The watch-and-wait (WW) strategy is an alternative to anterior resection in patients with rectal cancer (RC) that have had a complete clinical response to neoadjuvant treatment. Few reports describe the quality of life and functional anorectal disorders (FADs) in that population.
AimTo analyze and compare the FADs and quality of life in patients with locally advanced adenocarcinoma of the rectum treated with neoadjuvant therapy, divided into two different strategy groups: group 1 (G1), WW; and group 2 (G2), anterior resection.
Materials and methodsThirty patients (G1: n = 20 and G2: n = 10) that had finished neoadjuvant therapy at least 12 months prior were included. Mean patient age was 59.5 years (range: 41-79) and 15 of the patients were men. The FADs were evaluated through: a) clinical history, b) 21-day bowel diary, c) Jorge and Wexner fecal incontinence scale, d) anorectal manometry (ARM), and fecal incontinence quality of life scale (FIQL).
ResultsBowel diary: fecal incontinence (40%) and urge to defecate (45%) in G1 vs. fecal incontinence (60%) and urge to defecate (30%) in G2, with no significant differences (p = NS). Fecal incontinence scale: fecal incontinence in G1 was significantly less severe than that in G2 (median 6.5 points vs. 13 points [p = 0.0142]). ARM: no differences between the two groups. Quality of life: significantly different between the two groups (FIQL/G1: 3.7 vs. FIQL/G2: 2.8; p < 0.03).
ConclusionsThe WW follow-up strategy in patients with locally advanced rectal cancer was associated with better quality of life and reduced fecal incontinence.
La estrategia “watch and wait” (WW) es una alternativa a la resección anterior (RA) en pacientes con cáncer de recto (CR) con respuesta clínica completa a la neoadyuvancia. Existen pocos reportes que describan la calidad de vida (CV) y los trastornos funcionales anorrectales (TFA) en esta población.
ObjetivoAnalizar y comparar los TFA y la CV en pacientes con adenocarcinoma de recto localmente avanzados tratados con neoadyuvancia con diferentes estrategias: grupo 1 (G1): WW y grupo 2 (G2): RA.
Material y métodosSe incluyeron 30 pacientes (G1: n = 20 y G2: n = 10) que cumplieron al menos 12 meses de finalizado el tratamiento neoadyuvante, edad mediana de 59,5 años (rango: 41-79), 15 son hombres. Los TFA fueron evaluados con: a) historia clínica, b) diario de continencia anal de 21 días, c) escala de continencia anal de Jorge y Wexner, d) manometría anorrectal (MAR) y la CV con el cuestionario de incontinencia fecal (FIQL).
ResultadosDiario de continencia anal: G1: incontinencia fecal (40%) y urgencia defecatoria (45%) vs G2 incontinencia fecal (60%) y urgencia defecatoria (30%) sin diferencias significativas (p = NS). Escala de continencia anal: la incontinencia fecal de G1 fue significativamente menos severa que la de G2 [mediana 6,5 puntos vs 13 puntos; (p = 0,0142)]. MAR: sin diferencias entre los grupos. CV: es significativamente diferente entre ambos grupos (FIQL/G1: 3,7 vs FIQL/G2: 2,8; p < 0,03).
ConclusionesLa estrategia de seguimiento WW en pacientes con CR localmente avanzado estaría asociada con una mejor CV y menor incontinencia fecal.
Colorectal cancer (CRC) is a disease of great epidemiologic magnitude. Its incidence rates show there has been an ascending trend in recent years. It holds third place in both sexes in Argentina, and according to calculations by Abriata MG et al., the 2012 crude mortality rate for every 100,000 inhabitants in the country was 18.3 for men and 15.0 for women.1
Rectal cancer (RC) accounts for approximately one-third of the cases of CRC. Recent publications by the Surveillance, Epidemiology, and End Results (SEER) Program of the National Cancer Institute showed an increase in incidence of 2.6 in the last few years.2
Accurate staging is essential for planning preoperative treatment strategies. In patients with locally advanced RC, treatment is preoperative or neoadjuvant chemoradiotherapy (CRT), followed by surgery. Anterior resection (AR) with total mesorectal excision (TME) is the surgery of choice when the sphincteric apparatus can be spared, but it is associated with significant morbidity from complications, such as anastomotic leakage, and functional defecation and genitourinary disorders.3 Radiation of the pelvis is also an important factor and tends to lead to worse functional results and greater anastomotic complications.
