Hemangioma is the most common benign liver tumor. Incidence ranges from 0.4% to 20% in the general population and is predominant in females, with a 5:1 female-to-male ratio.
Diagnosis is based on clinical presentation, physical examination, and imaging studies (hepatobiliary ultrasound, intravenous contrast abdominal computed tomography, and/or magnetic resonance imaging). Treatment includes both conservative and surgical management1. Surgical treatment is reserved for patients with tumors >5 cm2 and for patients whose symptomatology compromises their quality of life3.
Laparoscopic liver resection (LLR) is the preferred surgical approach, given that it has the advantages of less intraoperative blood loss, a reduced need for transfusion, and less postoperative pain and morbidity4.
LLR for giant tumors (>10 cm) that are close to vascular structures or in technically difficult segments, can be performed at referral centers by experienced surgeons, with no increase in postoperative morbidity or mortality5.
Ban et al. proposed a scoring system for evaluating the difficulty of a given LLR, grading the level of difficulty as low, intermediate, or high. They found that the level of difficulty directly correlated with intraoperative blood loss, surgery duration, and hospital stay (p < 0.001)6.
We present herein the case of a 65-year-old woman that had a past medical history of high blood pressure and allergy to penicillin and a past surgical history of total abdominal hysterectomy secondary to uterine prolapse and laparoscopic cholecystectomy secondary to chronic cholecystitis due to gallstones.
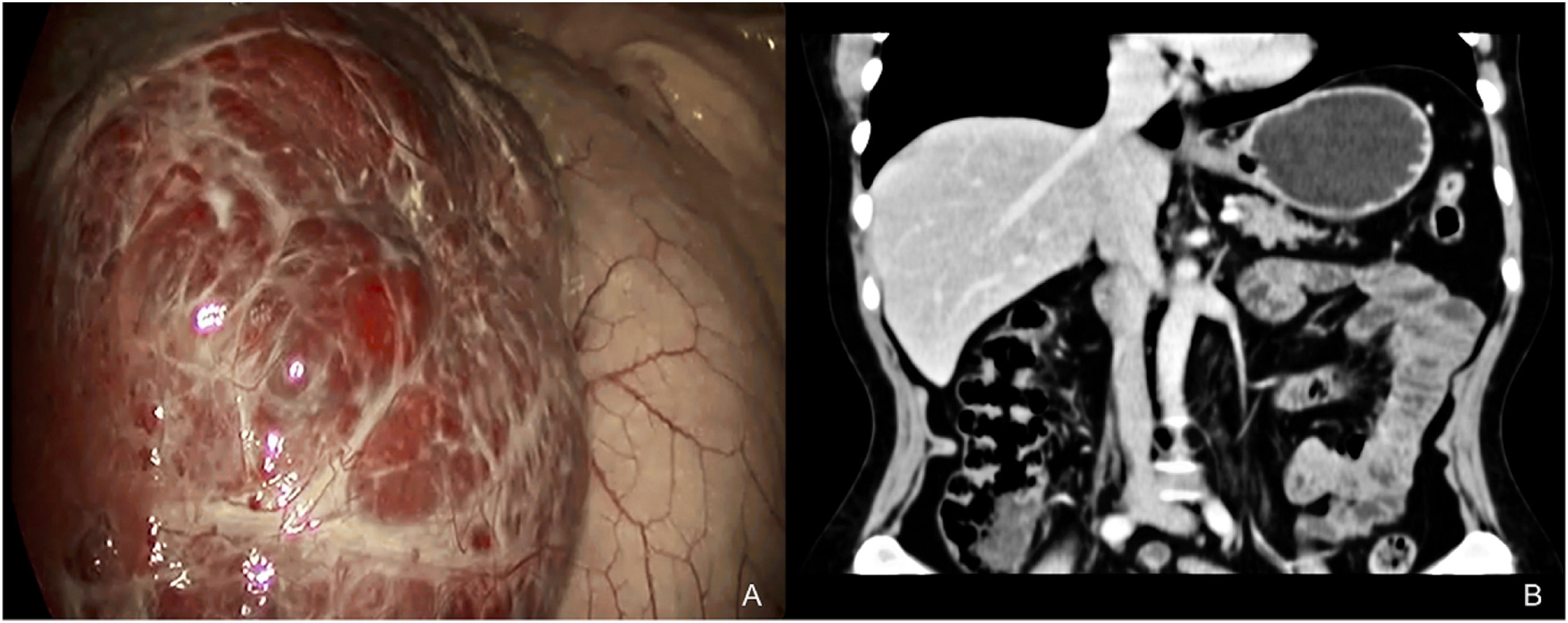
The patient was referred to our hospital for epigastric pain of two-year progression. Liver hemangioma was diagnosed through a tomography scan, with the characteristic uptake of contrast medium, involving segments II and III, and measuring 95 × 98 × 90 mm (Fig. 1A and B).
