The presence of a family history implies an increased risk for developing colorectal cancer (CRC), and may require a different screening strategy.
The aim of this study was to evaluate lesions found during colonoscopies of patients that had a family history of CRC.
Material and methodsA retrospective study was conducted that included consecutive colonoscopies performed on patients with a family history of CRC at a referral center within the period from April 2000 to January 2012. The colonoscopic findings were analyzed in relation to sex, age, and the presence or absence of symptoms.
ResultsData from 3,792 colonoscopies were collected. The mean age of the patients was 53.14 years (SD 12.22), and 57.4% were women. Colonoscopy was normal in 71.7% of the cases, with hyperplastic polyps being detected in 7.1%, and adenomatous polyps in 19.8% (39.4% of them were high risk). There was a 1.5% presence of adenocarcinomas in the subjects. Polyps and CRC were predominant in men (P=.001 and P=.027, respectively) and there was a linear increase with age. Symptomatic patients had a higher CRC detection rate (P<.001), but no differences were observed in relation to polyp diagnosis.
ConclusionsAge and male sex increased the risk for presenting with CRC or adenomas in the group of patients with a family history of CRC, and the presence of symptoms was associated with a greater risk for presenting with CRC.
La presencia de antecedentes familiares implica un riesgo aumentado de presentar colorrectal (CCR), lo que condiciona una estrategia de cribado diferente.
El objetivo de este trabajo fue evaluar las lesiones halladas en las colonoscopias de pacientes que se sometieron a esta exploración y que tuvieron antecedentes familiares para CCR.
Material y métodosSe realizó un estudio retrospectivo incluyendo las colonoscopias consecutivas realizadas en un centro de referencia desde abril del 2000 hasta enero del 2012 en pacientes con antecedentes familiares de CCR. Los hallazgos encontrados en la colonoscopia se analizaron en función del sexo, la edad y la presencia o ausencia de síntomas.
ResultadosSe recogieron datos de 3,792 colonoscopias. La edad media ± desviación estándar de los pacientes fue de 53.14 ± 12.22 años, siendo el 57,4% mujeres. La colonoscopia fue normal en el 71.7% de los casos, se detectaron pólipos hiperplásicos en el 7.1% y pólipos adenomatosos en el 19.8% (39.4% de ellos, de alto riesgo). La presencia de adenocarcinomas se evidenció en el 1.5% de los sujetos. La presencia de pólipos y CCR predomina en varones (p=0.001 y p=0.027, respectivamente) y aumentan de forma lineal con la edad. En los pacientes sintomáticos hubo mayor tasa de detección de CCR (p<0.001), mientras que no se observaron diferencias para el diagnóstico de pólipos.
ConclusionesEn el grupo de pacientes con antecedentes familiares de CCR, la edad y el sexo masculino aumentan el riesgo de presentar CCR o adenomas. La presencia de síntomas se asocia a mayor riesgo de presentar CCR.
Colorectal cancer (CRC) is the third most frequent tumor in men and the second in women worldwide.1 Incidence is greater in men than in women with a ratio of 1.4:1. This tumor represents 8% of the overall mortality due to cancer, making it the 4th most common cause of death by cancer.2
The Health Sector in León, Spain, has rates that are standardized with those of the worldwide population, between 33.7 and 41.6 for men and 19.8 and 23 for women per 100,000 inhabitants. In this area of health, a study by Martin Sanchez et al. reported an increase in the incidence rate from the year 1994 to 2008.3 An increase in CRC incidence, prevalence, and mortality in men and their reduction in women are expected in the coming years.4 This upward trend is also observed in other regions of the world5 where similar genetic factors are presupposed.