Neoadjuvant CRT is a therapeutic strategy that increases the possibility of sphincter-sparing surgery in tumors of the low rectum. Forty to 60% of patients show some type of response to CRT, but only 7 to 15% have complete pathologic response.3,4 Given that scenario, the nonsurgical strategy called “watch-and-wait” (WW) has been developed, in which patients with complete clinical response (total tumor regression determined by proctologic exam, endoscopic evaluation, and images after CRT) are managed under a strict follow-up protocol with no radical surgery.3,5–7
Even though AR is the treatment of choice for RC, that procedure produces a series of pathophysiologic alterations known as “anterior resection syndrome” that occurs in up to 60% of operated patients.8–10 Said syndrome, combines different degrees and intensity of functional anorectal disorders (FADs): urge to defecate, tenesmus, incomplete defecation sensation, increase in the number of bowel movements, altered defecation rhythm, and varying degrees of fecal incontinence, causing psychologic and social consequences that influence patient quality of life (QoL). Different pathophysiologic factors are involved, such as loss or reduction of rectal reservoir function, or rectal compliance, and damage to the efferent and afferent nerve pathways of the hypogastric plexus, which cause reduced anorectal sensation and incoordination of the locoregional reflexes, with loss of the inhibitory rectoanal reflex.10,11 Even though said symptoms normally improve several months after surgery, they persist in half of patients one year after the surgical procedure and at least 10% of patients continue to present with deteriorated defecation function. Hygienic-dietary measures, pharmacologic treatment, and biofeedback exercises provide varied results. Some symptoms tend to improve over time, but not all alterations resolve, and some even worsen.12 Sacral neuromodulation is also a treatment proposal,13 but ostomy should be considered if conservative methods fail.
Functional results after AR vary significantly and tend to be related to the level of the anastomosis. As a general principle, defecation function worsens the more distal the anastomosis. Upon analyzing functional results, sexual and urinary functions should also be taken into account. Even though tumor exeresis is the main goal of the surgery, sparing of the autonomous nerves of the pelvis is essential for reducing alterations of those functions. In one case series, up to 25% of the patients operated on due to RC were reported to present with genitourinary dysfunction in the form of retrograde ejaculation, erectile dysfunction, dyspareunia, and urinary incontinence, among other symptoms.14,15
Surgery is not the only intervention that affects the defecation and genitourinary function of patients treated for RC. Radiation therapy to the pelvis is also an important factor and tends to lead to worse functional results and greater anastomotic complications.16 The biologic effects of radiation depend on two mechanisms: an immediate one caused by damage to DNA, and a later one, related to the appearance of an inflammatory response in the irradiated tissue. DNA damage can be direct, causing immediate cell death, or indirect, causing cell death as a consequence of the formation of free radicals. The late effects are produced as a result of progressive changes in the vascular and connective tissues, accompanied by an increase in the inflammation and fibrogenic mediators. The final result is chronically inflamed and ulcerated mucosa. The intestinal mucosa is characterized by its rapid response to radiation due to elevated cell reuptake. Symptoms can appear during radiotherapy, a few days afterwards, or months or years after finishing treatment. Radiation proctocolitis manifests as tenesmus, diarrhea, mucorrhea, and sometimes as proctorrhagia.16–18
The aim of our work was to analyze and compare the FADs and QoL in two cohorts of patients diagnosed with RC and treated with neoadjuvant CRT that were divided into two different strategy groups: group 1 (G1), with WW follow-up; and group 2 (G2), with AR + TME surgical treatment.
