and provided signed statements of informed consent. The study met the current bioethics research regulations and was authorized by the local Research and Ethics Committee of the hospital (R-2020-3601-005).
ResultsTwenty-one patients were included in the study, their mean age was 37 years (± 11.9), 7 patients (33%) were females, and 20 patients (95.2%) presented with acute GvHD. Median gastric transit time was 55 min (20-113). Eight patients (38%) were given metoclopramide (10 mg IV) one hour after having swallowed the video capsule, given that it had not advanced to the duodenum. The capsule was advanced by endoscopy with the help of a polypectomy snare in 5 of those cases (23.8%) because it had not advanced, despite the metoclopramide, 2 h after ingestion. Median intestinal transit time was 261 min (238-434) and the entire SB was visualized in 17 patients (80.95%). There were no complications associated with the CE.
Of the 21 cases, GvHD diagnosis was made through histopathology in 17 cases and by CE in 16 cases. There was agreement between the two methods in 18 cases (15 positive and 3 negative). The Cohen’s kappa coefficient showed moderate agreement of 0.57 between the histopathologic result and the CE. Utilizing the Brand classification, the CE findings were defined as grade II in one case, grade III in 4 cases, and grade IV in 11 cases. No grade I lesions were identified (Fig. 1). CE had 88% sensitivity, 75% specificity, a PPV of 94%, and a NPV of 60%, when compared with the histopathologic study (Table 1). In the sub-analysis, the agreement between the endoscopic Brand classification and the Lerner histopathologic GvHD classification was mild, with a kappa of 0.12 and agreement in only 7 cases (Table 2).
Findings in the gastroscopy and colonoscopy with ileoscopy studies that were consistent with GvHD (mainly erosions, ulcers and/or active bleeding) were observed in 12 of the 21 cases (3 in gastroscopy and 11 in colonoscopy). Eleven of the cases diagnosed with GvHD were confirmed through histopathology. Aphthous ulcers in the terminal ileum were observed in one case but the diagnosis of GvHD was ruled out by histopathology. That patient was also diagnosed with GvHD by CE. The endoscopic studies (gastroscopy and colonoscopy), without biopsy, showed 64% sensitivity, 75% specificity, a PPV of 91%, and a NPV of 33% for GvHD diagnosis, compared with histopathology (Table 3). The diagnostic yield of CE was superior to the diagnostic yield of upper gastrointestinal endoscopy and colonoscopy without biopsy (85% vs. 66%; p = 0.026).
Diagnosis of graft-versus-host disease through histopathology and by gastroscopy and colonoscopy findings
| Histopathology (+) | Histopathology (-) | ||
|---|---|---|---|
| Gastroscopy and/or colonoscopy (+) | 11 | 1 | PPV 91% |
| Gastroscopy and/or colonoscopy (-) | 6 | 3 | NPV 33% |
| Sensitivity 64% | Specificity 75% |
NPV: negative predictive value; PPV: positive predictive value.
Different studies have shown a delay in gastric emptying in patients with GvHD. Varadarajan et al.12 observed a delay in the gastric transit time of the capsule in 45% of the patients in their case series that included 11 patients with GvHD. They considered an emptying delay when the video capsule was in the stomach for more than 2 h. In our case series, there was gastric emptying delay in 23.8% of the CEs, requiring endoscopy for capsule advancement. That percentage was lower probably due to the administration of metoclopramide in the patients in whom the capsule had not advanced for a period of one hour after its ingestion.
CE is a useful method for the diagnosis of GvHD, when compared with the gold standard of histopathology, as demonstrated by Pérez-Cuadrado et al.10 Theirs is the largest case series on CE in GvHD, identifying 86.21% sensitivity, 78.57% specificity, a PPV of 80.64%, and a NPV of 84.82%. Our study showed similar sensitivity and specificity (88 and 75%), but our NPV was lower (60%) and our PPV was higher (94%). As in our case series, Pérez-Cuadrado et al. also showed that the diagnostic yield of CE was statistically higher than that of gastroscopy and colonoscopy without biopsy.
The agreement between the result of the CE and the histopathologic result was moderate. That could be due to the great variety of findings identified in the intestinal mucosa in the patients with GvHD, that ranged from mild erythema to denudation of the mucosa. Previous studies have also reported no correlation between the histopathologic grade of GvHD and the grade of endoscopic findings.11 In our study, we also found no correlation between the histopathologic grades and the CE grades, given that the agreement between them was mild.
An advantage of CE over histopathology is that diagnosis by CE can be obtained in fewer than 24 h after placement, whereas histopathologic diagnosis usually takes longer (> 2 days), depending on the center where it is performed. Thus, CE enables the patient to start treatment earlier.
The limitations of our study were its retrospective design and the number of patients, even though the pathology is not very common. Given our study results, we conclude that CE is a useful tool for diagnosing GvHD, with high sensitivity and high PPV.
Financial disclosureNo financial support was received in relation to the present article.
Conflict of interestThe authors declare that there is no conflict of interest.
Please cite this article as: Blanco-Velasco G, Palos-Cuellar R, Domínguez-García MR, Solórzano-Pineda OM, Zamarripa-Mottú RA, Martínez-Camacho C, et al. Utilidad de la cápsula endoscópica en el diagnóstico de la enfermedad injerto contra huésped gastrointestinal. Revista de Gastroenterología de México. 2021;86:215–219.