It has been reported that approximately 25% of the patients with acute pancreatitis (AP) will present with the severe form of the disease, which is associated with local complications, such as infected pancreatic necrosis (IPN), whose mortality rate is 30%1.
Walled-off pancreatic necrosis (WOPN) is a mature collection of pancreatic and/or peripancreatic necrosis and has a well-defined inflammatory wall; said maturation usually occurs more than 4 weeks after the onset of necrotizing pancreatitis2.
Computed tomography (CT) cannot easily distinguish solid content from liquid content, thus pancreatic and peripancreatic necroses can be misdiagnosed as pancreatic pseudocyst, resulting in the possible need for magnetic resonance imaging, transabdominal ultrasonography, and endoscopic ultrasonography2. The indications for intervention in WOPN are infection or clinical deterioration following conservative management, the persistence of symptoms of gastric, intestinal, or biliary obstruction, or pain due to the mass effect3.
Late necrosectomy (after 4 weeks) has shown fewer complications and less mortality than early necrosectomy, because that amount of time is needed for the demarcation of the necrotic tissue to occur. However, open necrosectomy is associated with significant morbidity, especially with a high rate of pancreatic fistulas (40%), enteric fistulas (20%), and incisional hernias (25%), as well as with a mortality rate that ranges from 9 to 25%1,4.
In recent years, different minimally invasive techniques have been described for pancreatic drainage, such as percutaneous drainage, endoscopic transgastric drainage, laparoscopic drainage, and video-assisted retroperitoneal drainage (VARD). The failure rate of percutaneous drainage varies from 20 to 50%, requiring formal necrosectomy. Laparoscopic transgastric necrosectomy (LTN) enables efficacious debridement of the necrotic tissue in a single intervention and creates a controlled communication that enables the continuous drainage of the pancreatic necrosis, in addition to reducing the risk for enterocutaneous fistulas, pancreatic fistulas, and incisional hernias4.
Indocyanine green has a 2 to 3-minute half-life, with tissue penetration of up to 5mm. It is eliminated in the bile, without metabolizing, after 15-20minutes, there is no enterohepatic recirculation, and its toxicity is low (0.005% complications)5.
Fluorescent cholangiography with indocyanine green is radiation-free and enables real-time intraoperative visualization of the extrahepatic bile ducts in 72 to 96% of cases, although whether it reduces operating time for identifying the critical view of safety (CVS), compared with the conventional method, has not been demonstrated6,7. There are few studies on the use of indocyanine green in pancreatic resection, due to cancer of the pancreas, and we found no articles on its use in pancreatic necrosectomy.
During our intervention, we utilized cholangiography with the intravesicular injection of indocyanine green, which resulted in increased visualization and identification of the extrahepatic bile ducts, reducing the risk for bile duct injury, compared with the white light method8.
We present herein the case of a 57-year-old woman, with no past medical history, who presented with sharp abdominal pain in the epigastrium that radiated to the back, of 1-month progression, with periods of remission and exacerbation. Her laboratory tests showed serum amylase of 816u/l and serum lipase of 2884u/l; a liver and biliary tract ultrasound revealed a gallbladder containing stones, a 2.8mm wall, and a choledochus of 4mm, resulting in the diagnosis of acute biliary pancreatitis. Dynamic pancreatography was carried out 48h after hospital admission, due to the persistence of pain and an elevated systemic inflammatory response, which showed pancreatic necrosis in 30% of the gland.
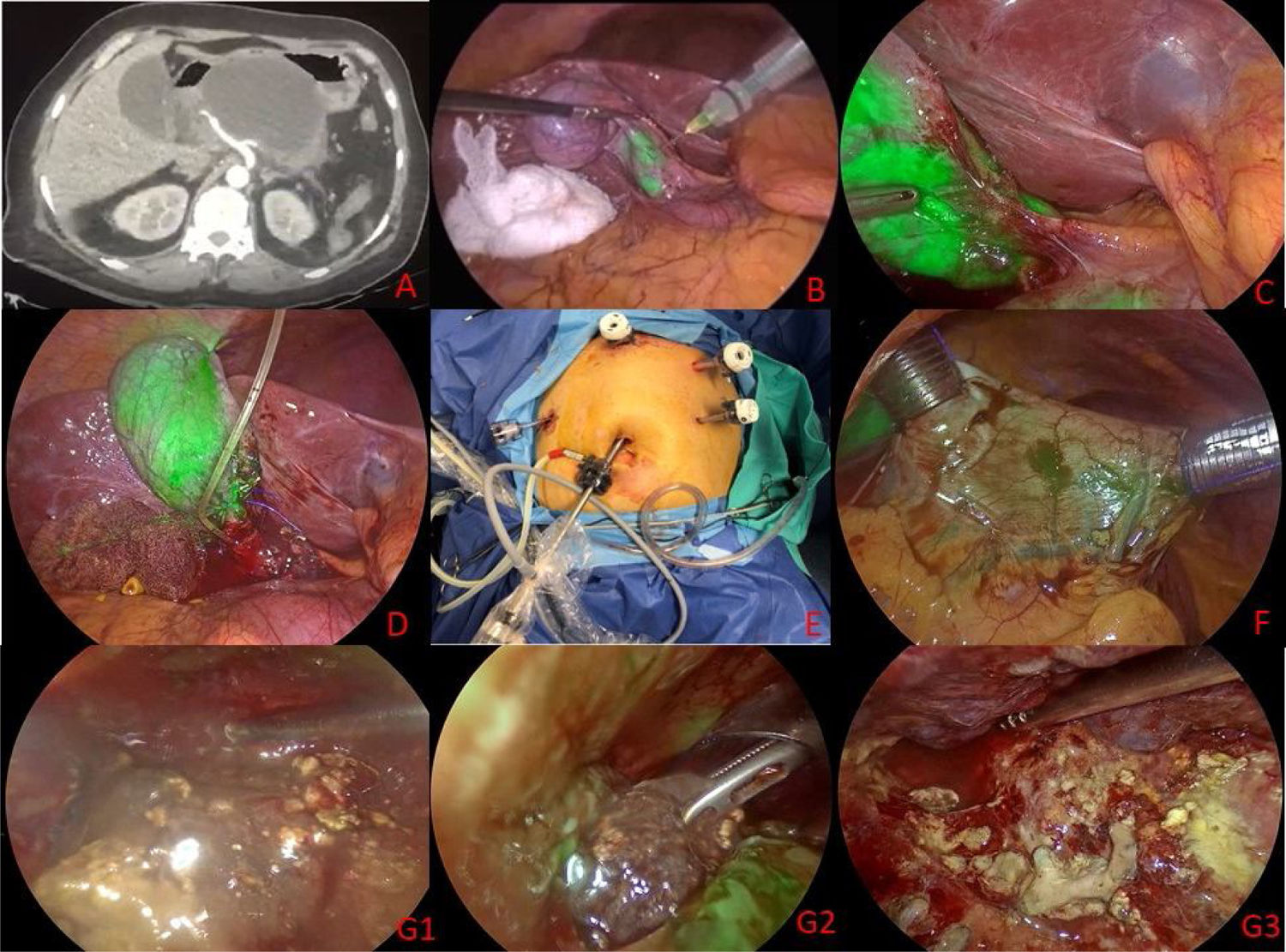