Materials and methodsPopulationThe present study included patients diagnosed with adenocarcinoma of the rectum that underwent neoadjuvant CRT and were then prospectively selected for the WW strategy (G1) or surgery (G2), at a single institution, within the time frame of January 1, 2013, and April 30, 2019. The inclusion criteria were patients with nonmetastatic adenocarcinoma of the rectum up to 15 cm from the anal verge, with a minimal post-CRT interval of twelve months, with no evidence of disease under strict surveillance (G1) and patients operated on more than twelve months after protective ileostomy closure (G2). The exclusion criteria were patients treated with local resection, previous pelvic radiotherapy for other pathologies, FADs diagnosed prior to RC, complications of the AR, such as stricture, and/or a previous history of dehiscence of the anastomosis.
MethodologyNeoadjuvant CRT was based on long-course 3D radiotherapy, with a total dose of 50-50.4 Gy, together with continuous oral administration of 825 mg/m2/bid of capecitabin. The evaluation of treatment response was analyzed based on the results of the proctology examination, endoscopic studies, abdominal and pelvic high-resolution magnetic resonance imaging (HRMRI), and computed tomography scan of the chest, performed within a period not less than 6-8 weeks after having finished radiotherapy. Complete clinical response was defined as endoscopic evidence of a whitish zone or telangiectasias or loss of folds in the rectal mucosa where the tumor had been, associated with the absence of tumor lesion and lymph node disease, determined through HRMRI.
The patients identified as complete clinical response cases were selected for the WW surveillance strategy (G1), if they required abdominoperineal amputation. The surveillance criteria for nonsurgical management were based on a monthly proctology exam, pelvic HRMRI, tumor markers every three months, chest and abdominal tomography scan every six months, for the first two years, after which they were all performed every 6 months.
In the G2 patients, surgery was performed according to the TME technique with protective ileostomy, with an interval equal to or greater than eight weeks after finishing the neoadjuvant treatment in the patients with residual lesion, determined through proctology exam or HRMRI. Postoperative follow-up was carried out with tumor markers every three months and a computed tomography scan of the chest, abdomen, and pelvis every six months for the first two years and video colonoscopy 12 months after the surgical procedure.
After the patients that met the eligibility criteria were selected, the clinical history, FADs, and QoL through the fecal incontinence quality of life (FIQoL) questionnaire were analyzed in each group.
The following functional characteristics were registered in the clinical history: a) daily number of bowel movements, divided into 3 categories, according to the ROME IV consensus: constipation: <3 bowel movements per week; normal defecation rhythm: between 3 and 21 bowel movements per week; diarrhea: >21 bowel movements per week, b) number of episodes of fecal incontinence per day, c) urge to defecate (presence or absence), d) tenesmus (presence or absence), e) stool characteristics, f) sexual function (erectile dysfunction and retrograde ejaculation in men and dyspareunia in women), and g) micturition alterations (incontinence, urgency, tenesmus). Likewise, the patients were given a continence diary to complete that consisted of a 21-day register of the following parameters: number of bowel movements and their characteristics, perceived and nonperceived episodes of fecal incontinence, presence of the urge to defecate, flatus episodes, use of pads, presence of leakage, use of drugs that modify the defecation rhythm, and daily activity conditioning. Continence was evaluated using the modified Jorge and Wexner anal continence scale that determines anal incontinence severity, taking into account whether the patient presents with incontinence of solid stools, liquid stools, or gas, reduced rectal sensation, the use of pads, and the impact on quality of life, on a scale from 1 to 20. Incontinence severity is classified as mild: 1-5 points, moderate: 6-10 points, serious: 11-15 points, and severe: 16-20 points.19 Conventional anorectal manometry (ARM) was performed, which is a technique that enables anorectal motor activity to be evaluated through the simultaneous registering of anal canal and rectal stump pressures, under resting conditions, as well as during the simulation of physiologic situations (voluntary contraction, squeeze, and cough maneuvers).20 Magna-Ars® equipment was utilized and consists of a pneumohydraulic capillary infusion pump with continuous perfusion at a speed of 0.2 mL/min, a polyvinyl probe with four radially directed (standard anorectal 4-channel probe R4B-3-0-0-0), a pressure recording system, and a computer that records and analyzes the data obtained. The following parameters were evaluated: resting pressure, pressure during voluntary contraction, cough reflex, squeeze maneuver, inhibitory rectoanal reflex, rectal sensation, rectal compliance,21 and the balloon expulsion test. Likewise, the slow removal technique was employed to obtain the anal canal pressures (pull-through technique).