The hereditary forms of CRC (mainly colorectal polyps and Lynch syndrome) make up 3% of the total cases of CRC. It is estimated that up to 30% of CRC cases in the Spanish population have family aggregation.6 The genetic profile of the familial forms are currently not well established. The implicated alleles are more common and have a lower penetration. Pangenomic association studies have recently identified how some single nucleotide polymorphisms could be associated with the excess of familial risk, enabling the classification of patients into subgroups according to their risk.7
The relatives of patients with CRC have an increased risk for presenting with this type of neoplasia, depending on the degree of the relation and the age at which the affected relative presents with the tumor.8 A prospective study by Ng et al.9 was recently published in which the siblings of patients with CRC had a 7.5% prevalence of advanced neoplasia, compared with 2.9% in controls. Knowing the risk for presenting with the disease in relatives of CRC patients implies a different screening strategy for early lesion detection.10
The aim of our study was to evaluate colonoscopy findings in patients with a family history (FH) of CRC and to analyze the factors associated with the presence of neoplastic lesions.
MethodsA retrospective study was conducted in which the colonoscopies performed at our center within the time frame of April 2000 and January 2012 on outpatients with a FH of CRC were reviewed. Asymptomatic patients, as well as patients that in addition to a FH also presented some symptom, were included in the study. The successive examinations of any given patient were excluded from the analysis. There was no active CRC screening program in place in our healthcare sector during the time frame of the study. The patients were referred from different specialized care consultations (mainly gastroenterology, surgery, and internal medicine) and primary care consultations.
The variables of sex and age of the patients were analyzed (dividing them into 3 groups for their evaluation: under 40 years of age, between 40 and 60 years of age, and over 60 years of age). The patients were divided into 2 groups for the analysis according to the presence or absence of symptomatology together with a FH of the disease. The purpose of this division was to distinguish those patients that came for screening from those that had symptoms; the FH was a complemetary datum.
In relation to the pathologic findings we distinguished the following groups according to the lesion grade found:
- 1.
Patients with a normal colonoscopy or extirpation of hyperplastic polyps.
- 2.
Patients with adenomas. This group included all types of adenomas, sizes, and dyplasia grades. Patients were considered to present with high-risk adenoma if they had at least one polyp larger than 1cm, more than 3 polyps, regardless of their size, or at least one polyp with high-grade dysplasia.
- 3.
Patients with a histology of either microinvading adenocarcinoma or infiltrating adenocarcinoma.
If a patient presented with several concomitant lesions, he or she was classified in the group of the lesion with the highest risk.
This study was approved by the Ethics Committee of our center in accordance with the guidelines of the 1975 Declaration of Helsinki.
Statistical analysisThe study variables were placed in an appropriately elaborated database (Microsoft Access) and analyzed using a statistical software package (SPSS v. 11.0 for MacOS X). The quantitative variables were expressed as means ± standard deviation and the categorical variables as counts (percentage).
The chi-square test was used for comparing the categorical variables and the quantitative variables were analyzed using the Student's t test. The chi-square test for linear trend was employed to test for linear trend, calculating the corresponding odds ratio (OR) of the case when possible. Statistical significance was set at a p < 0.05.