Due to favorable progression, the patient was released 13 days after admission. One week later, she presented with abdominal pain again, poor tolerance to oral diet, bloating, and early satiety. A new CT scan showed a cystic image with walled-off necrosis that involved the head and body of the pancreas, with diameters of 10.2×7.4×9.6cm and a volume of 378cm3 that conditioned compression of the gastric chamber (Fig. 1A).
A) Contrast-enhanced abdominal tomography scan. B) Intravesicular application of indocyanine green. C) Identification of the structures of the hepatocystic triangle. D) Intraoperative cholangiography. E) Positioning of the trocars. F) Transgastric trocars after intravenous injection of indocyanine green. G1-G3) Transgastric necrosectomy.
The patient was operated on 31 days after the onset of necrotizing pancreatitis. Laparoscopic cholecystectomy, intraoperative cholangiography with indocyanine green, and laparoendoscopic transgastric necrosectomy were performed.
The surgical technique was carried out with the patient in the French position, utilizing Storz RUBINA™ laparoscopic equipment. Five ports were used in the approach. A 12mm trocar for the supraumbilical port, a 12mm trocar for the subxiphoid port, and a 5mm trocar in the right flank port were used for the laparoscopic cholecystectomy. One milliliter of indocyanine green was diluted in 10ml of saline solution and applied intravesicularly (Fig. 1B), enabling fluorescence-guided cholangiography that identified the structures of the hepatocystic triangle (Fig. 1C). Cholangiography with water-soluble contrast medium at 50% was then performed, ruling out the presence of choledocholithiasis (Fig. 1D).
In the approach to WOPN, the previously placed 12mm trocar in the subxiphoid port was used, and two additional trocars were placed: a 12mm trocar in the left hypochondrium and a 5mm trocar in the left flank (Fig. 1E). The 12mm subxiphoid and left hypochondrium trocars were placed on the anterior surface of the gastric antrum, after intravenous injection of 3ml of indocyanine green (Fig. 1F), to prevent vascular injury during the access to the stomach. Gastroscopy was simultaneously performed to achieve maximum insufflation of the stomach and double intragastric vision. The posterior gastrostomy was made at the compression site, utilizing a harmonic scalpel, with an approximately 7cm incision, achieving drainage of the pancreatic collection, and necrosectomy was performed under direct vision, until the viable pancreatic tissue was demarcated. The viability of the residual pancreatic tissue was corroborated by another intravenous injection of 3ml of indocyanine green (Fig. 1G1-G3). The resected necrotic tissue was sent for pathologic study, which reported mature adipose tissue with areas of liquefactive necrosis (blurring of adjacent structures).
The posterior gastrostomy was left open and the intragastric trocars were removed, with closure of the anterior gastrostomies with polypropylene 0 extracorporeal Gea knots. A Jackson Pratt closed drain was placed in the subhepatic space. Surgery duration was 111minutes, with intraoperative blood loss of 250ml.
Oral diet was started the same day in the afternoon and the patient was released from the hospital with no complications, 48h after the surgery.
Ethical considerationsBefore performing the surgical procedure, a written statement of informed consent was requested from the patient and the corresponding relative responsible for the patient, and observed by two witnesses. Because it is a case report, and not a research protocol, authorization by the ethics committee of the Hospital General Dr. Manuel Gea González was not required. The authors declare that this article contains no personal information of any kind that could identify the patients.
Financial disclosureNo financial support was received in relation to this article.
Conflict of interestThe authors declare that there is no conflict of interest.
Please cite this article as: Brito-Carmona RD, Cuendis-Velázquez A, Chávez-Hernández AF, Galván-Cruz AD, Cárdenas-Lailson LE. Tratamiento laparoendoscópico de necrosis pancreática encapsulada, guiado con verde de indocianina. Revista de Gastroenterología de México. 2022;87:388–390.