The FIQoL scale was utilized in the present study. It is a specific instrument validated in Spanish (in Spain) that measures QoL in patients with fecal incontinence and is composed of 29 items that evaluate four aspects: lifestyle (10 items), behavior (9 items), depression/self-perception (7 items), and embarrassment (3 items). Each item has a scale from one to four, and the higher score, the better the QoL. The questionnaire has a maximum value of four points and a minimum value of one point. The score for each subscale is the mean of all the items.22,23
Statistical analysisThe personal, clinical, and histologic information, as well as the results of the tests performed, were recorded on a calculation sheet in the Excel program and processed utilizing MedCalc Version 11.2.1.0, MedCalc software. The data were reported as median and range. The results of the quantitative variables were analyzed comparing the values through the Mann-Whitney U test for independent groups. The qualitative variables were expressed in percentages. The differences were analyzed using the chi-square test or the Fisher’s test, as appropriate. Statistical significance was set at a p < 0.05.
Ethical considerationsNo experiments on animals or humans were conducted in the present research. The study was approved by the Teaching and Research Committee (CODEI, Spanish acronym) and the Ethics in Research Committee (CEI, Spanish acronym) of the Hospital de Gastroenterología “Dr. Carlos Bonorino Udaondo”. Informed consent was obtained from each patient (the documents are in the possession of the corresponding author) and carried out according to the principles of the Declaration of Helsinki, guaranteeing data confidentiality.
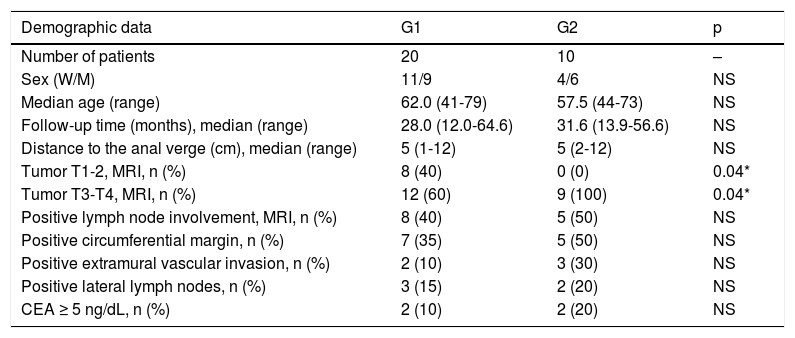
ResultsFifty-five patients were selected to participate in the study and a total of 30 patients were finally included. Mean patient age was 59.5 years (range: 41-79) and 15 of the patients were men (Table 1). There were no differences between the two groups in relation to the distance of the RC from the anal verge, lymph node involvement, the circumferential margin, extramural vascular invasion, carcinoembryonic antigen (CEA), and follow up time (p = NS) (Table 1). Likewise, in the initial HRMRI staging, the two groups were categorized into the tumor penetration subgroups of T1/T2 and T3/T4 (one patient in G2 did not have a HRMRI study). We found no significant differences in QoL or FADs between the two subgroups in the G1 patients (p = NS). Those findings could not be compared in the G2 patients because they all belonged to the T3/T4 subgroup (p < 0.04). There were significant differences in the QoL comparison in the T3/T4 subgroup: G1 median, 3.75 (1.45-4.0) vs. G2 median, 2.67 (1.92-4.0); p = 0.05 (Table 1).
