Bile duct tumors are relatively rare. The general prognosis is poor, and they are detected in older adult patients. Treatment and management of those lesions has changed over the past 2 decades.
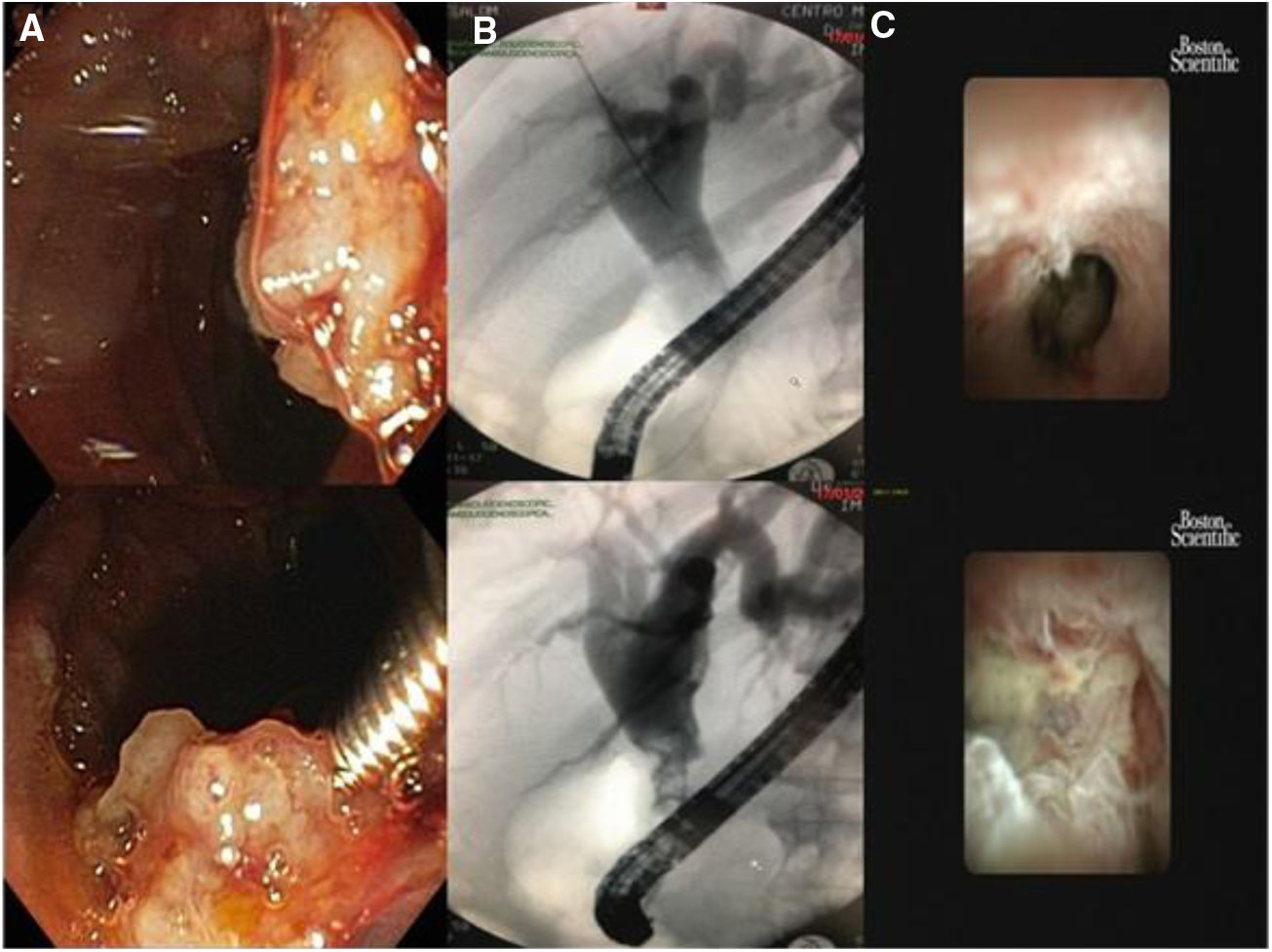
A 60-year-old man had a history of high blood pressure, dyslipidemia, and functional gastrointestinal disorders. One month earlier, he presented with pain in the right hypochondrium, bloating, general malaise, early satiety, and hyporexia. He was treated with prokinetics and antispasmodics, resulting in partial improvement. Two weeks before hospital admission, he presented with the added symptoms of choluria, mild jaundice, chills, and tachycardia. He arrived at the emergency room with a body temperature of 38.8 °C and mild dehydration. Cardiopulmonary examination was normal, and he had a distended abdomen, with non-radiating pain in the right flank. The initial laboratory work-up reported total leukocytes of 13.1, AST 288 U/L, ALT 449 U/L, ALP 509 U/L, GGT 1296 U/L, TB 2.65 mg/dL, DB 1.32 mg/dL, and LDH 236 U/L. Upper abdominal ultrasound revealed dilation of the intrahepatic bile ducts, a choledochus measuring 1.7 cm, hydrocholecyst, sludge, and microlithiasis. Moderate cholangitis was diagnosed, according to the 2018 Tokyo criteria. Endoscopic retrograde cholangiopancreatography (ERCP), with sphincterotomy and balloon sweeps, was performed. Parts of a vegetative tumor measuring approximately 1 cm were extracted (Fig. 1A). The cholangiography revealed irregular radiolucent images in the common hepatic duct that extended up to the papilla (Fig. 1B). The histopathologic report stated papillary neoplasm with unclassified atypia. Magnetic resonance cholangiography confirmed the bile duct dilation and showed hypointense material in the entire choledochus, without determining the extension. Cholangioscopy (Spyglass) was performed later, finding hyperemic lesions in the right and left hepatic ducts, extending into the proximal and distal choledochus. The lesions were biopsied (Fig. 1C).
