Invasive management of pancreatic pseudocysts (PP) is currently indicated in those patients with symptoms or complications. Treatment options are classified as surgical (open and laparoscopic) and non-surgical (endoscopic and radiologic).
AimTo describe the morbidity, mortality, and efficacy in terms of technical and clinical success of the laparoscopic surgical approach in the treatment of patients with PP in the last 3 years at our hospital center.
MethodsWe included patients with PP treated with laparoscopic surgery within the time frame of January 2012 and December 2014. The morbidity and mortality associated with the procedure were determined, together with the postoperative results in terms of effectiveness and recurrence.
ResultsA total of 38 patients were diagnosed with PP within the last 3 years, but only 20 of them had invasive treatment. Laparoscopic surgery was performed on 17 of those patients (mean pseudocyst diameter of 15.3, primary drainage success rate of 94.1%, complication rate of 5.9%, and a 40-month follow-up).
ConclusionsThe results obtained with the laparoscopic technique used at our hospital center showed that this approach is feasible, efficacious, and safe. Thus, performed by skilled surgeons, it should be considered a treatment option for patients with PP.
Actualmente el manejo invasivo de los seudoquistes pancreáticos (SP) está indicado en aquellos que ocasionan síntomas en el paciente o que desarrollan complicaciones. Las opciones de tratamiento se clasifican en quirúrgicas (convencionales y laparoscópicas) y no quirúrgicas (endoscópicas y radiológicas).
ObjetivoDescribir la morbilidad, la mortalidad y la eficacia en términos de éxito técnico y clínico del abordaje quirúrgico laparoscópico en el tratamiento de los pacientes con SP de los últimos 3 años en el hospital sede.
Materiales y métodosSe incluyeron pacientes con SP tratados de manera quirúrgica laparoscópica en el periodo comprendido de enero de 2012 a diciembre de 2014. Se determinó la morbimortalidad asociada al procedimiento y los resultados posquirúrgicos en términos de efectividad y recurrencia.
ResultadosTreinta y ocho pacientes fueron diagnosticados con SP en los últimos 3 años de los cuales 20 tuvieron indicación de tratamiento invasivo; a 17 se les sometió a tratamiento quirúrgico laparoscópico (diámetro promedio del SP 15.3cm, éxito primario de drenaje del 94.1%, el 5.9% presentó complicaciones, 40 meses de seguimiento).
ConclusionesLos resultados obtenidos con la técnica laparoscópica utilizada en el hospital sede demuestran que dicho abordaje es factible, eficaz y seguro; por lo que, en manos expertas debe considerarse como una opción para el tratamiento de pacientes con SP.
Pancreatic and peripancreatic collections are divided into 4 categories (acute collections, post-necrotic acute collections, pancreatic pseudocysts [PPs], and encapsulated pancreatic necrosis). At present, PPs are the most common cause of cystic lesions of the pancreas.1,2