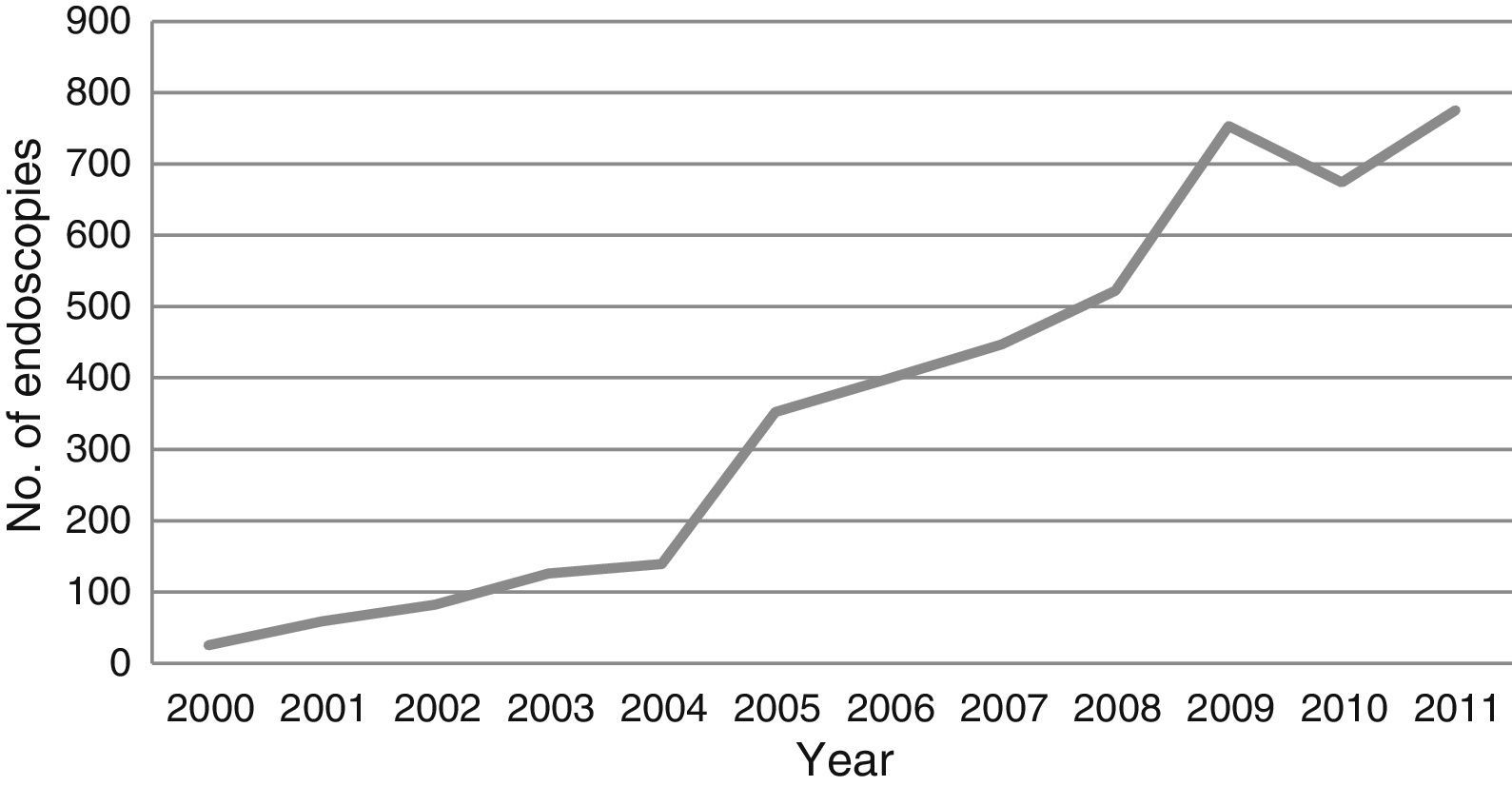
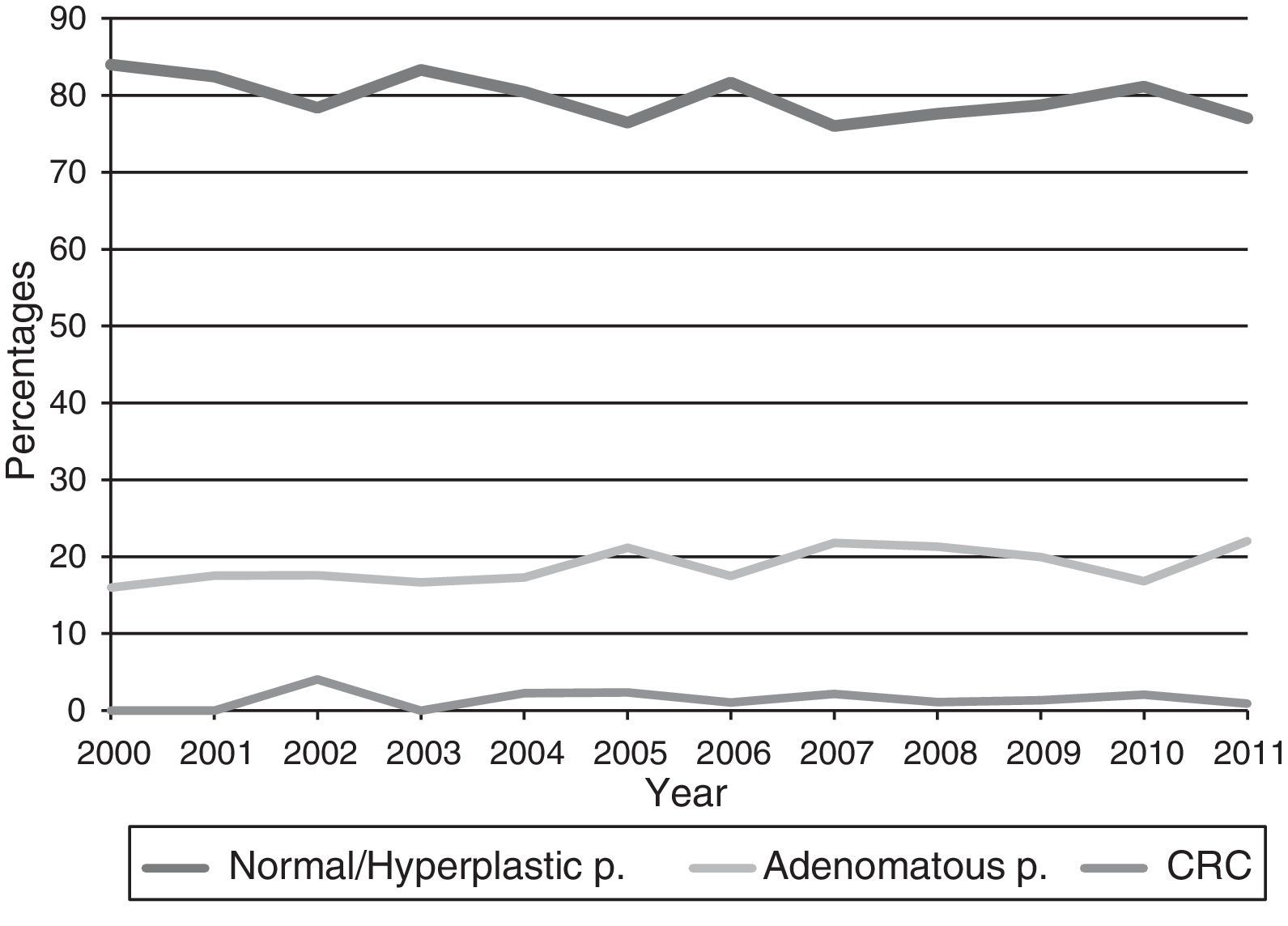
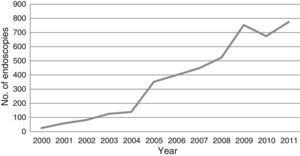
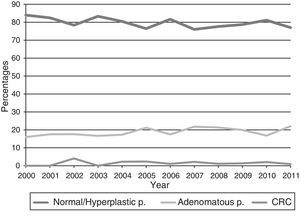
ResultsThe data from 4,408 colonoscopies were collected; 3,792 patients were finally analyzed after excluding the successive examinations of any given patient. Figure 1 shows the progression in time of the number of screening colonoscopies performed in relatives with or without symptoms. Linear growth has been observed in the number of colonoscopies ordered for this indication in the last few years. Figure 2 shows the percentages of the normal colonoscopies (hyperplastic polyps are included in this group) and the finding of adenomatous polyps and tumors during this same period.
The mean age of the patients was 53.14 ± 12.22 years and 57.4% of the patients were women. Colonoscopy was incomplete in 3.11% (118/3,792) of the cases. Pathologic findings were encountered in 28.3% of the patients globally. Colonoscopy revealed the following findings: normal in 2,717 subjects (71.7%), hyperplastic polyps in 269 (7.1%), and adenomatous polyps in 749 (19.8%). Of the adenomatous polyps, 295/749 (39.4% of all the adenomas) were high-risk. Adenocarcinoma was detected in 57 patients, representing 1.5% of the total.