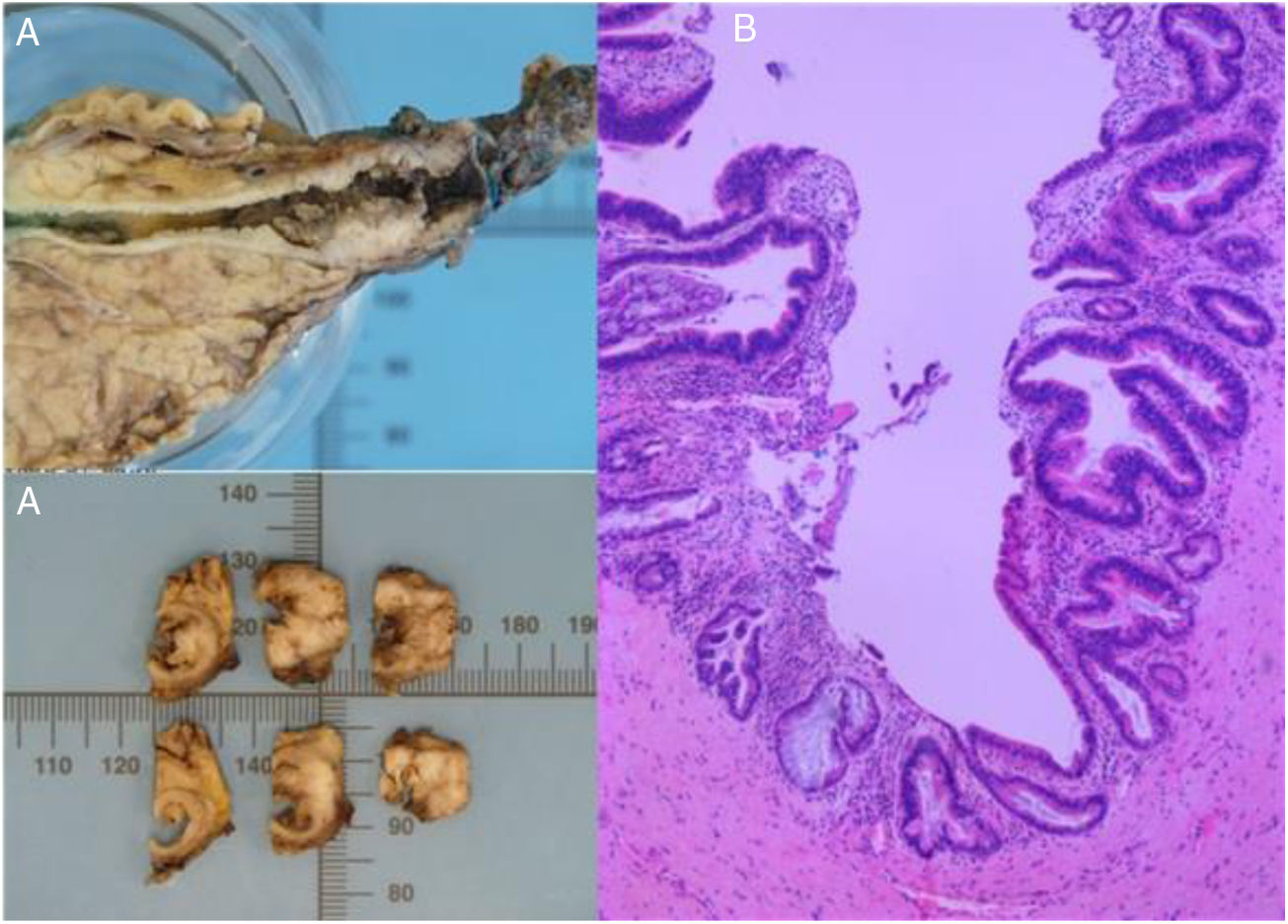
The histopathology study reported an intraductal papillary neoplasm of the bile duct, with a polypoid-villous, digitiform appearance and high-grade dysplasia, and a pancreatobiliary and foveolar epithelium, with no invasive component. Surgical treatment with the pylorus-sparing Whipple procedure (pancreatoduodenectomy) and intraoperative examination with the choledochoscope to evaluate the tumor margins were performed. Two main tumor sites were found. The first was near the bifurcation of the hepatic ducts and the second was near the ampulla of Vater, measuring approximately 3 cm in length (Fig. 2A). Pancreaticojejunal anastomosis was carried out, cannulating the pancreatic duct with an exteriorized 5 Fr catheter, and double-layered hepaticojejunal and duodenojejunal anastomoses were also carried out, leaving a 19 Fr Blake drain at the surgical site of the 3 anastomoses. The final histopathology report confirmed an intraductal papillary neoplasm, measuring 2.8 × 1.5 cm; foci of high-grade dysplasia in the extrapancreatic and intrapancreatic distal choledochus; foci of well-differentiated intestinal adenocarcinoma (G1), invading the wall of the choledochus; low-grade and high-grade dysplasia at the surgical margin of the bile ducts (T4); no lesion at the surgical margins of the pancreatic neck, main pancreatic duct, the uncinate process, or the duodenum; and twelve resected regional lymph nodes (pN0) with no metastasis and no vascular or perineural invasion. Through immunohistochemistry, the neoplastic cells were positive for CK7, CK20, CKX2, and MUC5AC (Fig. 2B). The patient spent time in the intensive care unit, after which he was transferred to the hospital ward, and then released for outpatient follow-up.