Current PP management indications are based on the presence of symptoms (abdominal pain, early satiety, weight loss, persistent fever) or complications (infection, gastric or biliary obstruction, rupture, vascular thrombosis, or pseudoaneurysm formation).3,4
Treatment options for PPs are classified as surgical (open and laparoscopic) and nonsurgical (endoscopic and radiologic).5,6
Internal drainage of PPs through conventional open surgery was first described in 1923 when Jedlica published the cystogastrostomy technique.7 In 1996 Gumaste et al. published a systematic review of the literature that included 1,032 patients from 14 different studies that underwent conventional open surgery for internal PP drainage and reported morbidity of 40% and mortality of 5.8%.8
Because of this elevated morbidity and mortality rate, in the 1990s interest was sparked in developing minimally invasive surgical treatment options that resulted in the description of different internal drainage techniques with the laparoscopic approach, such as laparoscopic posterior or exogastric cystogastrostomy reported by Morino et al. in 1995 and by Park and Schwartz in 1999, transgastric or anterior cystogastrostomy, endogastric cystogastrostomy, and cystojejunostomy with a Roux-en-Y jejunal loop.9,10
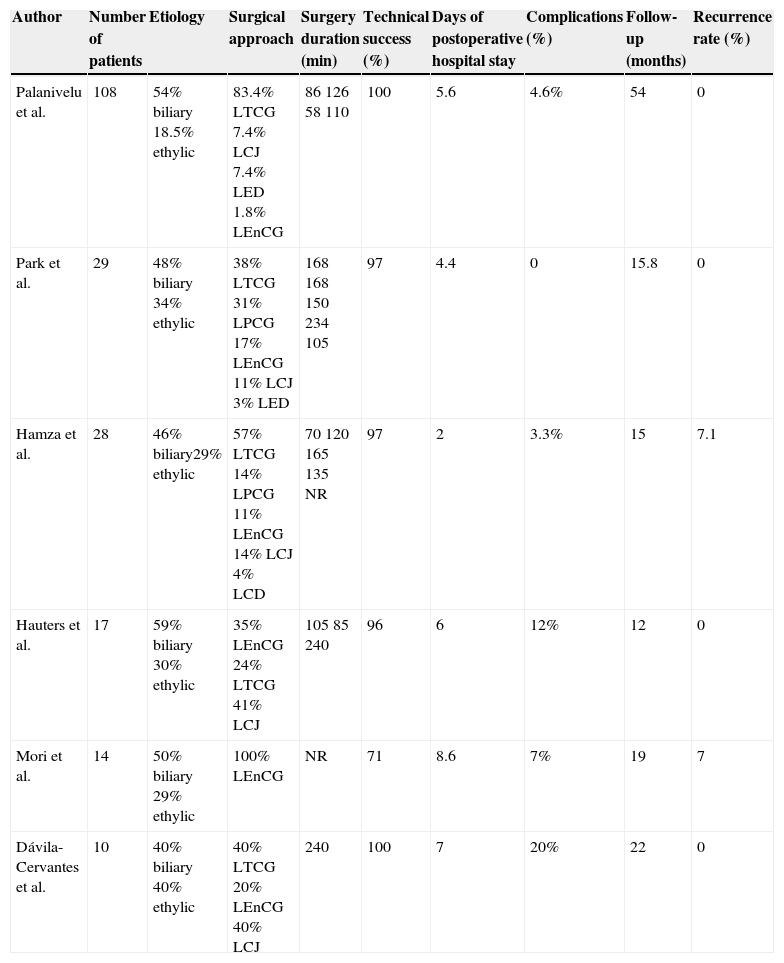
Since then, there have been numerous case series describing the success and morbidity and mortality rates of different laparoscopic drainage techniques (table 1). In 2007 Aljarabah and Ammori carried out a systematic review of the literature and reported complication, mortality, and recurrence rates of 4.6, 0, and 0%, respectively, in patients with laparoscopically treated PP.11
Laparoscopic pancreatic pseudocyst treatment case series.
| Author | Number of patients | Etiology | Surgical approach | Surgery duration (min) | Technical success (%) | Days of postoperative hospital stay | Complications (%) | Follow-up (months) | Recurrence rate (%) |
|---|---|---|---|---|---|---|---|---|---|
| Palanivelu et al. | 108 | 54% biliary 18.5% ethylic | 83.4% LTCG 7.4% LCJ 7.4% LED 1.8% LEnCG | 86 126 58 110 | 100 | 5.6 | 4.6% | 54 | 0 |
| Park et al. | 29 | 48% biliary 34% ethylic | 38% LTCG 31% LPCG 17% LEnCG 11% LCJ 3% LED | 168 168 150 234 105 | 97 | 4.4 | 0 | 15.8 | 0 |
| Hamza et al. | 28 | 46% biliary29% ethylic | 57% LTCG 14% LPCG 11% LEnCG 14% LCJ 4% LCD | 70 120 165 135 NR | 97 | 2 | 3.3% | 15 | 7.1 |
| Hauters et al. | 17 | 59% biliary 30% ethylic | 35% LEnCG 24% LTCG 41% LCJ | 105 85 240 | 96 | 6 | 12% | 12 | 0 |
| Mori et al. | 14 | 50% biliary 29% ethylic | 100% LEnCG | NR | 71 | 8.6 | 7% | 19 | 7 |
| Dávila-Cervantes et al. | 10 | 40% biliary 40% ethylic | 40% LTCG 20% LEnCG 40% LCJ | 240 | 100 | 7 | 20% | 22 | 0 |
LCD: Laparoscopic cystoduodenoscopy; LCJ: Laparoscopic cystojejunoscopy; LED: Laparoscopic external drainage; LEnCG: Laparoscopic endogastric cystogastrostomy; LPCG: Laparoscopic posterior cystogastrostomy; LTCG Laparoscopic transgastric cystogastrostomy; NR: Not reported.
