Orthotopic liver transplantation (OLT) is the treatment of choice for patients with end-stage liver disease, acute liver failure, hepatocellular carcinoma, and other liver diseases.1
However, the mortality rate for patients on the liver transplant waiting list has increased due to high demand and organ scarcity worldwide, including Mexico.2 To resolve this problem, efforts have been made to broaden the potential donor pool, including some donors considered “high risk” or marginal; for example, donors with positive blood cultures, whose organs can be safely transplanted, with the exception of those with sepsis and multiorgan failure at the time of procurement.3
We present herein the case of an OLT recipient whose donor had confirmed bacteremia due to multidrug-resistant (MDR) Acinetobacter baumannii (A. baumannii).
A 66-year-old man, whose current disease appeared in 2016, characterized by general malaise, variceal bleeding, ascites, and grade II hepatic encephalopathy. He was diagnosed with cirrhosis of the liver due to metabolic dysfunction-associated fatty liver disease (MAFLD), after ruling out other etiologies. Two years after his disease onset, the patient developed three lesions under 4cm, consistent with hepatocellular carcinoma. He received three sessions of locoregional treatment with transarterial embolization, with no complications. Six months after the final treatment, the patient maintained the Milan criteria and was evaluated for liver transplantation, with no contraindications. He was placed on the waiting list in 2019.
After three years on the waiting list, with no recurrence of hepatocellular carcinoma, the patient was offered an organ from a 56-year-old female donor. Overweight was her only comorbidity, and her blood group was compatible with his. The donor died from a hemorrhagic stroke and was maintained in the intensive care unit. Two days before brain death occurred, she had presented with fever. MDR A. baumannii that was only sensitive to tigecycline developed in her blood cultures. Treatment with that agent was begun and the central venous catheter was removed approximately 36h before liver procurement.
After a brief pretransplant evaluation of the donor, with laboratory tests and a macroscopically normal liver, the risks presented by the blood cultures were discussed with the patient and he accepted them. The transplant was performed in May of 2022. As preventive measures, the blood cultures were repeated in the donor the day of the procurement and baseline blood cultures were carried out on the recipient, the results of which were negative. Antimicrobial prophylaxis with tigecycline for seven days was indicated. The patient had an excellent posttransplant recovery. During his hospital stay, the patient did not present with fever or signs of systemic inflammatory response, nor was modification of the traditional immunosuppression regimen necessary. He was discharged eight days after the procedure and currently has no complications at month 10 of follow-up.
Even though organ transplantation is considered a life-saving procedure, it is not without risks. One of the goals of liver transplant programs is to minimize the risk for unanticipated disease transmission between donors and recipients, in order to reduce posttransplant morbidity/mortality, which has been reported at up to 22%.4
A variety of pathogens, such as viruses, bacteria, fungi, mycobacteria, and parasites, can be transmitted by the donor. A review of the literature showed that the definition of infection in organs from donors varies according to the hospital center, which explains the wide range of cases of infection (from 2.2% to 23%). Despite those differences, case series have demonstrated that bacterial infection transmission from the donor to the recipient is not common, reaching 6.2%.5
In our case report, the organ came from a female donor with documented MDR A. baumannii bacteremia. The recipient had excellent posttransplant progression, with no infectious complications, and antibiotic treatment was maintained for seven days.