Laboratory test results showed hemoglobin 14.9 g/dL, hematocrit 44.5%, leukocytes 10,700 cells/µL, platelets 233,000 cells/µL, glucose 101 mg/dL, creatinine 0.71 mg/dL, sodium 142 mEq/L, potassium 3.9 mEq/L, alanine aminotransferase 15 U/L, aspartate aminotransferase 16 U/L, lactate dehydrogenase 293, total bilirubin 0.56 mg/dL, prothrombin time 13.2 s, partial thromboplastin time 27.5 s, and INR 0.98.
Laparoscopic left lateral segmentectomy was performed on June 6, 2019, with a two 12 mm port approach. The first port was placed at the supraumbilical right paramedian level and the second at the supraumbilical left paramedian level. An additional 5 mm epigastric trocar and 5 mm right subcostal trocar were placed.
A liver hemangioma measuring 14 × 11 × 10 cm was found during the surgery that completely involved segments II and III (Fig. 2A).
Lateral segment resection was performed using the laparoscopic SONOCA 400 ultrasonic aspirator/dissector (Söring®), the Sonicision ultrasonic dissection system (Medtronic®), a monopolar hook, bipolar energy, and a white cartridge linear stapler (Covidian®) to control the left suprahepatic vein. The surgical specimen was extracted through a 6 cm infraumbilical median incision. Surgery duration was 140 min, with blood loss of 300 mL. The Pringle maneuver was not performed.
The patient’s postoperative progression was satisfactory and oral diet was begun on postoperative day one. There were no signs of complications, and so she was released on postoperative day three.
During the postoperative outpatient follow-up, the patient was asymptomatic, with improved quality of life. At postoperative year one, the patient has had no symptoms and the control tomography scan showed no tumor recurrence (Fig. 2B).
LLR is currently the standard treatment for benign liver tumors2. Its benefits regarding postoperative morbidity include less postoperative pain, early return to oral diet, and reduced hospital stay4. In a study that compared posterosuperior and anterolateral segments in 197 patients, the anterolateral resections were less difficult technically, and had a lower conversion rate and shorter surgery duration (p < 0.001)7. The decision was made to operate on the patient at our tertiary care referral center, given that the procedure is classified as having an intermediate level of difficulty6.
The presence of symptoms is the most frequent indication for the resection of benign liver tumors. Pain is the most common symptom of said pathology. Surgery resolves the symptoms in 81.3% of patients2, and therefore, is considered the treatment of choice in symptomatic patients.
Schnelldorfer et al. compared expectant management with surgical treatment in patients with giant liver hemangioma. No differences were observed in relation to the complication rate, but the surgical group had presented with more severe preoperative symptoms, thus the authors concluded that surgical treatment should be reserved for those patients3.
Even though some authors consider that hybrid surgical techniques are associated with better outcomes than traditional laparoscopic surgery8, no clear benefit has been observed. However, they have been reported to be a useful resource in acquiring laparoscopic technical skill5.
LLR has become the standard treatment in benign liver tumors, given its clear benefit with respect to postoperative patient progression. Ours is the first case of giant liver hemangioma treated through a minimally invasive technique described in Mexico. Even though greater experience is required at our center, LLR can be performed safely in selected patients, with good postoperative outcomes.
Ethical considerationsInformed consent was requested of the patient described in the present article. She was above 18 years of age and mentally competent to grant its authorization.
The present work meets the current bioethics research regulations. Approval by an ethics committee was not needed, given the observational nature of the study and the fact that it involved no diagnostic/therapeutic interventions carried out on the patient.
The authors declare that the present article contains no personal data of any type within the text or annexed to it that could identify the patient.
Financial disclosureNo funding was required for the present article.
Conflict of interestThe authors declare that there is no conflict of interest.
Please cite this article as: Beristain-Hernández JL, Mora-Muñoz VS, García-Sánchez M. Segmentectomía lateral izquierda laparoscópica por un hemangioma hepático gigante. Rev Gastroenterol México. 2021;86:448–450.