In 2014 Khaled published a retrospective study that directly compared the laparoscopic surgical technique with the conventional open approach for PP treatment and concluded that the former offered advantages in terms of shorter surgery duration, a lower morbidity rate, and shorter hospital stay, and therefore should be considered the first choice approach in centers that have the adequately trained personnel.12
Minimally invasive treatment techniques have recently been described for pancreatic and peripancreatic collections different from PP. In 2010 Van Santvoort et al. carried out a multi-center, prospective, randomized study showing that patients with infected necrotic pancreatitis treated through a minimally invasive technique (the step-up approach) using computerized axial tomography-guided fine needle aspiration and/or laparoscopic necrosectomy had a lower rate of multiple organ failure, a lower incidence of incisional hernia, and a lower incidence of new-onset diabetes than the patients treated through open necrosectomy.13
AimOur aim was to describe the morbidity, mortality, and efficacy in terms of technical and clinical success associated with the laparoscopic surgical approach in patients with PP treated at the Hepatobiliary and Pancreatic Clinic of our hospital center over the last 3 years.
MethodsA retrospective, cross-sectional, observational, and descriptive study was conducted. The case records were reviewed of the patients 18 years of age or older that were diagnosed with PP and treated through laparoscopic posterior cystogastrostomy at our hospital center within the time frame of January 2012 and December 2014.
A contrast-enhanced computerized axial tomography scan was carried out on the patients with a history of acute pancreatitis that were seen as outpatients 4 weeks after the inflammatory pancreatic event and presented with epigastric pain, early satiety, or persistent fever. PP was defined as a peripancreatic collection meeting the following tomographic criteria: round or oval, with a well-defined wall, content with a fluid density in Hounsfield units, and no evidence of solid debris or necrotic tissue in its interior. Infected PP was defined as a collection presenting tomographic evidence of gas in its interior.
The patients that fit the abovementioned criteria underwent internal drainage through laparoscopic cystogastrostomy as a first treatment option, performed by a surgeon and an assistant. The technique employed at our hospital center is described in detail in the 2012 Revista Mexicana de Gastroenterología14 and the most important steps are the following: with the patient under general anesthesia, the pneumoperitoneum is insufflated with a Veress needle, inserting a 10mm supraumbilical optical port and three 5mm working ports at the subxiphoid location and the mid-clavicular line in the right and left subcostal regions, respectively. To gain access to the pancreas, the gastrocolic ligament is dissected with monopolar and bipolar cautery. The posterior surface of the stomach and the anterior surface of the pseudocyst are located and dissected. The pseudocyst is incised using a monopolar hook and its content is aspirated. The posterior surface of the stomach is then incised at the level corresponding to the incision in the wall of the PP. A 3cm anastomosis is performed with 0 polypropylene separate sutures using an extracorporeal Gea knot. The procedure is finished by placing 2 Jackson-Pratt drains at the surgical site and closing the aponeurosis with Vicryl 1 and the skin with 3-0 polypropylene simple sutures. In cases with a biliary etiology of the patient's acute pancreatitis episode culminating in PP formation, conventional laparoscopic cholescystectomy following the Strasberg principles was performed as the initial step of the surgical procedure.
Patients resumed oral intake in the postoperative period as soon as gastrointestinal function was recovered (bowel sounds and the passage of flatus) and they were released from the hospital when they tolerated that diet and the drains had a serous output under 100 cc for 24h (the drains were removed on the day of release).
The drained pseudocyst diameter (measured through tomography), the percentage of conversion to open surgery, primary drainage success defined as the clinical and tomographic resolution of the pseudocyst in a single surgery, surgery duration, intraoperative blood loss, days of postoperative hospital stay, and complications requiring surgical or endoscopic intervention under general anesthesia (III b according to the Clavien-Dindo classification) during the first 30 postoperative days were recorded.
Outpatient follow-up consisted of monthly consultations for the first 6 postoperative months and then appointments every 3 months. At each consultation the patient was asked about possible recurrence symptoms, such as early satiety, abdominal pain, and weight loss. In addition, control tomography scans were done at the 2nd and 6th months of follow-up. Recurrence was considered if there were persistent symptoms or tomographic evidence of residual pseudocyst during the follow-up.