Clinical and demographic characteristics of the patients in the two groups, upon entering the study.
| Demographic data | G1 | G2 | p |
|---|---|---|---|
| Number of patients | 20 | 10 | – |
| Sex (W/M) | 11/9 | 4/6 | NS |
| Median age (range) | 62.0 (41-79) | 57.5 (44-73) | NS |
| Follow-up time (months), median (range) | 28.0 (12.0-64.6) | 31.6 (13.9-56.6) | NS |
| Distance to the anal verge (cm), median (range) | 5 (1-12) | 5 (2-12) | NS |
| Tumor T1-2, MRI, n (%) | 8 (40) | 0 (0) | 0.04* |
| Tumor T3-T4, MRI, n (%) | 12 (60) | 9 (100) | 0.04* |
| Positive lymph node involvement, MRI, n (%) | 8 (40) | 5 (50) | NS |
| Positive circumferential margin, n (%) | 7 (35) | 5 (50) | NS |
| Positive extramural vascular invasion, n (%) | 2 (10) | 3 (30) | NS |
| Positive lateral lymph nodes, n (%) | 3 (15) | 2 (20) | NS |
| CEA ≥ 5 ng/dL, n (%) | 2 (10) | 2 (20) | NS |
W: women M: men.
MRI: initial staging through magnetic resonance imaging.
CEA: carcinoembryonic antigen.
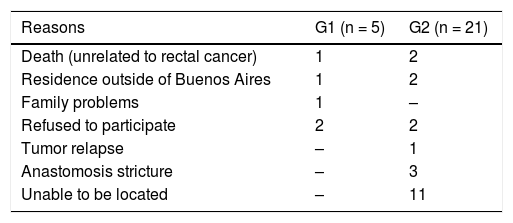
Table 2 describes the reasons why initially selected patients were not enrolled in the study. Notably, the majority of unenrolled patients corresponded to G2. The most frequent cause was not being able to locate the patients due to outdated telephone numbers and addresses in the clinical history.
Reasons why patients corresponding to either group were not enrolled in the study.
| Reasons | G1 (n = 5) | G2 (n = 21) |
|---|---|---|
| Death (unrelated to rectal cancer) | 1 | 2 |
| Residence outside of Buenos Aires | 1 | 2 |
| Family problems | 1 | – |
| Refused to participate | 2 | 2 |
| Tumor relapse | – | 1 |
| Anastomosis stricture | – | 3 |
| Unable to be located | – | 11 |
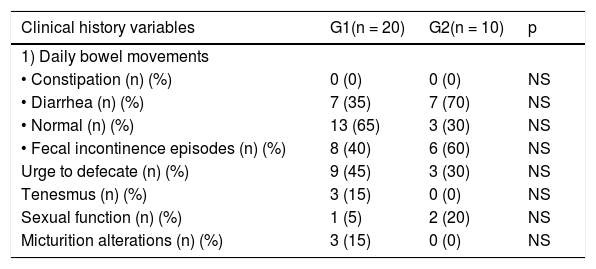
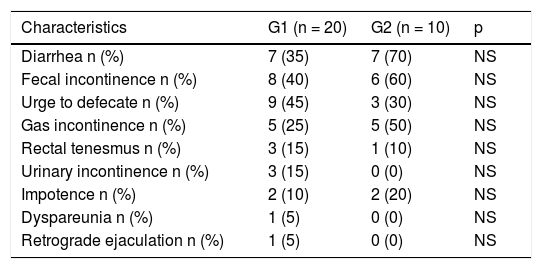
Table 3 shows the functional characteristics obtained from the clinical history. By direct questioning and evaluating the 21-day continence diary, the comparative analysis of the two groups produced no significant differences in any of the variables analyzed (p = NS) (Table 4).