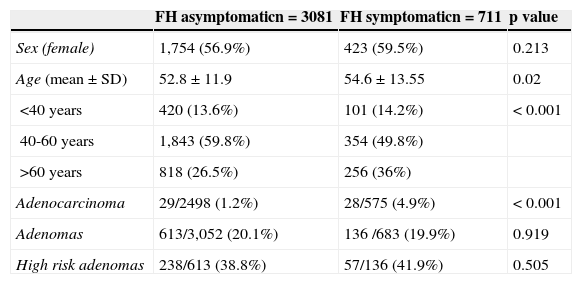
Table 1 shows the findings in relation to the presence or absence of symptoms. The groups were not comparable in regard to age and the older patients were in the symptomatic group. The symptomatic patients presented with a larger number of tumors and there were no differences in the presence of polyps in the two groups. With respect to the symptomatic patients with adenocarcinoma, 19 (67.9%) presented with rectorrhagia, 4 (14.2%) with anemia or iron deficiency, 3 (10.7%) had altered bowel habit, and 2 (7.1%) with general syndrome.
Group characteristics and colonoscopy findings according to the presence or absence of symptoms.
| FH asymptomaticn = 3081 | FH symptomaticn = 711 | p value | |
|---|---|---|---|
| Sex (female) | 1,754 (56.9%) | 423 (59.5%) | 0.213 |
| Age (mean ± SD) | 52.8 ± 11.9 | 54.6 ± 13.55 | 0.02 |
| <40 years | 420 (13.6%) | 101 (14.2%) | < 0.001 |
| 40-60 years | 1,843 (59.8%) | 354 (49.8%) | |
| >60 years | 818 (26.5%) | 256 (36%) | |
| Adenocarcinoma | 29/2498 (1.2%) | 28/575 (4.9%) | < 0.001 |
| Adenomas | 613/3,052 (20.1%) | 136 /683 (19.9%) | 0.919 |
| High risk adenomas | 238/613 (38.8%) | 57/136 (41.9%) | 0.505 |
FH asymptomatic: patients with a family history of the disease but without symptoms; FH symptomatic: patients with a family history of the disease and with symptoms.
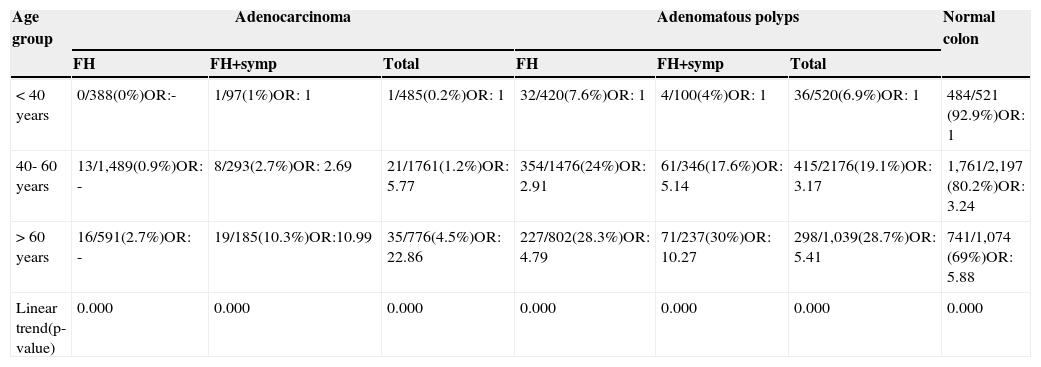
Table 2 shows the pathology found according to age group and the presence or absence of symptoms. The < 40 year age group presented with 6/36 (16.7%) (OR = 1) high-risk adenomas from the adenoma total (asymptomatic patients with FH: 3/32 [9.4%]; symptomatic patients with FH: 3/4 [75%]); the 40-50 year age group had 153/415 (36.9%) (OR = 2.92) (asymptomatic patients with FH:131/354 [37%]; symptomatic patients with FH: 22/346 [6.4%]), and the age group above 60 years had 136/298 (45.6%) (OR = 4.2) (asymptomatic patients with FH: 104/802 [12.9%]; symptomatic patients with FH: 32/71[45%]). There was a statistically significant linear trend in the patient total and in the asymptomatic patients with FH (p < 0.001), but not in the symptomatic patients with FH (p = 0.77).