Statistical analysisThe data were registered on a data collection sheet specifically designed for this line of investigation and then put in a database (Microsoft Excel; Microsoft Corporation, Seattle, WA, USA). Descriptive statistics with simple percentages, means, and minimum and maximum values were used for establishing the results of the laparoscopic surgical approach in the treatment of patients with PP.
ResultsA total of 38 patients diagnosed with PP were attended to at our hospital center over the last 3 years. Twenty-three were men and 15 were women and their mean age was 38.8 years (13-76 years).
A total of 18 patients (47.3%) did not meet the criteria for invasive management and remained under surveillance. The peripancreatic collection was reabsorbed in 100% of the cases and there were no remaining or residual local complications. Twenty patients (52.7%) met the criteria for invasive management (symptoms and complications).
Of the 20 patients that required invasive management, 13 (64%) had a history of acute biliary pancreatitis. Of those patients, the underlying etiology of the acute pancreatitis was alcohol-related in 6 (32%) and in one (4%) it was due to hypertriglyceridemia. Of the 20 patients, 13 were men and 7 were women.
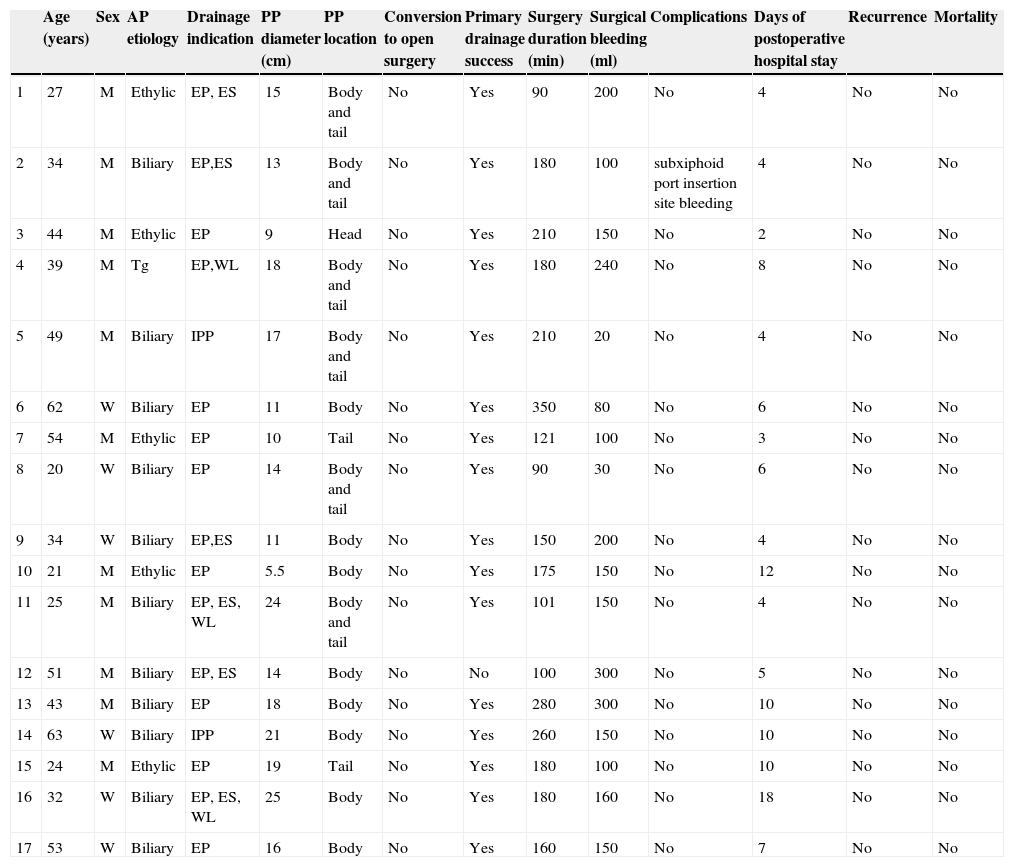
In the group of patients requiring invasive management, 17 (77.2%) underwent laparoscopic posterior cystogastrostomy as the first treatment option (table 2). The indication for invasive treatment was the presence of symptoms in 88.2% of the patients and infected pseudocyst in the remaining 11.8%. Of those patients, 11 were men and 6 were women and their mean age was 39.7 years (20-63 years). Acute pancreatitis etiology was biliary in 64.7% of the cases, alcohol-related in 29.4%, and due to hypertriglyceridemia in 5.8%.