Functional characteristics of the two groups.
| Clinical history variables | G1(n = 20) | G2(n = 10) | p |
|---|---|---|---|
| 1) Daily bowel movements | |||
| • Constipation (n) (%) | 0 (0) | 0 (0) | NS |
| • Diarrhea (n) (%) | 7 (35) | 7 (70) | NS |
| • Normal (n) (%) | 13 (65) | 3 (30) | NS |
| • Fecal incontinence episodes (n) (%) | 8 (40) | 6 (60) | NS |
| Urge to defecate (n) (%) | 9 (45) | 3 (30) | NS |
| Tenesmus (n) (%) | 3 (15) | 0 (0) | NS |
| Sexual function (n) (%) | 1 (5) | 2 (20) | NS |
| Micturition alterations (n) (%) | 3 (15) | 0 (0) | NS |
21-day anal continence diary description in the two groups.
| Characteristics | G1 (n = 20) | G2 (n = 10) | p |
|---|---|---|---|
| Diarrhea n (%) | 7 (35) | 7 (70) | NS |
| Fecal incontinence n (%) | 8 (40) | 6 (60) | NS |
| Urge to defecate n (%) | 9 (45) | 3 (30) | NS |
| Gas incontinence n (%) | 5 (25) | 5 (50) | NS |
| Rectal tenesmus n (%) | 3 (15) | 1 (10) | NS |
| Urinary incontinence n (%) | 3 (15) | 0 (0) | NS |
| Impotence n (%) | 2 (10) | 2 (20) | NS |
| Dyspareunia n (%) | 1 (5) | 0 (0) | NS |
| Retrograde ejaculation n (%) | 1 (5) | 0 (0) | NS |
The fecal incontinence analysis, evaluated with the Wexner scale, showed that the disorder was less severe in the G1 patients, and significantly different, compared with the G2 patients (median: 6.5 points [range: 3-14] vs. 13 points [range: 11-17], respectively [p = 0.0142]).
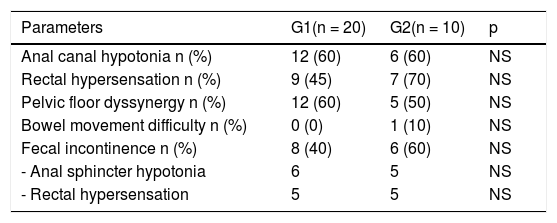
There were no significant differences in any of the ARM parameter variables between the two groups (Table 5).
Anorectal manometry parameter description in the two groups.
| Parameters | G1(n = 20) | G2(n = 10) | p |
|---|---|---|---|
| Anal canal hypotonia n (%) | 12 (60) | 6 (60) | NS |
| Rectal hypersensation n (%) | 9 (45) | 7 (70) | NS |
| Pelvic floor dyssynergy n (%) | 12 (60) | 5 (50) | NS |
| Bowel movement difficulty n (%) | 0 (0) | 1 (10) | NS |
| Fecal incontinence n (%) | 8 (40) | 6 (60) | NS |
| - Anal sphincter hypotonia | 6 | 5 | NS |
| - Rectal hypersensation | 5 | 5 | NS |
The QoL analyzed using the FIQoL questionnaire was significantly worse in the operated patients: G1 median 3.74 (1.45-4.0) vs. G2 median 2.83 (1.92-4.0); p = 0.0153. Likewise, upon comparing the patients with fecal incontinence in the two groups, there was a significantly different lower score in G2 (G1 [n = 8] median: 3.69 [1.4-4.0] vs. G2 [n = 6] median: 2.49 [1.9-3.1]; p = 0.0282). No significant differences were found between the two groups, regarding the patients with no fecal incontinence (p = NS) (Table 6).