(A) Macroscopic image of the bile duct resected in the pancreatoduodenectomy, with two tumor sites (near the bifurcation of the hepatic ducts and near the ampulla of Vater). (B) Intraductal papillary neoplasm with foci of high-grade dysplasia in the extrapancreatic and intrapancreatic distal choledochus, microscopic foci of well-differentiated intestinal adenocarcinoma (G1) invading the wall of the choledochus, with low-grade and high-grade dysplasia at the surgical margin of the bile ducts.
Bile duct adenomas are rare and are usually found during cholecystectomy. They can present at any segment of the extrahepatic biliary tree1. The majority of patients present with obstructive jaundice, as the main manifestation. Those adenomas can be confused with malignant lesions, such as cholangiocarcinoma, lymphoma, and carcinoid tumors. There is little knowledge about the management of bile duct adenomas and the frequency of malignant transformation has not been determined. Risk is higher in tubular lesions2,3. Immunohistochemistry plays an essential role in the evaluation of gastrointestinal tumors. It differentiates benign conditions from malignant diseases, can determine tumor origin and subclassify the lesions, and is crucial for guiding the approach to patients and their management4. Treatment has not been defined in any guidelines and surgical resection is the main treatment in the majority of the reports in the literature5–7. Roux-en-Y anastomosis and endoscopic resection or ablation have been described in some reports. Nevertheless, there is little information, with respect to the long term, on the follow-up and progression of those patients8.
Financial disclosureNo financial support was received in relation to this article.
Conflict of interestThe authors declare that there is no conflict of interest.
Please cite this article as: Ruiz-Ballesteros E, Keil-Ríos D, Farca-Belsaguy A, Vilatobá-Chapa M, Baquera-Heredia JJ. Adenocarcinoma invasivo de la vía biliar extrahepática. Revista de Gastroenterología de México. 2021;86:451–453.