Patients with pancreatic pseudocyst treated through the laparoscopic surgical approach at our hospital center.
| Age (years) | Sex | AP etiology | Drainage indication | PP diameter (cm) | PP location | Conversion to open surgery | Primary drainage success | Surgery duration (min) | Surgical bleeding (ml) | Complications | Days of postoperative hospital stay | Recurrence | Mortality | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 27 | M | Ethylic | EP, ES | 15 | Body and tail | No | Yes | 90 | 200 | No | 4 | No | No |
| 2 | 34 | M | Biliary | EP,ES | 13 | Body and tail | No | Yes | 180 | 100 | subxiphoid port insertion site bleeding | 4 | No | No |
| 3 | 44 | M | Ethylic | EP | 9 | Head | No | Yes | 210 | 150 | No | 2 | No | No |
| 4 | 39 | M | Tg | EP,WL | 18 | Body and tail | No | Yes | 180 | 240 | No | 8 | No | No |
| 5 | 49 | M | Biliary | IPP | 17 | Body and tail | No | Yes | 210 | 20 | No | 4 | No | No |
| 6 | 62 | W | Biliary | EP | 11 | Body | No | Yes | 350 | 80 | No | 6 | No | No |
| 7 | 54 | M | Ethylic | EP | 10 | Tail | No | Yes | 121 | 100 | No | 3 | No | No |
| 8 | 20 | W | Biliary | EP | 14 | Body and tail | No | Yes | 90 | 30 | No | 6 | No | No |
| 9 | 34 | W | Biliary | EP,ES | 11 | Body | No | Yes | 150 | 200 | No | 4 | No | No |
| 10 | 21 | M | Ethylic | EP | 5.5 | Body | No | Yes | 175 | 150 | No | 12 | No | No |
| 11 | 25 | M | Biliary | EP, ES, WL | 24 | Body and tail | No | Yes | 101 | 150 | No | 4 | No | No |
| 12 | 51 | M | Biliary | EP, ES | 14 | Body | No | No | 100 | 300 | No | 5 | No | No |
| 13 | 43 | M | Biliary | EP | 18 | Body | No | Yes | 280 | 300 | No | 10 | No | No |
| 14 | 63 | W | Biliary | IPP | 21 | Body | No | Yes | 260 | 150 | No | 10 | No | No |
| 15 | 24 | M | Ethylic | EP | 19 | Tail | No | Yes | 180 | 100 | No | 10 | No | No |
| 16 | 32 | W | Biliary | EP, ES, WL | 25 | Body | No | Yes | 180 | 160 | No | 18 | No | No |
| 17 | 53 | W | Biliary | EP | 16 | Body | No | Yes | 160 | 150 | No | 7 | No | No |
AP: Acute pancreatitis; EP: Epigastric pain; ES: Early satiety; IPP: Infected Pancreatic pseudocyst; M: Men; PP: Pancreatic pseudocyst; Tg: Triglycerides; W: Women; WL: Weight loss.
The mean transverse length of the laparoscopically-drained pseudocysts was 15.3cm (5.5-25cm). The entire procedure was laparoscopic and there was no need for conversion to open surgery in any of the 17 cases. The pseudocyst was resolved in 16 patients (94.1%) with a single surgical intervention (primary drainage success). In the remaining case (5.9%), despite having a preoperative computerized axial tomography scan that showed a collection with fluid content and no necrosis, abundant necrotic detritus was encountered during the procedure. Once the detritus was debrided, the cystogastrostomy continued with the previously described technique. In the postoperative period the patient presented with obstruction of the anastomosis by necrotic debris, which was resolved through endoscopic dilation. The mean surgery duration was 177min (range: 90-350min), being longer in the first cases. The mean intraoperative blood loss was 151ml (20-300ml).
Only one patient (5.9%) had a complication associated with the procedure. Due to the presence of blood output through the drain, he underwent a diagnostic laparoscopy that revealed bleeding from the subxiphoid trocar insertion site, which was controlled laparoscopically.