Findings according to age distribution and the presence of symptoms.
| Age group | Adenocarcinoma | Adenomatous polyps | Normal colon | ||||
|---|---|---|---|---|---|---|---|
| FH | FH+symp | Total | FH | FH+symp | Total | ||
| < 40 years | 0/388(0%)OR:- | 1/97(1%)OR: 1 | 1/485(0.2%)OR: 1 | 32/420(7.6%)OR: 1 | 4/100(4%)OR: 1 | 36/520(6.9%)OR: 1 | 484/521 (92.9%)OR: 1 |
| 40- 60 years | 13/1,489(0.9%)OR: - | 8/293(2.7%)OR: 2.69 | 21/1761(1.2%)OR: 5.77 | 354/1476(24%)OR: 2.91 | 61/346(17.6%)OR: 5.14 | 415/2176(19.1%)OR: 3.17 | 1,761/2,197 (80.2%)OR: 3.24 |
| > 60 years | 16/591(2.7%)OR: - | 19/185(10.3%)OR:10.99 | 35/776(4.5%)OR: 22.86 | 227/802(28.3%)OR: 4.79 | 71/237(30%)OR: 10.27 | 298/1,039(28.7%)OR: 5.41 | 741/1,074 (69%)OR: 5.88 |
| Linear trend(p-value) | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 |
FH: patients with a family history of the disease but with no symptoms; FH + symp: patients with a family history of the disease and with symptoms.
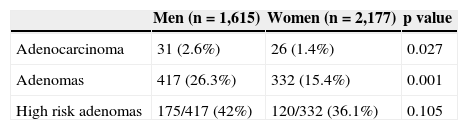
Table 3 shows the endoscopic findings by sex. The pathology predominated in men in relation to polyps and adenocarcinomas, whereas statistical significance was not achieved for high-grade polyps.
DiscussionThere has been an important increase in the number of colonoscopies performed on patients with a FH of CRC in the last few years. Our data revealed pathology in the examinations in 28.3% of the patients, diagnosing 19.8% with adenomas and 1.5% with adenocarcinomas. The presence of both lesions predominated in men and increased with age. Lesions in asymptomatic patients under 40 years of age was exceptional.
In spite of our results, we must take into account a series of limitations in regard to the methodology of the study. First of all, it is a retrospective study that is based on computerized data in which it was possible to omit the existence of a family history of disease when including symptomatic patients, resulting in selection bias. And the fact that we did not specify the patients’ symptoms could also consitute such bias, influencing the type of lesion found.
Second, given that a computerized register of the examinations prior to the year 2000 was not available, we do not know how many patients might have undergone previous examinations, or in which interval, which could also skew the results. Concerning the characterization of the index cases, the degree of family relation to the affected relative and his or her age were not entered into the database, invalidating this study for analyzing the risk conferred by kinship.
The risk for developing CRC in first-degree relatives has been evaluated in numerous studies and meta-analyses and is estimated to be between 2 and 3 times higher than in the general population.11 This risk increases the younger the age of the affected relative, as well as when there are 2 or more first-degree realtives diagnosed with this pathology. Baglietto et al.8 reported that the risk also appears to depend on the kinship; the relative who has an affected sibling is at greater risk (RR: 3.47 95% CI [2.24-5.4]) than when the affected relative is a parent (RR: 2.05 95% CI [1.63-2.09]).