Quality of life in the two groups.
| Score | G1(n = 20) | G2(n = 10) | p |
|---|---|---|---|
| Median total FIQoL (range) | 3.74 (1.45-4.0) | 2.83 (1.92-4.0) | 0.0153* |
| Number of patients with incontinence (n) (%) | 8 (40) | 6 (60) | |
| Median FIQoL (range) | 3.69 (1.4-4.0) | 2.49 (1.9-3.1) | 0.0282* |
| Number of patients without incontinence (n) (%) | 12 (60) | 4 (40) | |
| Median FIQoL (range) | 3.81 (2.8-4) | 3.68 (3.0-4.0) | NS |
FADs and QoL in patients with RC treated with surgery have been studied but there are few publications on patients with the WW follow-up strategy.8,24–26 Neoadjuvant therapy per se is not free from adverse effects, given that one-third of WW group patients have altered scores on fecal incontinence scales.27
The study by Habr-Gama A et al. compared patients with the WW strategy vs. patients that received CRT followed by local excision, utilizing ARM, the Wexner scale, and the FIQoL scale, three years after completing treatment.4 The group that underwent local resection presented with lower anal canal pressure, less rectal compliance, a higher score on the Wexner scale, and a lower score on the FIQoL questionnaire.25 Even though the surgical strategy in our population was different, the results were similar.
In 2015, Ozgen Z et al. studied QoL (through the EORTC QLQ C30 and CR38 questionnaires) and the functional results (ARM and the Wexner scale), at a mean of 30 months of follow-up, in 29 patients with locally advanced RC that had neoadjuvant treatment and AR. Twenty-five to 50% of the patients presented with some type of pelvic dysfunction. Those authors concluded that neoadjuvant therapy + AR was associated with greater urge to defecate and fecal incontinence, with a significant impact on QoL.26
To the best of our knowledge, there is only one article that simultaneously analyzes the two groups. Hupkens BJP et al. compared QoL through different questionnaires, two years after completing CRT.27 The patients in the WW group had better scores on all the questionnaires. The AR group had worse scores on the fecal incontinence scales, with statistically significant differences. Our study supports that perspective with similar results. There was a greater impact on QoL in the patients that underwent surgery (Table 6). The G2 patients with fecal incontinence had a statistically significant lower score, compared with the G1 patients with fecal incontinence (p = 0.0282). There were no differences between the groups, in the patients that did not have fecal incontinence.
Fecal incontinence was analyzed using the Wexner scale, and even though it was present in both groups, it was less severe, and significantly different, in the patients with the WW strategy, compared with the operated patients (p = 0.0142). The results suggest incontinence would be mild-to-moderate in the non-operated patients and serious-to-severe in the operated patients. Anorectal motor activity of the two groups was analyzed through ARM, but no significant difference was demonstrated in any of the variables studied (Table 5).
Our study maintains the view that no treatment of RC is free from FADs and leads to QoL alterations, but that surgical treatment has worse functional results with greater impact on QoL.
We believe that WW is the better strategy for preserving anatomic structures, with a lower probability of fecal incontinence.
ConclusionsThe results of the present study suggest that a large percentage of patients treated for RC, regardless of the strategy employed, present with alterations of anorectal function and quality of life.
The watch-and-wait strategy in patients with locally advanced adenocarcinoma of the rectum was associated with better QoL and reduced fecal incontinence, compared with the AR + TME strategy.
A larger number of patients are needed to be able to ratify or rectify the results of our study.
Conflict of interestThe authors declare that there is no conflict of interest.
Financial disclosureFinancial supportNo financial support was received in relation to the designing, conducting, and/or drafting of the present manuscript.
GrantsAgostina Pascual Russo received a Training, Public Health, and Research grant from the Buenos Aires City Government for “Estudio piloto comparativo de la calidad de vida y la función anorrectal en pacientes tratados por cáncer de recto mediante watch and wait versus tratamiento quirúrgico”. years: 2017-2019. Buenos Aires City Government, Department of Health, Autonomous City of Buenos Aires, Argentina.
SubsidyGiven for the purchase of supplies (4-channel anorectal manometry probe, poster printing). Buenos Aires City Government, Department of Health, Autonomous City of Buenos Aires, Argentina.
Please cite this article as: Pascual-Russo A, Milito D, Facio L, Furia M, Forestier V, Iseas S, et al. Mejor calidad de vida y menor incontinencia fecal en pacientes con cáncer de recto con la estrategia de seguimiento watch and wait. Rev Gastroenterol Méx. 2021;86:340–347.