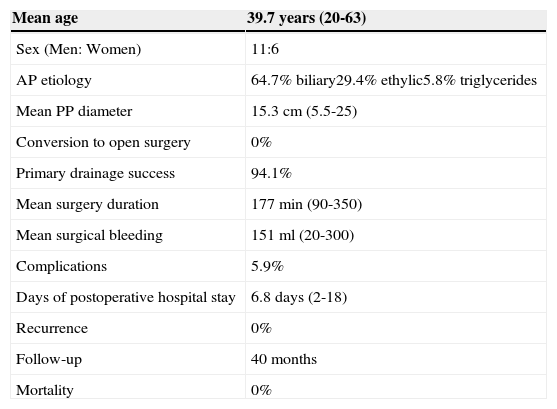
Postoperative hospital stay was a mean of 6.8 days (2-18 days). The current follow-up period is 40 months and so far no disease recurrence has been registered (table 3).
Results of the laparoscopic surgical approach.
| Mean age | 39.7 years (20-63) |
|---|---|
| Sex (Men: Women) | 11:6 |
| AP etiology | 64.7% biliary29.4% ethylic5.8% triglycerides |
| Mean PP diameter | 15.3cm (5.5-25) |
| Conversion to open surgery | 0% |
| Primary drainage success | 94.1% |
| Mean surgery duration | 177min (90-350) |
| Mean surgical bleeding | 151ml (20-300) |
| Complications | 5.9% |
| Days of postoperative hospital stay | 6.8 days (2-18) |
| Recurrence | 0% |
| Follow-up | 40 months |
| Mortality | 0% |
AP: acute pancreatitis; PP: pancreatic pseudocyst
This is the largest published case series to date in a Mexican population on the laparoscopic surgical treatment of PPs. In 2004 Dávila-Cervantes et al. reported complications of 20% and 0% recurrence in 22 months of follow-up on 10 Mexican patients with PP treated through laparoscopic internal drainage.15
Our data show that the minimally invasive technique for treating patients with PP employed at our hospital center is a feasible, safe, and effective option in our medical environment and the results are comparable to those published in the largest and most recent article on laparoscopic drainage of PP. In that case series by Palanivelu et al., which included 108 patients, they reported a mean postoperative hospital stay of 5.6 days and conversion, morbidity, mortality, and recurrence rates of 0, 8.3, 0, and 1%, respectively.16
It is important to point out that in contrast to the other case series published in the international literature that use different types of laparoscopic internal drainage (transgastric cystogastroscopies, cystojejunoscopies, etc.), only one laparoscopic technique (posterior cystogastrostomy) is used at our hospital, which facilitates the teaching/learning process and the reproducibility of the technique.
Minimally invasive management (laparoscopic and endoscopic) of PPs is currently gaining ground over the open approach.12 In 2013, Varadarajulu et al. published a randomized, prospective study that compared a minimally invasive approach (endoscopic drainage) with the conventional surgical approach, showing that in select cases, endoscopic management achieves the same success rates as conventional surgical treatment, but with fewer days of hospital stay and a lower economic cost.17
It remains to be established whether one minimally invasive treatment modality is superior to another. In 2009 Melman conducted a retrospective study comparing laparoscopic drainage with endoscopic drainage. He concluded that the primary success rate for PP drainage was statistically superior with the surgical approach.5
ConclusionsThe results obtained with the laparoscopic posterior cystogastrostomy technique at our hospital center showed that this approach in our environment is feasible, safe, and effective, and in skilled hands, should be considered a treatment option for patients with PP. Our technique has the added advantage of being standardized and thus facilitates the teaching/learning process of the procedure, making our hospital a human health resource formation center for the minimally invasive treatment of this pathology in the Mexican population.
Ethical responsibilitiesProtection of persons and animalsThe authors declare that no experiments were performed on humans or animals for this study.
Data confidentialityThe authors declare that they have followed the protocols of their work center in relation to the publication of patient data.
Right to privacy and informed consentThe authors have obtained the informed consent of the patients and/or subjects referred to in the article. This document is in the possession of the corresponding author.
Financial disclosureNo financial support was received in relation to this study/article.
Conflict of interestThe authors declare that there is no conflict of interest.
Please cite this article as: Crisanto-Campos BA, Arce-Liévano E, Cárdenas-Lailson LE, Romero-Loera LS, Rojano-Rodríguez ME, Gallardo-Ramírez MA, et al. Manejo laparoscópico de los seudoquistes pancreáticos: experiencia de un hospital general en la Ciudad de México. Revista de Gastroenterología de México. 2015;80:198–204.