In relation to the average-risk population, Strul et al.12 found a 2.6% prevalence of CRC in patients from 76-80 years of age, 1.2% in patients from 50 to 75 years of age, and no cases in patients from 40 to 49 years of age. CRC risk increases not only with age but also when there is a family history of CRC; another study reported a risk for CRC of 2.5% in the general population for patients > 75 years of age, 4.7% when there was a first-degree relative with the disease, and 9.6% if there were 2 or more affected relatives.13 Our study showed a 0.2% probability in patients < 40 years, which was equal to the published data showing an age-related increase (4.5% in patients > 60 years).
The prevalence of adenomas in patients with a first-degree FH is greater than that of the general population (OR 1.7 [95% CI 1.4-3.5]) and it increases with age: at 35 years (OR 0.06 [95% CI 0.04-0.08]), at 55 years (OR 0.19 [95% CI 0.15-0.23]), and at 75 years (OR 0.44 [95% CI 0.35-0.56]).14 Strul et al.12 found a prevalence of advanced adenoma of 2% in patients from 40-49 years, of 5.5% in patients from 50-75 years, and 11.7% in patients from 76 to 80 years, in a population with no FH of the disease. Gupta et al.15 analyzed the prevalence of adenomas in first-degree relatives from 40 to 49 years of age and obtained a higher prevalence of adenomas in the group with a family history of the pathology (26.7% vs 13.5%; p = 0.002), with no statistical significance for advanced adenomas. In our patient cohort only 6 patients under 40 years of age presented with advanced adenoma, making up 2% of the adenomas found in this age group. The number of high-risk adenomas was also observed to increase with the age of the patient.
With respect to the presence or absence of symptoms, our results determined that symptomatic patients had a higher incidence of CRC, with no differences in relation to the appearance of polyps. A recent systematic review16 concluded that only bleeding and weight loss were associated with the presence of CRC, albeit with a low predictive power (AUC 0.66 and 0.67, respectively). There was no evidence that bowel habit alteration, diarrhea, constipation, or abdominal pain were associated with this neoplasm. None of the symptoms analyzed showed an association with the presence of polyps. In our study the most prevalent symptom in the patients diagnosed with CRC was rectorrhagia (67.9%).
Colorectal cancer is a prevalent problem in our society. Knowledge of the prevalence of colonic lesions that these patients with a FH of the disease present with is necessary in order for guidelines to be adequately implemented in and adapted to our environment.17,18 The number of screening colonoscopies has increased in our unit in the last decade (currently it represents 20% of the work carried out there). Adequate implementation of the CRC guidelines is essential for resource adaptation, especially when 17%19 of colonoscopies performed for this purpose are not properly indicated, according to EPAGE II criteria.20
In conclusion, age increases the risk for presenting with CRC or adenomas in patients with a FH of CRC, in both asymptomatic and symptomatic patients, and there is a higher prevalence in the male sex. These findings support the implementation of a screening program in this high-risk population, adapting the resources and criteria in accordance with current guidelines. Despite the reports of advances that have been published, more prospective studies directed at determining which relatives are at greater risk for this disease are necessary.
Ethical responsibilitiesProtection of persons and animalsThe authors declare that the procedures followed conformed to the ethical standards of the responsible committee on human experimentation and were in accordance with the World Medical Association and the Declaration of Helsinki.
Data confidentialityThe authors declare that they have followed the protocols of their work center in relation to the publication of patient data.
Right to privacy and informed consentThe authors have obtained the informed consent of the patients and/or subjects referred to in the article. This document is in the possession of the corresponding author.
Financial disclosureNo financial support was received in relation to this study.
Conflict of interestThe authors declare that there is no conflict of interest.
Please cite this article as: Álvarez-Cuenllas B, Díez-Rodríguez R, Vaquero L, Pisabarros C, Aparicio M, Rodríguez-Martín L, et al. Análisis descriptivo de los hallazgos endoscópicos en pacientes con antecedentes familiares de cáncer colorrectal. Revista de Gastroenterología de México. 2015;80:192–197.