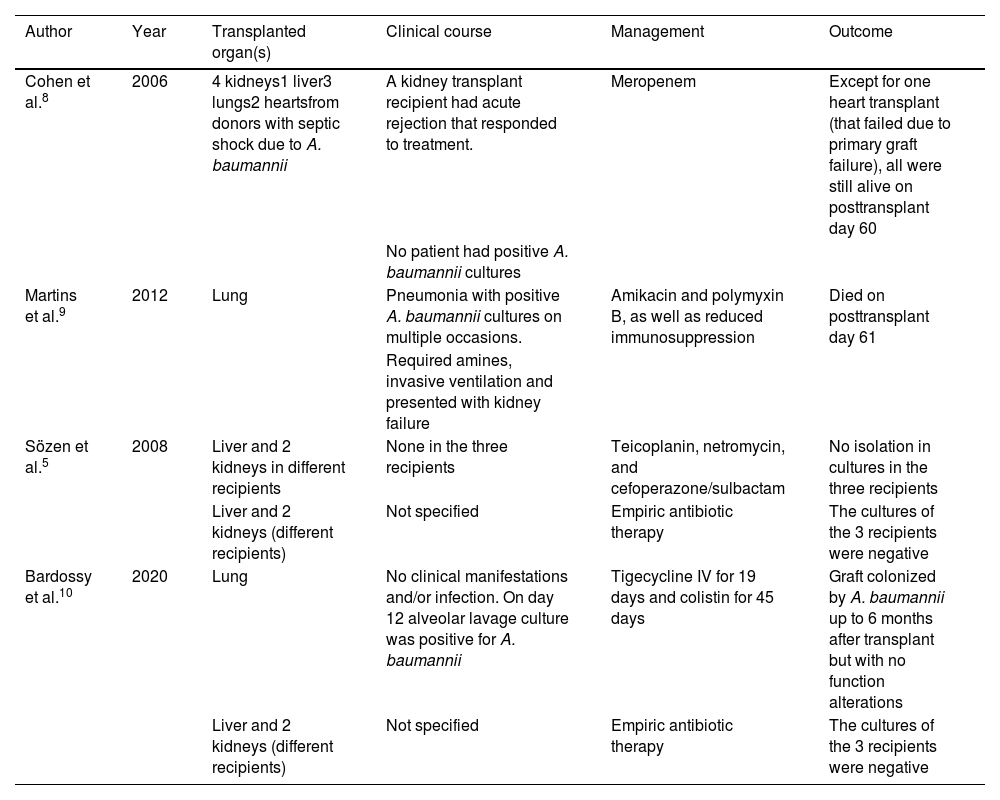
At present, numerous cases of solid organ transplantation from donors with positive blood cultures have been reported in the literature, and survival results are equal to those reported in noninfected organs (Table 1).
Case reports of solid organ transplants from donors with Acinetobacter baumannii.
| Author | Year | Transplanted organ(s) | Clinical course | Management | Outcome |
|---|---|---|---|---|---|
| Cohen et al.8 | 2006 | 4 kidneys1 liver3 lungs2 heartsfrom donors with septic shock due to A. baumannii | A kidney transplant recipient had acute rejection that responded to treatment. | Meropenem | Except for one heart transplant (that failed due to primary graft failure), all were still alive on posttransplant day 60 |
| No patient had positive A. baumannii cultures | |||||
| Martins et al.9 | 2012 | Lung | Pneumonia with positive A. baumannii cultures on multiple occasions. | Amikacin and polymyxin B, as well as reduced immunosuppression | Died on posttransplant day 61 |
| Required amines, invasive ventilation and presented with kidney failure | |||||
| Sözen et al.5 | 2008 | Liver and 2 kidneys in different recipients | None in the three recipients | Teicoplanin, netromycin, and cefoperazone/sulbactam | No isolation in cultures in the three recipients |
| Liver and 2 kidneys (different recipients) | Not specified | Empiric antibiotic therapy | The cultures of the 3 recipients were negative | ||
| Bardossy et al.10 | 2020 | Lung | No clinical manifestations and/or infection. On day 12 alveolar lavage culture was positive for A. baumannii | Tigecycline IV for 19 days and colistin for 45 days | Graft colonized by A. baumannii up to 6 months after transplant but with no function alterations |
| Liver and 2 kidneys (different recipients) | Not specified | Empiric antibiotic therapy | The cultures of the 3 recipients were negative |
Nevertheless, Tong et al.6 described a cohort of patients that underwent liver transplantation. Eighty-two patients were infected, 12 (14.6%) of whom had donor-derived infections. Five of those patients were infected with A. baumannii and three of them died. Mularoni et al.7 described a series in which four out of 14 recipients of organs from donors with infection/colonization caused by resistant Gram-negative bacilli presented with transmission of said bacteria. Those four recipients had not received treatment against isolates in the donor. The rest of the recipients received at least seven days of adequate treatment in the immediate posttransplant period.
In a context in which the quantity of organ donors is precarious, it is important to take advantage of any opportunity that implies obtaining a graft for patients on the waiting list, which can include an infected donor. The presence of bacterial infections in the potential donor does not preclude liver donation. Effective treatment should be started in the donor, and possible infectious foci controlled (changing of central venous catheters, arterial lines, etc.). Communication with the procurement team should be established, so that effective antimicrobial treatment is administered to the recipient.
Ethical considerationsThe present scientific letter rigorously meets the ethical considerations required for bioethical research, was authorized by the corresponding ethics committee. Importantly, to protect patient privacy, informed consent was not obtained, given that no personal information that could identify the patient was included in the content of the article.
Financial disclosureNo financial support was received in relation to this article.
Conflict of interestThe authors declare that there is no conflict of interest.
Please cite this article as: García-Carrera CJ, Rivera-Lopez FE, Papacristofilou-Riebeling B, Fernández-García OA, García-Juárez I. Trasplante hepático de un donador con infección por Acinetobacter baumannii multidrogorresistente. ¿Representa un riesgo? Rev Gastroenterol Mex. 2023;88:436–439.